Introduction: Recently, a new role of vitamin D and PTH interaction in muscle performance has been demonstrated, however, whether this interaction also plays a role in physical performance after exercise remains unknown.
Method: The study evaluated the serum levels of vitamin D and PTH, as well as the physical performance of 345 older women aged ≥ 60 years of age, practicing aquatic training (AT) and multifunctional fitness (MF), before and after one year of vitamin D supplementation (21,000 IU/week). Physical performance tests: Timed up-and-go (TUG), arm curl (AC), unipedal balance test with visual control (UB), and the 2-min step test (2MST).
Results: There was an effective and predominantly physical activity-dependent increase on vitamin D levels in all supplemented groups as well as decreased values of PTH. In addition, PTH showed a positive correlation with TUG test, and a negative correlation with the 2MST.
Conclusion: The interplay between vitamin D, PTH and appropriated physical activity results in a better physical performance in older women.
Physical performance, Vitamin D, Older Women, Parathyroid Hormone
During the last two decades a large amount of literature supports that the role of vitamin D extends far beyond the skeleton. The discovery of vitamin D receptor (VDR) has provided more insight on its additional functions [1]. VDR are present on many organs, such as the pancreas, large and small intestine, muscle, and nervous system [2]. Vitamin D was found to regulate the cell cycle and subsequently influence organ functions by binding to its receptor in the cells of the immune, nervous, and cardiovascular systems [3].
In bone, the vitamin D deficiency and the elevation in PTH leads to cortical thinning, and in some cases, marrow fibrosis [4]; effects that have been mostly associated to high levels of PTH. PTH plays diverse roles in the body from maintaining whole body calcium homeostasis to maintaining bone density. PTH affects all bone cells; stimulation of osteoblasts enhances bone formation while stimulation of osteoclast maturation increases bone resorption. PTH interacts directly with osteoblasts and osteocytes through PTH1R to trigger a number of different pathways including cAMP/PKA, PLC/PKC, β-arrestin translocation, and ERK1/2. PTH is also the key molecule responsible for the 25 vitamin D 1α-hydroxylase activation, forming active vitamin D that modulates calcium reabsorption in the intestine [5]. The osteoanabolic effect of PTH on bone has been successfully and effectively used pharmacologically to treat bone disorders.
In muscle, vitamin D and PTH have been found to exert important effects including anabolism, regulation of muscle metabolism and maintanence of calcium homeostasis. Low levels of vitamin D and high levels of PTH have been associated with sarcopenia [6,7]. However, the effect of vitamin D supplementation and changes in serum PTH on muscle function either alone or combined with physical exercise remains uknown.
In the present study, we evaluated the physical performance of older women practicing aquatic training and multifunctional fitness before and after vitamin D supplementation, as well as the correlation between serum PTH, and vitamin D and their levels of physical function. We hypothesized that PTH plays an important role in the response of the muscle to a combination of vitamin D supplementation and that this interaction is also dependent on the physical activity type.
The study was performed in accordance with the Declaration of Helsinki, and it was approved by the Ethics Committee of the Federal University of the São Paulo/UNIFESP. All subjects voluntarily signed a consent form prior to beginning the study.
The research started with 458 older women aged ≥ 60 years. However, for a variety of reasons such as missing the second phase of the study or inapropriate use of vitamin D supplementation, 113 (24.6%) of subjects abandoned the programs during the 12 months of intervention. The final number of women who completed the study were 345.
The subjects were divided into three groups: 1) AT: Individuals participating in the aquatic training program (n = 146); 2) MF: Individuals participating in the multifunctional fitness program (n = 99) at the Social Service of Commerce (SESC), São Paulo, Brazil; with all participants from these groups performing physical activity for at least one year in the same program; and 3) Control group (CT), composed of 100 community-dwelling older women from community centers providing services to older persons living in the same geographic area, who had not been performing any regular physical exercise for at least one year. The CT group did not receive any information about vitamin D supplementation or regarding physical exercises. The participants were excluded if they were receiving hormonal treatment, were on medication for weight loss, were receiving vitamin D supplementation of > 600 IU/day, and/or had a creatinine level of > 1.5 mg/ dL. In addition, they shouldn't have a total calcium level of > 10.5 mg/dL, psychiatric disorder, and/or acute illness that would prevent them from exercising or following the protocol. The use of antihypertensive, antidiabetic, and lipid lowering medications was continued during the protocol, according to the medical prescriptions.
To evaluate the physical activity levels of the participants, a short version of the International Physical Activity Questionnaire (IPAQ) was used [8]. The aquatic training supplemented group (ATSG) and multifunctional fitness supplemented group (MFSG) were classified by IPAQ as irregularly active, i.e., meeting at least one of the criteria of recommendation regarding the frequency or duration of physical activity: 5 days/week or 150 min/week. The control group was classified as sedentary (SSG) [9].
A maximum of three absences per month were allowed in the physical exercise programs, the participants who exceeded this number were excluded from the programs. The participants were supervised by the same physical education instructor, twice a week. The activities were performed indoors, for one year, at the same place.
The aquatic training and multifunctional fitness sessions lasted 60 min, starting with 10-min warm-up exercises, followed by cardiorespiratory training, coordination exercises, strength and resistance exercises. The sessions ended with 10 min of stretching and balance exercises.
An intervention study design protocol has been followed. Due the lack of consensus in the literature regarding the vitamin D level cutoffs for performance evaluation during the study period (2010-2011), the median of the serum 25 (OH)D levels of all participants were considered to define the supplemented group (S) and the non-supplemented control group (NS). So, the participants in each group (AT, MF, and CT) with serum levels of 25(OH)D below the median, 17.6 ng/mL for ATSG, 18.50 ng/mL for MFSG, and 14.60 ng/mL for SSG received cholecalciferol supplementation.
According to the Endocrine Society's practice guidelines on vitamin D, vitamin D levels were defined as 25(OH) D: Deficiency, < 20 ng/mL; Insufficiency, 21-29 ng/mL; and Sufficiency, ≥ 30 ng/mL [2].
Two months before the beginning the supplementation protocol, participants were instructed to discontinue the use of any vitamin D supplements in order to maintain the baseline levels. The supplemented group received 21,000 IU/week of vitamin D3 for 12 months. All participants were advised to take the supplement in the prescribed dose once a week (4 drops/week). To improve adherence to treatment, participants received a calendar where the suggested dates for taking the supplement had been highlighted.
The vitamin D supplements were obtained at Magister® Pharmacy of Manipulation LTDA., São Paulo, SP, Brazil. The content of the cholecalciferol drops (5246 ± 20 IU/drop) was checked at the AFIP Laboratory for quality assurance in 17.5% of the sample.
Regarding calcium supplementation, although the University geriatrics outpatient service routinely prescribed at least 500 mg of calcium carbonate during the follow-up period, calcium supplementation was not part of our protocol. Participants were instructed to continue their usual diets, from which they ingested approximately 387 (294-513) mg/day of calcium [10].
Blood samples were collected after 12 h of fasting. All participants had their first blood sample collected in August 2010 and their second blood sample collected in October and November 2011. The serum concentration of 25(OH)D was determined by chemiluminescence using the LIAISON® 25 OH vitamin D Total Assay (Product code: 310600; DiaSorin Inc., USA), with intra-assay and inter-assay coefficients of 1.6% and 5.6%, respectively.
The intact PTH was determined by a chemiluminescence method (Elecsys® 2010, Roche Diagnostics, USA), with intra- and inter-assay coefficients of 3.0% and 3.5%, respectively. Total calcium was analyzed by an enzymatic colorimetric method (II Selectra Merck).
Timed up-and-go test (TUG): The participants were timed as they got up from a chair, walked 10 feet, without running, turned back, returned, and sat down again. The performances of two tests was measured at the baseline, and the final result was the mean of the two trials [11].
The arm curl test (AC): Measured upper-body muscle function and was assessed by the number of arm curl repetitions performed with a 2 kg dumbbells for 30 seconds [12].
Unipedal balance test with visual control (UB): In a standing position, the subject had to flex one of her legs in a 90° for 30 s. Three attempts were made, and the average value was recorded [13].
The 2-min step test (2MST): The number of full steps completed in 2 min while raising a knee to midway between the patella and iliac crest was measured. The result was presented as the number of times the right knee reached the target [14].
Statistical analysis was performed using the SPSS statistics software (version 19.0 for Windows). According to the G*Power software and based on expected observed power of 80% and an effect size of 49% (based in our previous results in a pilot study), in the TUG test score, the sample included 432 individuals (72 individuals in each group).
For groups characterization, we performed a descriptive analysis (mean ± standard deviation). The methodology was based on the median value for the 50% for vitamin D. The data variation percent before (time = 0) and after vitamin D supplementation with their respective standard deviation. The comparison between the groups of the percentages of the tests mentioned above was performed by the univariate GLM test, covariate by the percentage difference of the fraction: PTH by the percentage difference of vitamin D.
Pearson correlations were used to first analyze the data. From the significant data, linear regression and a logistic regression model was established in order to establish the effect of vitamin D supplementation between the groups on the other variables analyzed.
Figure 1 shows the effectiveness of vitamin D supplementation in all evaluated groups. To note, even before supplementation, the MF group already presented higher levels of vitamin D when compared to AT or CT groups. As expected, a negative correlation between vitamin D and PTH levels (Figure 1 and Figure 2) was observed [15,16].
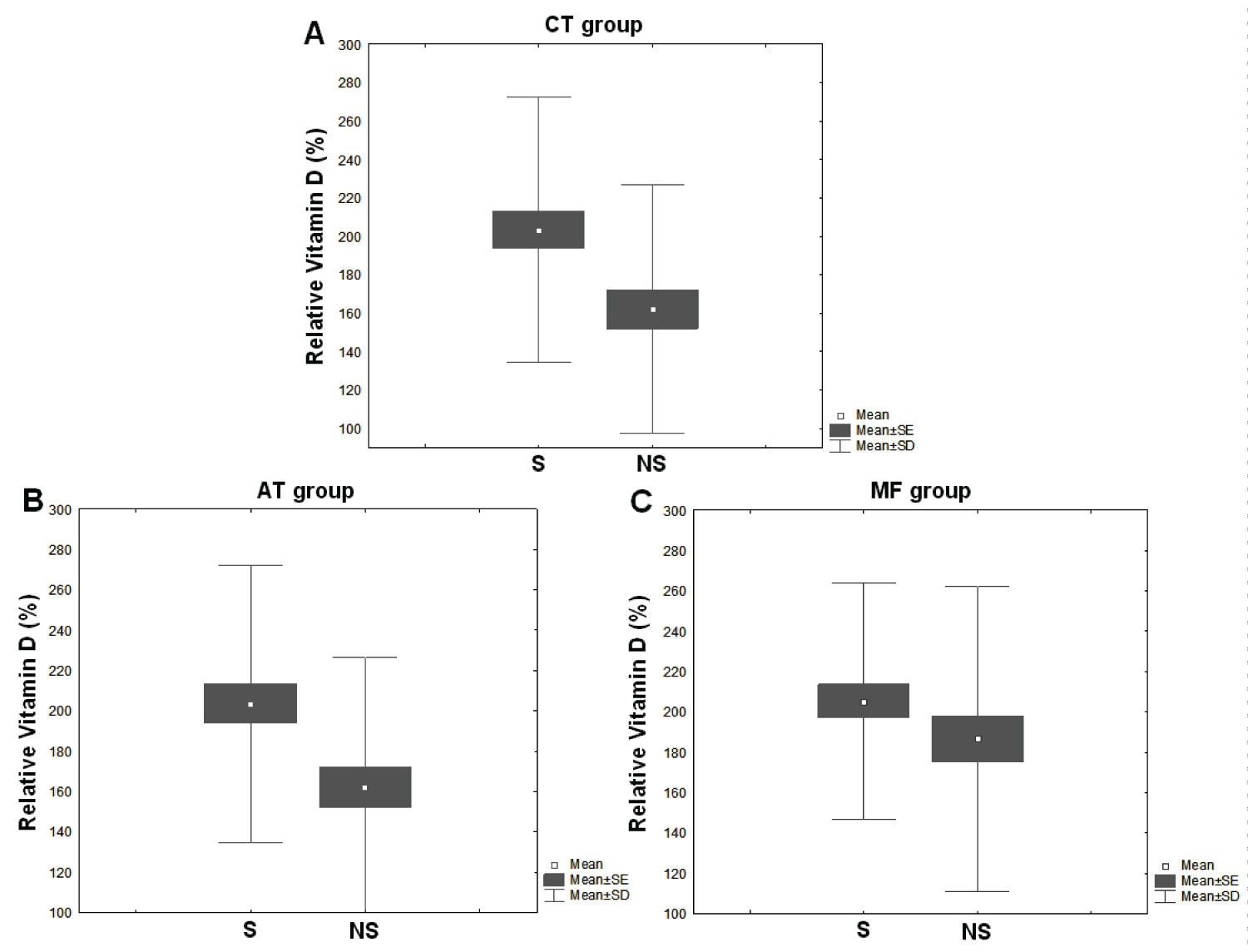 Figure 1: The effectiveness of vitamin D supplementation in all evaluated groups. View Figure 1
Figure 1: The effectiveness of vitamin D supplementation in all evaluated groups. View Figure 1
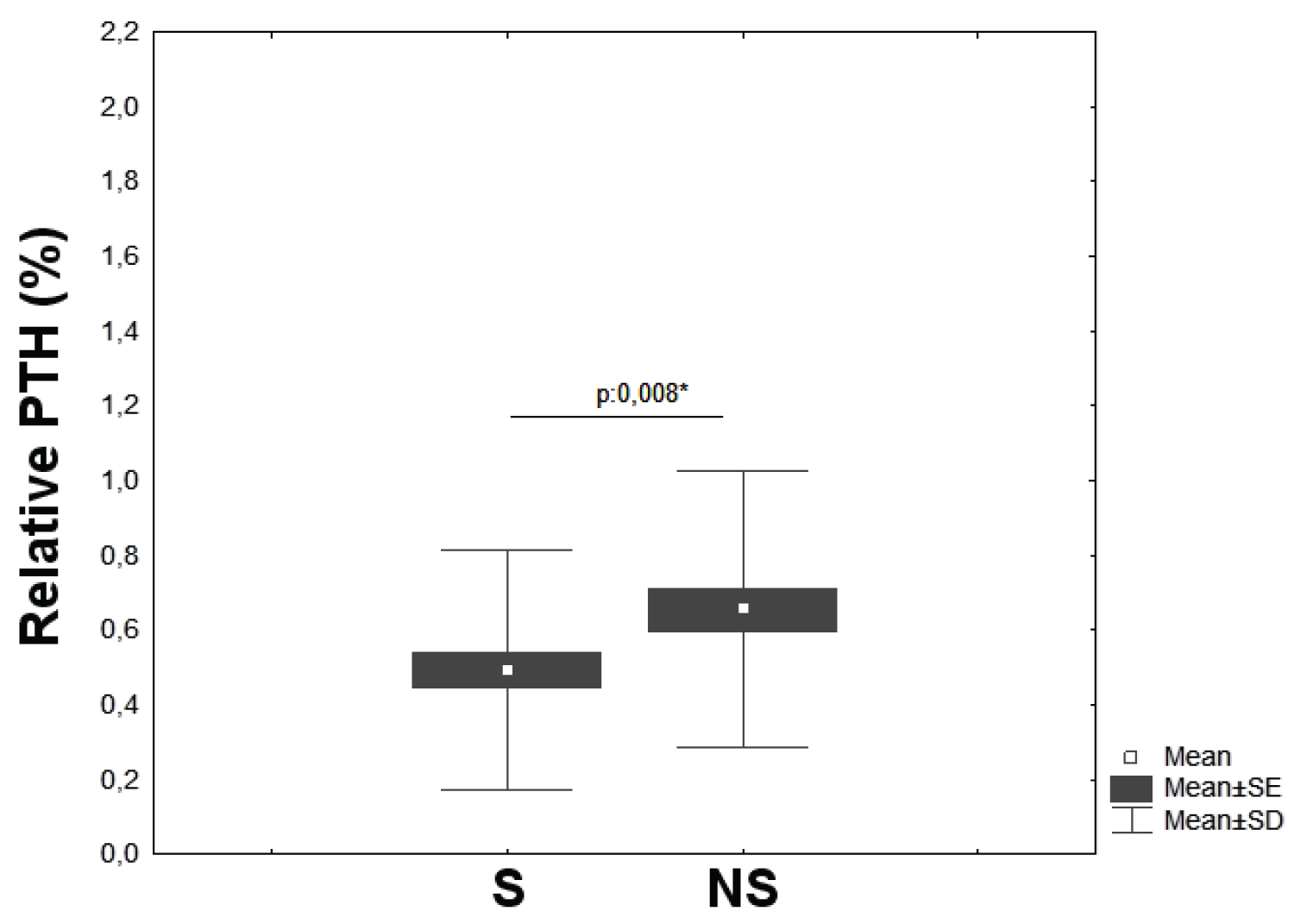 Figure 2: Correlation between vitamin D and PTH levels. View Figure 2
Figure 2: Correlation between vitamin D and PTH levels. View Figure 2
Table 1: Anthropometric measurements and clinical data in pre- and post-treatment in all groups. View Table 1
Regarding physical performance, the Figure 3 shows the TUG test results in the non-supplemented (Figure 3A) and supplemented (Figure 3B) groups. The results show an improvement in the performance of the supplemented older women, especially in the group that does not practice physical activity (CT). It is also possible to note that the MF group showed a considerable adjustment in the group performance, showed by the results concentration close to the average and, consequently, reduction of the sample standard deviation. Interestingly, the panel C shows a positive correlation between PTH levels and the TUG test performance (Figure 3A, 3B and 3C).
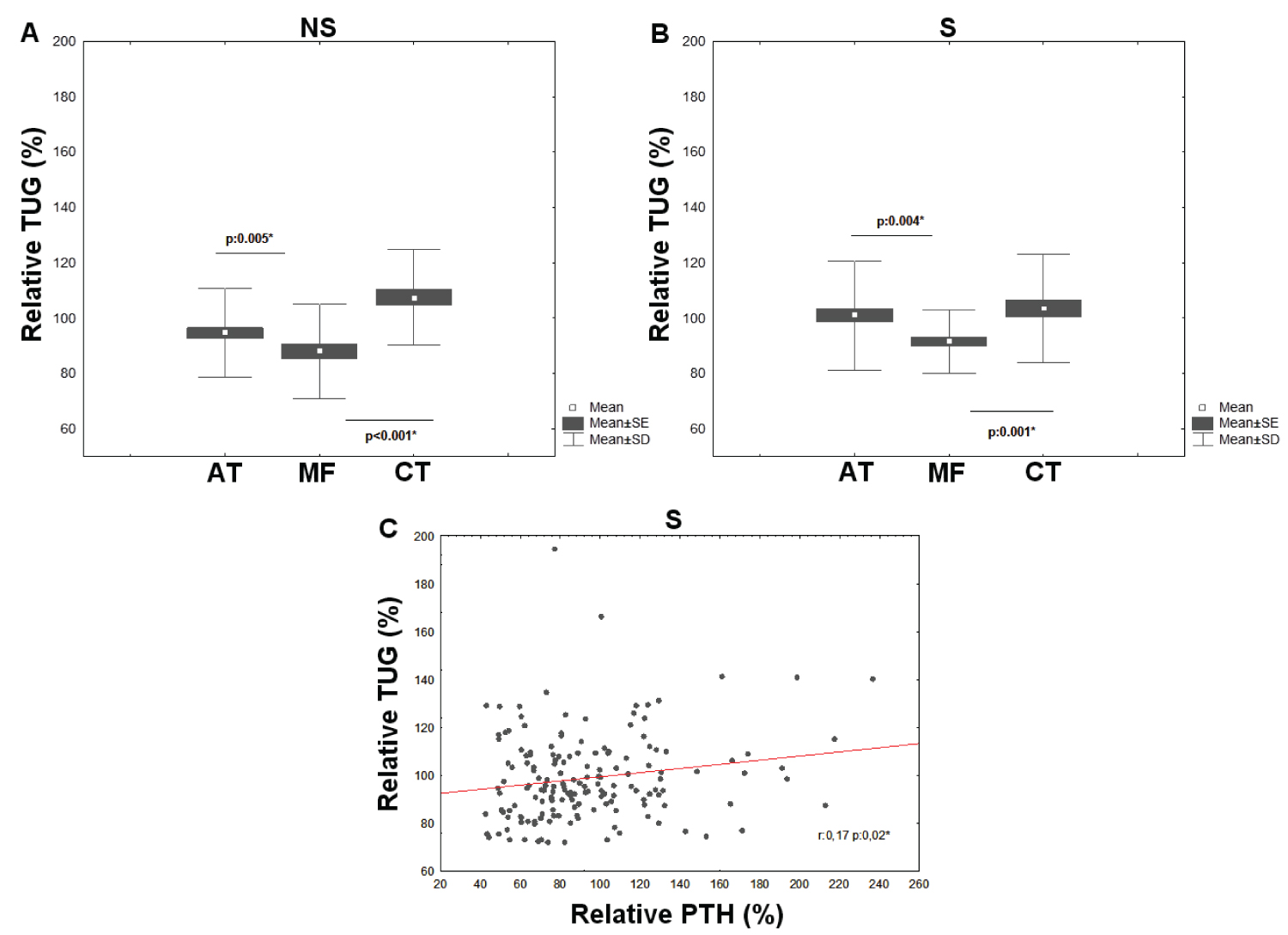 Figure 3: The TUG test results in the non-supplemented (A) and supplemented (B) groups, and a positive correlation between PTH levels and the TUG test performance (C). View Figure 3
Figure 3: The TUG test results in the non-supplemented (A) and supplemented (B) groups, and a positive correlation between PTH levels and the TUG test performance (C). View Figure 3
Figure 4 shows that, despite the statistical differences within the non-supplemented (Figure 4A) and supplemented (Figure 4B) groups, the results for the arm curl test do not correlate with serum vitamin D levels, since both the AT and the MF groups had, proportionally, the same evolution in this test. It is important to note that the CT group showed no increase in performance in any of the situations (NS or S) (Figure 4A and 4B).
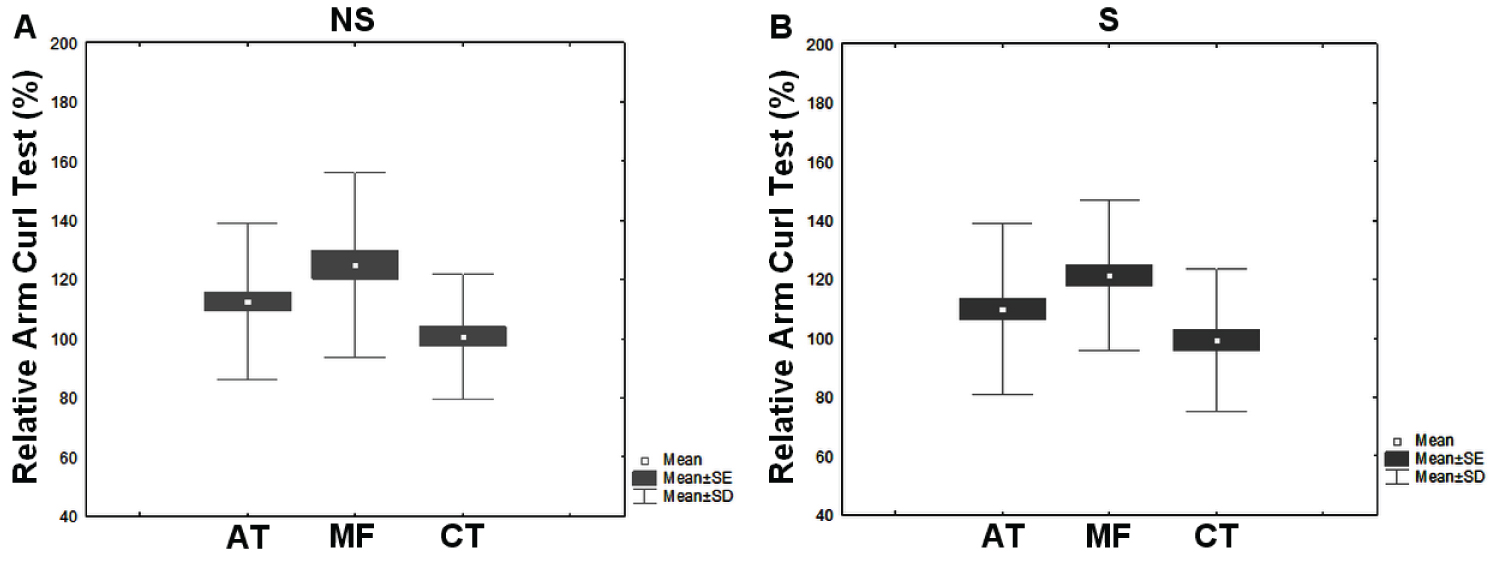 Figure 4: The statistical differences within the non-supplemented (A) and supplemented (B) groups. View Figure 4
Figure 4: The statistical differences within the non-supplemented (A) and supplemented (B) groups. View Figure 4
The unipedal balance test, presented in the Figure 5, confirms the relationship between balance and vitamin D levels. Again, the improvement in performance was more evident in the MT group when compared to the AT group. The CT group shows that only supplementation without physical activity is not enough to improve performance (Figure 5A and 5B).
 Figure 5: The relationship between Unipedal Balance Test and vitamin D levels. View Figure 5
Figure 5: The relationship between Unipedal Balance Test and vitamin D levels. View Figure 5
The results obtained in the 2 min step test-2MST (Figure 6A and Figure 6B) show the efficacy of supplementation mainly in the MF group, despite a slight improvement in the AT group. However, the decrease the CT group performance demonstrates the importance of maintaining a physical activity program. Interestingly, the statistical analysis of the data showed that the performance in the 2MST has a negative correlation with the PTH levels (Figure 6) in the evaluated elderly women.
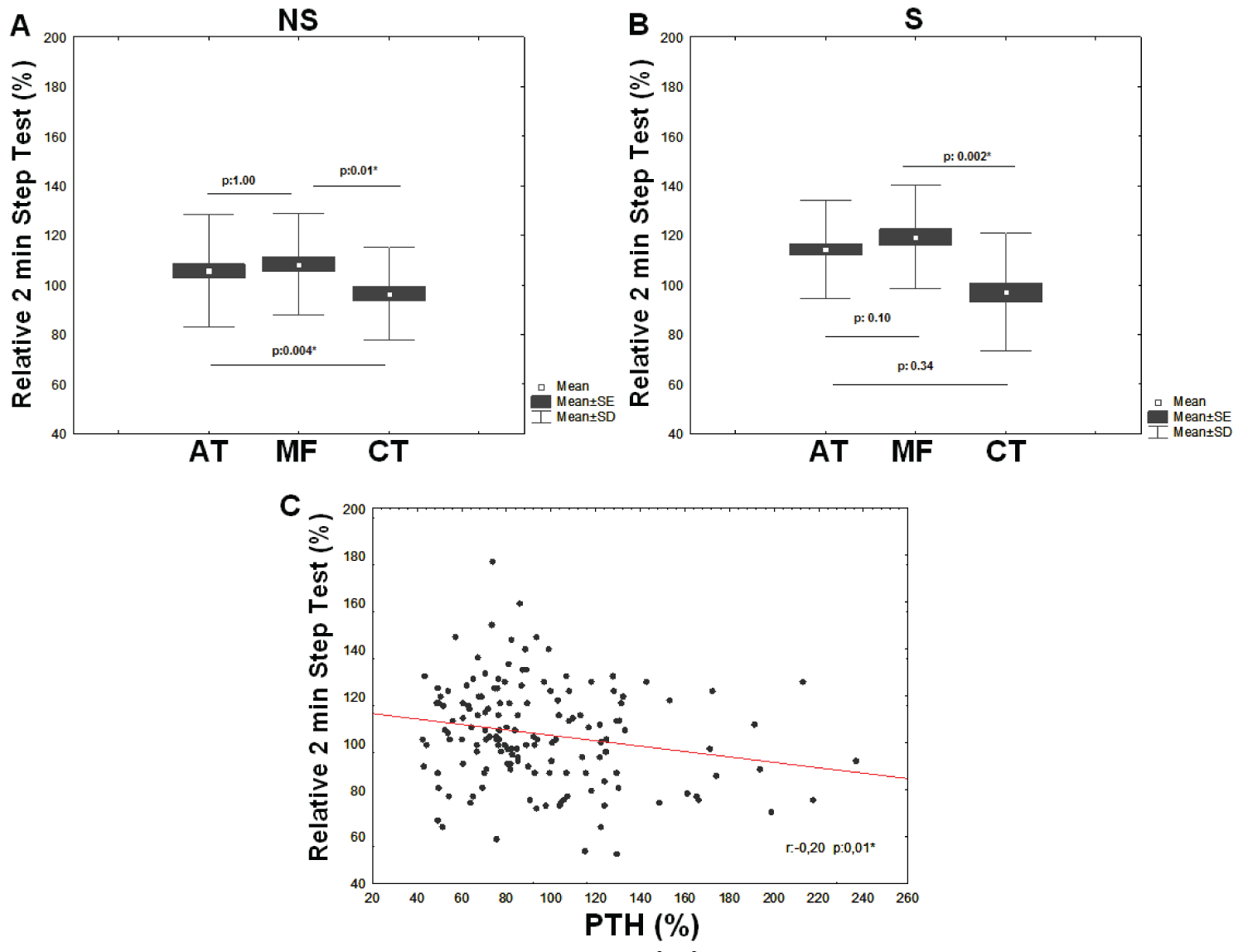 Figure 6: The results obtained in the 2 min step test - 2MST (A and B) and a negative correlation with the PTH levels in the evaluated of the older women (C). View Figure 6
Figure 6: The results obtained in the 2 min step test - 2MST (A and B) and a negative correlation with the PTH levels in the evaluated of the older women (C). View Figure 6
This study showed that in vitamin D deficient older women, 25(OH)D supplementation improved their overall physical performance as well as their response to physical exercise.
Trying to establish correlations between performance in different sort of physical activities and serum levels of vitamin D and PTH is always challenging. In a previous study of our group we showed that even older women living in tropical regions have, in the majority, insufficient serum levels of 25(OH)D [17]. In the present study 166 older women were vitamin D supplemented for 12 months and evaluated in relation to physical performance before and after supplementation while practing AT or MT.
A study conducted by Brock K et al. demonstrated that skeletal muscle has a role in maintaining the long residence time of vitamin D in blood and, still, that there is a positive relationship between the intensity of physical exercise in older adults [18], and the level of vitamin D in blood [6,7]. This may explain our findings where the MF group, known as a more effective exercise than AT, showed higher vitamin D levels even when the participants were not supplemented.
PTH (and PTH1R) has been related to play a role in skeletal muscle fiber differentiation by increasing the rate of myocyte regeneration [19]. These finds may explain the association between PTH and physical performance in older women found in our study. In a previous study from de França, et al. [20], PTH levels has been related with poor balance in older persons. However, the present study shows for the first time that PTH has positive correlation with TUG test, and a negative correlation with the 2 minutes step test.
Our study also shows that PTH plays an important role in the physical performance of older women, especially in maintaining dynamic balance, agility, reaction time (TUG), lower limb strength and cardio respiratory capacity (2MST). Furthermore, our data also suggest that the intensity of physical activity plays a fundamental role in maintaining the characteristics mentioned above.
This study has limitations. There was no randomization, because the intervention was implemented in groups that were already involved in the exercise modalities for at least one year. We did not evaluate the factors that influenced serum vitamin D levels during the study such as lifestyle, nutritional data, and sunlight exposure. We evaluated the supplementation of vitamin D in individuals following different modalities of physical exercises to test their physical performance, and therefore, this was not a blind study. The sample was confined to only one geographical area. The results are relevant to a community of physically independent older women.
Based on this evidence, it is possible to conclude that maintaining the practice of regular physical exercises program promotes an improvement in the skeletal muscle metabolism. Which in turn causes PTH to better control the time release of vitamin D into the bloodstream. As a consequence, this interplay between vitamin D, PTH and appropriated physical activity results in a better physical performance in older women, preventing primarily falls in these persons.
The authors declare no potential conflict of interest with respect to the authorship and/or publication of this manuscript.
This study was supported by FAPESP (Fundação de Amparo à Pesquisa do Estado de São Paulo; Grant no. 09/53658-8). Thanks to the Social Service of Commerce for the opportunity to perform most of the study in its facilities.