Background: Hip fractures are common among the elderly, due to lack of mobility, osteopenia and hypocalcaemia. Surgery for repairing a fracture in the femoral neck within 48 hours improves the clinical outcome.
Objective: To measure the performance rate of hip fracture repair within 48 hours of admission, and the effect on mortality.
Methods: The data were obtained from the Israeli National Program for Quality Indicators. The denominator included all the patients 65-year-old or older who was admitted and operated because of hip fracture, and the numerator included those who underwent surgical repair within 48 hours of admission.
Results: There has been a significant improvement in the national level of compliance within 48 hour time span- from 71% in 2013 to 87% in 2018. The success rate for total hip replacement (THR) was 53%, 68%, 74%, 81%, 79% and 78%, for partial hip replacement (PHR) the success rate was 66%, 76%, 80%, 82%, 84%, and 86%, and for fixation it was 74%, 80%, 85%, 89%, 89% and 89%, for 2013, 2014, 2015, 2016, 2017 and 2018, respectively.
The mortality rate within 30 days of the admission was 4% in patients who underwent hip fracture repair within 48 hours of the admission, and 6.1% in the patients who did not, respectively, with odds ratio (OR) of 0.645, 95% CI 0.573-0.726, P < 0.0001.
Conclusions: We could demonstrate a significant decrease in mortality of patients with hip fracture who underwent hip fracture repair within 48 hours of admission.
Quality, Indicators, National program, Hip fracture, THR
• Surgical hip fracture repair was performed within 48 hours of admission in 71%, 78%, 83%, 86%, 86% and 87% of the patients in 2013, 2014, 2015, 2016, 2017 and 2018, respectively.
• Seventeen hospitals out of 26 (65.38%) achieved the target of 85% in 2018.
• The mortality rate within 30 days from diagnosis was lower in patients who underwent hip fracture repair within 48 hours of the admission, odds ratio (OR) of 0.645, 95% CI 0.573-0.726, P < 0.0001.
The National Program for Quality Indicators (NPQI) of the Israeli Ministry of Health goal is to promote quality and safety of health care by a process of measuring the quality of care and publicizing the results to the public. Following seven years of activity, we conclude that there is a significant improvement in most quality indicators that were measured over the years. A Business Intelligence (BI) System enables access to the data and segmentation of the results by various characteristics, for the benefit of the service providers and the population.
Femoral neck fractures are common among the elderly, due to lack of mobility, osteopenia and hypocalcaemia, which can lead to numerous health risks, including secondary illness and mortality. Often after an initial hip fracture, a person cannot continue being independent and must undergo drastic lifestyle changes. Women suffer from hip fractures more than men due to their more rapid decrease of bone density [1]. In addition, the risk of incurring a hip fracture increases with age, with females aged 85+ at the highest risk level for a fracture [2]. Hip fractures are considered to be one of the most expensive burdens for the health system [3]. Overall, the total direct costs of hip fractures in the elderly population in Israel in 2013 was 719 million NIS, including hospitalization, rehabilitation and nursing care, with the majority of costs incurred during the first year after the event [4].
Surgery for repairing a fracture in the femoral neck within 48 hours improves the clinical outcomes of the patient. Delay of surgery beyond the 48-hour window raises the rate of mortality within 30 days by 41% and within a year by 32% [5]. Conversely, early surgery within 24-48 hours after admission lowers the rate of complications, including pulmonary embolism, acute coronary syndrome and renal failure [6,7]. Rationalized by these evidences, since its establishment in 2013, NPQI has set an indicator for performing surgical hip fracture repair with 48 hours of admission.
It should be emphasized that the purpose of NPQI is not to reach the maximum level of compliance possible. The relevant population of patients with hip fracture includes patients with complex medical conditions that prohibit performing operation within 48 hours, at least until the time that these patients are stabilized. As such, the percentage of compliance with the indicator at the hospital will be adjusted accordingly. The goal of compliance with this indicator has been set nationally at 85%. This allows some freedom for clinical decisions made by the staff for the benefit of the patients and according to their medical needs.
The indicator was set as surgical repair of hip fracture within 48 hours of admission. The denominator included patients who were admitted because of hip fracture, and the numerator included those who underwent its surgical repair within 48 hours of admission. Inclusion criteria included all the patients 65-year-old or older who were admitted and operated because of hip fractures according to the ICD9 codes. There was no target for the first year of measuring (2013). The target was 60%, 70%, 75%, 80% and 85% for 2014, 2015, 2016, 2017 and 2018 respectively.
Data computed for each case was age, gender, date and time of hospitalization, date of discharge, date of birth, date of death, and date and time of surgery.
Performance was reported every three months to a dedicate server ("safe") of the INPQ. Data was examined for accuracy by independent observers before acceptance to the server. Then, senior nurses and investigators validated a statistically significant sample of the reports, and when approved, referred the results for statistical evaluation and final approval.
Hospitals were compared every 3 months according to the indicator's results, and annual national achievements were computed. Indicator's target was increased every year according to the achievements. Once a year the results were published in the media and presented at the Ministry of Health Quality and Safety annual meeting.
We looked at changes along time in the indicator achievements, and the 30 days mortality rate of the patients who underwent hip fracture repair within 48 hours of admission compared to those who did not. It is clear that the selection of patients for early operation is not random, and dependent of the patient clinical status and background diseases. To neutralize these parameters we performed a logistic regression model first taking into account age and gender and then adding Charlson severity score. The gender was defined as a categorical parameter of 5 years groups (65-69, 70-74, 75-79, 80-84, 85-89, 90-94, 95 and older).
In 6 years, 2013-2018, 36515 patients were hospitalized because of hip fracture, an average of 6085 patients a year. There has been a significant improvement at the national level for compliance of performing surgery within 48 hours since admission-from 71% in 2013 to 87% in 2018 (Figure 1). The success rate for total hip replacement (THR) was 53%, 68%, 74%, 81%, 79% and 78% for 2013, 2014, 2015, 2016, 2017, and 2018, respectively. For partial hip replacement (PHR) the success rate was 66%, 76%, 80%, 82%, 84%, and 86% for 2013, 2014, 2015, 2016, 2017, and 2018, respectively, and for fixation it was 74%, 80%, 85%, 89%, 89% and 89% for 2013, 2014, 2015, 2016, 2017 and 2018, respectively. In 2018 the target compliance was achieved in 88% of 65-84 year-old patients and 86% of patients 85-year-old or older. For men and women the success-rate was 85% and 88%, respectively.
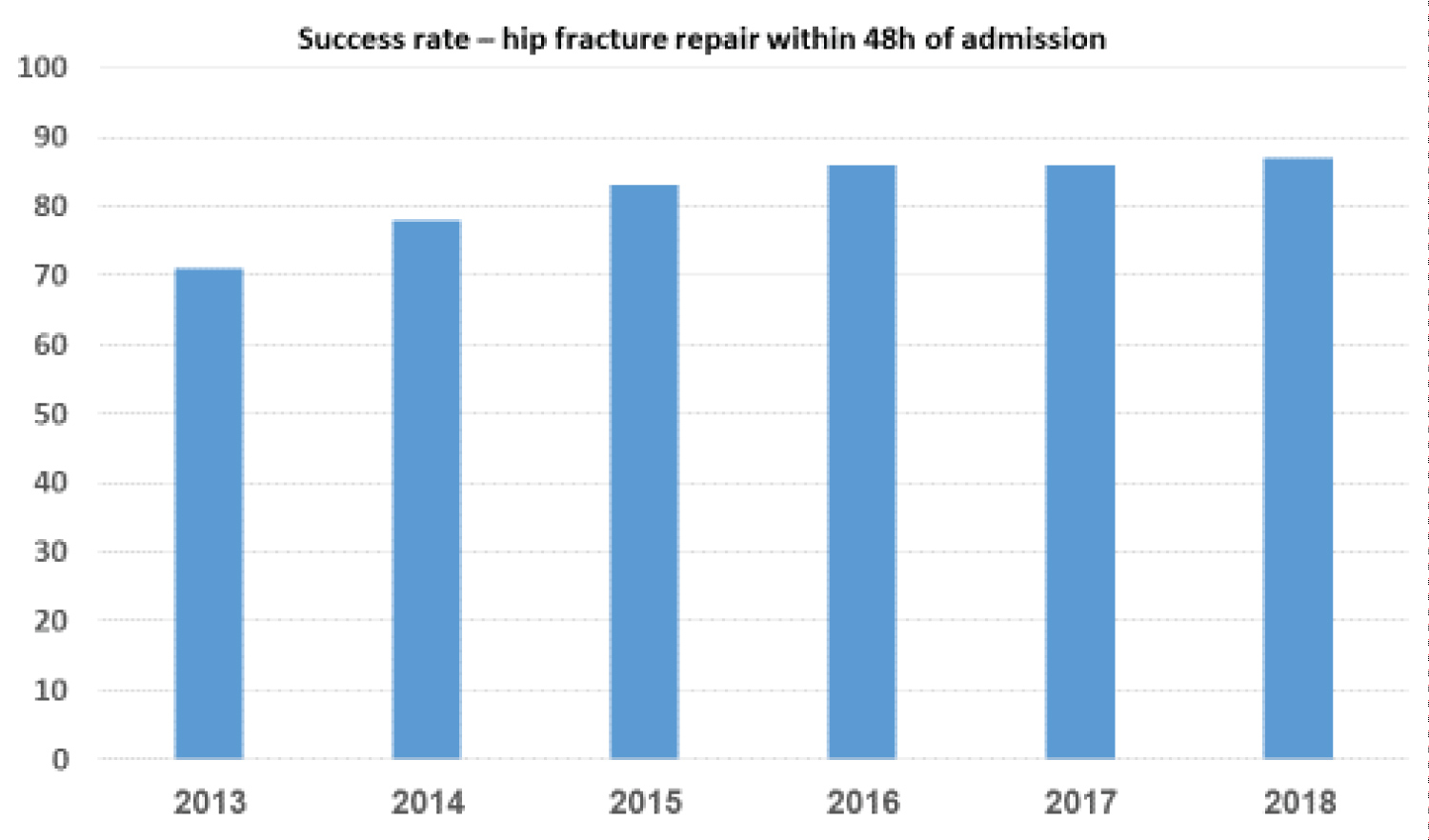 Figure 1: National level of success rate in hip fracture repair within 48h of admission.
View Figure 1
Figure 1: National level of success rate in hip fracture repair within 48h of admission.
View Figure 1
The mortality rate within 30 days of the admission was 4% in patients who underwent hip fracture repair within 48 hours of the admission, and 6.1% in the patients who did not, respectively, with odds ratio (OR) of 0.645, 95% CI 0.573-0.726, P < 0.0001. Lower mortality rate for patients who successfully underwent hip fracture repair within 48 hours was observed every year since 2013 (Figure 2).
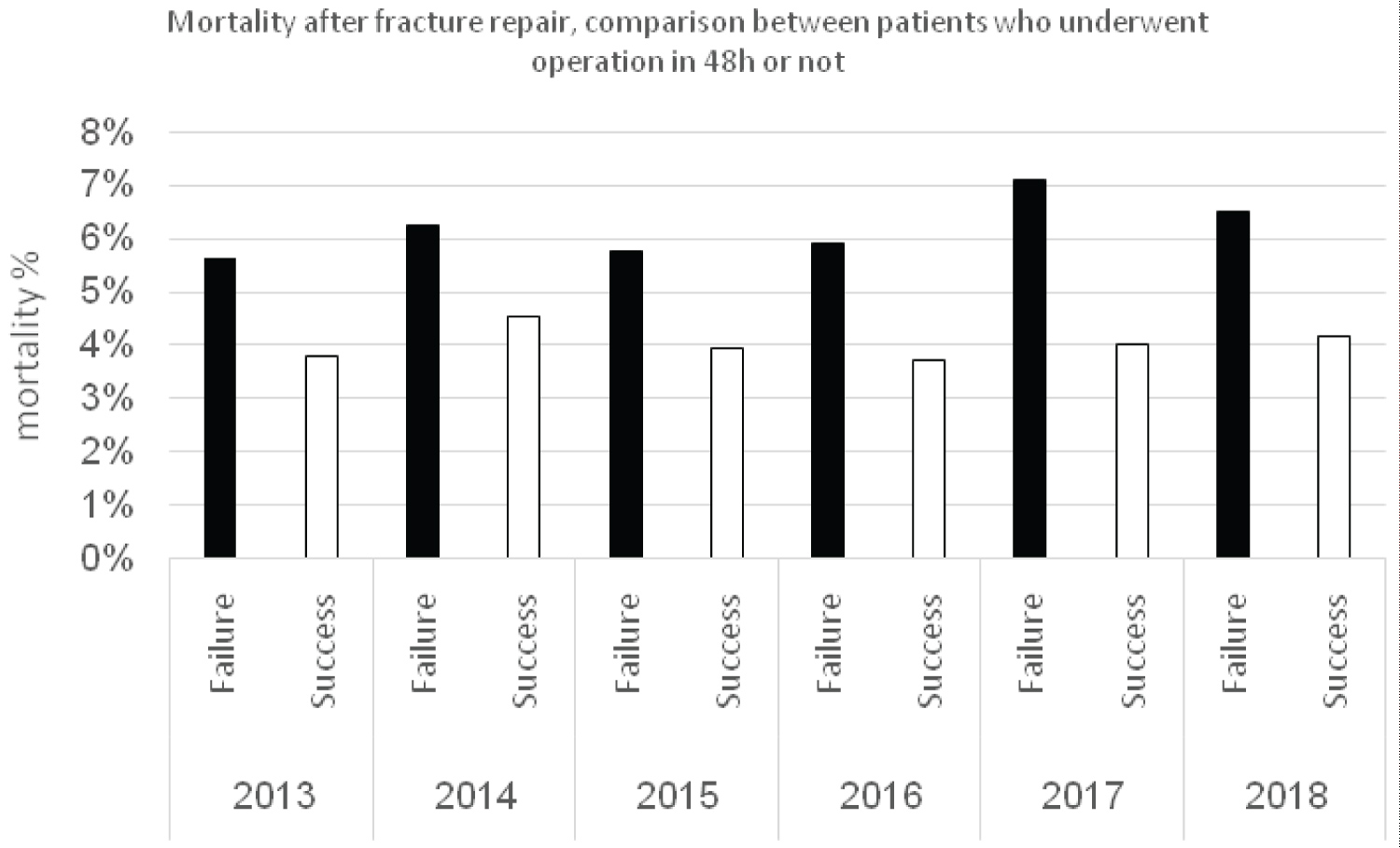 Figure 2: Comparison of mortality rate between patients who underwent hip fracture repair within 48h or not.
View Figure 2
Figure 2: Comparison of mortality rate between patients who underwent hip fracture repair within 48h or not.
View Figure 2
As expected death rate of men was higher than of women, and increased in older age group. Yet, OR for operation within 48 hours in this model was similar to that found without correction for age and gender. Adding Charlson severity score to the regression analysis changed the OR from 0.645 to 0.779, but sill the decrease in mortality remained significant (Table 1).
Table 1: A logistic regression model. View Table 1
Within 6 years, we achieved a significant increase in performance rate of surgical hip fracture repair, THR, PHR or fixation, within 48 hours of admission, from 71% to 87%, even though the target of the indicator was raised from 60% in 2014 to 85% in 2018. In addition, a significant lower 30-day mortality was observed, from 6.1% in patients who did not underwent operation within 48 hours to 4% in patients who did.
In 2017, on average across OECD countries, over 80% of patients admitted for hip fracture underwent surgery within two days. This represents a modest increase of 2.7 percentage points (from 78.2% to 80.9%) since 2012. The biggest improvement was observed in Israel (from 68% to 87%) [8]. Targeted policies that effectively incentivize timely surgery following hip fracture admission could partly explain this result. Iceland, the Czech Republic, Portugal and Latvia reported a decline in the proportion over this period, suggesting a need for policy interventions.
Our study has limitation using an epidemiological approach to study clinical issues. We could not know the causes of mortality, nor establish a cause and effect between mortality and hip repair within 48 hours of admission. We excluded the possibility of background diseases as a cause for the higher mortality rates in patients who did not underwent operation within 48 hours of admission.
In summary, hip repair within 48 hours of admission due to fracture is strongly recommended by guidelines in USA and Europe and by the Israeli Ministry of Health. The experience of the INPQ supports this approach. We could demonstrate a significant decrease of mortality in patients with hip fracture who underwent operation for THR, PHR or fixation within 48 hours of admission.
The authors have no conflict of interest.
None.
Dr. Anat Ekka-Zohar and Prof. Ronnie Gamzu for establishment of the NPQI.