COVID-19, Geriatrics, Stroke, Ischemic CVA, SARS-CoV-2, Gerontology, Primary Care, COVID Pneumonitis, Chest CT
COVID-19 is typically a respiratory or lung infection however the SARS-CoV-2 virus has been found to cause blood clots leading to stroke. The World Stroke Organization reported a 5% risk for an ischemic stroke in the setting of COVID-19 [1]. Stroke can occur regardless of age, symptoms, or comorbidities. However, patients with COVID-19 who had strokes were likely to be older, hypertensive with elevated D-dimer levels, cardiac troponin I, N-terminal pro-brain natriuretic peptide (NT-proBNP), and interleukin-6 (IL-6) [1,2]. In addition, patients with traditional stroke risk factors such as diabetes, heart disease, atherosclerosis, atrial fibrillation and obesity are more likely to have their vasculature attacked by COVID-19 [3]. Three main mechanisms appear to be responsible for the occurrence of ischemic strokes in COVID-19: A hypercoagulable state, vasculitis, and cardiomyopathy [4,5]. Although hemorrhagic stroke is not the focus of this case study, it is possible that the affinity of the SARS-CoV-2 virus for Angiotensin-converting enzyme 2 (ACE2) receptors, which are expressed in arterial smooth muscle and endothelial cells in the brain, allows the virus to damage intracranial arteries, causing vessel wall rupture [6]. ACE2 receptors are also present in the vascular endothelium which may be a causative factor for thrombotic complications in ischemic stroke [7]. This case will illustrate the importance of early treatment of COVID-19 in patients with underlying Cardiac Disease and Hypertension in order to help prevent strokes further complicating management and increasing mortality and morbidity. In addition, other key diagnostic findings such as a Computed Tomography (CT) scan may lead to earlier diagnosis and treatment of COVID-19 that may decrease risk.
This case report highlights the clinical course and recovery of a Black female, ZD, that experienced COVID-19 and was hospitalized for ischemic stroke. Older patients especially those from ethnic and minority populations in the United States have been shown to have poorer outcomes when diagnosed with COVID-19. This in conjunction with comorbidities such as Hypertension, Diabetes Mellitus, cardiac disease, and obesity further contribute to poor outcomes. Early detection and treatment of COVID-19 in this subsection of patients has led to improved outcomes, less hospitalizations, and decreased mortality. Vigilance and additional diagnostic tools for early detection of COVID-19 in this population of patients may be necessary to improve outcomes.
ZD is a 72-year-old Black female who had a telemedicine visit with her family physician to report a high risk COVID-19 exposure and new onset fatigue. The patient's past medical history includes hypertension, hyperlipidemia, obesity, atrial fibrillation, 2019 ischemic cerebral vascular accident (CVA), vitamin D deficiency, and prediabetes. The patient had been followed by cardiology and her atrial fibrillation and hypertension were well controlled on medication including metoprolol tartrate 25 milligrams (mg) and diltiazem HCL ER 240 mg. She was noted to be adherent to all her medications prior to this illness.
At the initial telemedicine visit, a COVID Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) test was ordered following a high-risk exposure. The physician followed up with the patient two days later to give her a negative result. At this time the patient denied fever, chills, nausea, vomiting, diarrhea, body aches, chest pain, cough, and headache. Twenty-three days later she was again seen via telemedicine with complaints of fever, chills, cough, and body aches for the last four days. ZD denied nausea, vomiting, shortness of breath (SOB), and anosmia.
The patient was diagnosed with suspected pneumonia possibly secondary to COVID-19 given continued exposure to a family member working as a nurse in a COVID unit. A COVID RT-PCR and chest Computed Tomography (CT) were ordered and completed the same day (Figure 1). CT results were available within 24 hours and showed multiple ground glass opacities compatible with COVID-19. She was prescribed Levaquin 500 mg daily for 10 days along with Tessalon Perles for cough, ibuprofen and acetaminophen OTC for fever, and was encouraged to rest and hydrate. The second COVID-19 RT-PCR results were negative. Patient called for a follow up telemedicine visit the next day and reported worsening cough and fever. She admitted to not starting the antibiotics as she did not believe she had COVID-19 since her RT- PCR was negative. The patient requested another antibiotic prescription and after counseling on importance of adherence, she was prescribed amoxicillin/clavulanate 875 mg twice daily. She was also given TheraFlu, aspirin 325 mg daily, and vitamin C 500 mg plus zinc 220 mg daily to boost immunity. The patient started the medications however her medical condition deteriorated. She was seen in the emergency room four days later and was admitted with chest pain, cough, vomiting, and shortness of breath. A chest X-ray completed during hospitalization showed pneumonitis. A third COVID-19 RT-PCR was repeated at the hospital and results were negative. ZD was discharged after 24 hours and asked to continue medications prescribed by her primary care doctor. The day after discharge, the patient had a telemedicine visit with her primary care doctor and reported persistent cough, lower extremities edema, and pain in her ribs and back. She was advised to continue all her medications including her antihypertensive medications.
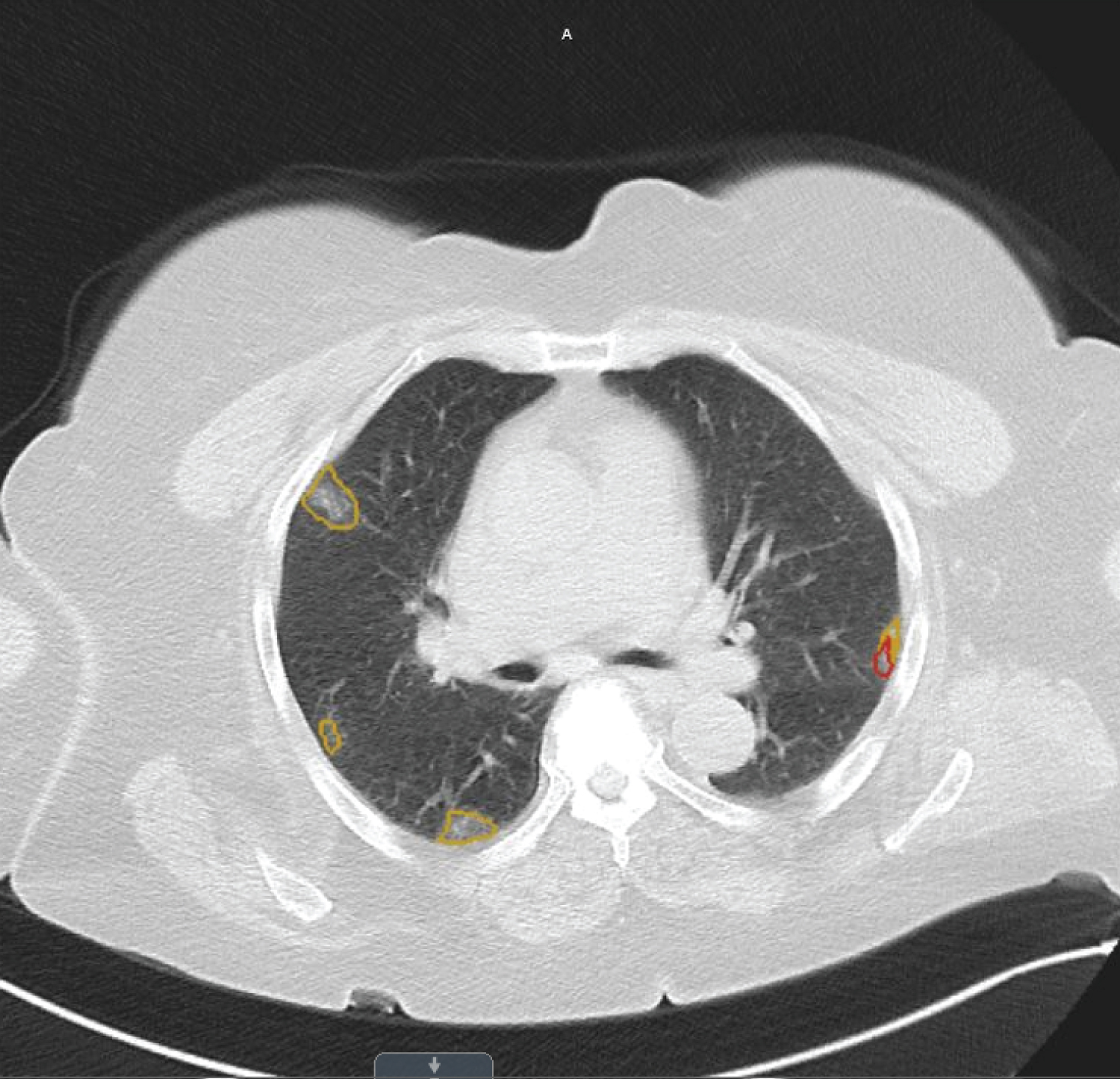 Figure 1: This is the chest CT completed on 5/18 on patient ZD. The ground glass opacities consistent with COVID-19 pneumonitis are circled in yellow and red throughout the lung field.
View Figure 1
Figure 1: This is the chest CT completed on 5/18 on patient ZD. The ground glass opacities consistent with COVID-19 pneumonitis are circled in yellow and red throughout the lung field.
View Figure 1
ZD's daughter reported the patient's condition did not improve and she was taken back to the emergency room 5 days later with sudden onset aphasia, right facial droop, and right sided weakness. She was emergently evaluated by neurology, and she was started on a tissue plasminogen activator (tPa) infusion, and admitted to the intensive care unit (ICU). Per hospital protocol, two troponin levels were drawn and both results came back normal. An echocardiogram was completed and showed no significant valvular heart disease and normal left ventricular systolic function. An electrocardiogram (EKG) was not available from this hospitalization. The patient developed a fever, elevated D-dimer (24+), and leukocytosis was noted (white blood cells were 15+). The following labs were drawn to assess renal function: Creatinine: 0.76 mg/dL and Blood Urea Nitrogen: 8 mg/dL. The following labs were not obtained during this hospital stay: IL-6 level, fibrinogen, lymphocyte and neutrophil count, ferritin, or cardiac function. A fourth COVID-19 RT-PCR test was completed as well as blood and urine cultures. The urine culture was negative for Legionella antigen. Ceftriaxone and vancomycin were started empirically. The fourth COVID-19 RT-PCR test came back positive. Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the head and carotid arteries were completed and showed the patient had a large chronic appearing infarct involving the left temporal parietal cortex. Figure 2 presents the imaging of the patient's completed MRI. A chest X-ray was also completed and showed minimal sub segmental bibasilar atelectas is with improvement in the previously visualized patchy opacities. ZD was placed on enoxaparin 40 mg subcutaneously every 12 hours for anticoagulation therapy. Her antibiotics were changed to ceftriaxone and azithromycin, then Zosyn for broader coverage. Her white blood cells started trending downwards and she became afebrile. She was transferred to the medical floor and her symptoms continued to improve. ZD was evaluated by Speech Therapy and advanced to a regular diet. The antibiotic was changed again to Levaquin 500 mg for 3 days and then discontinued.
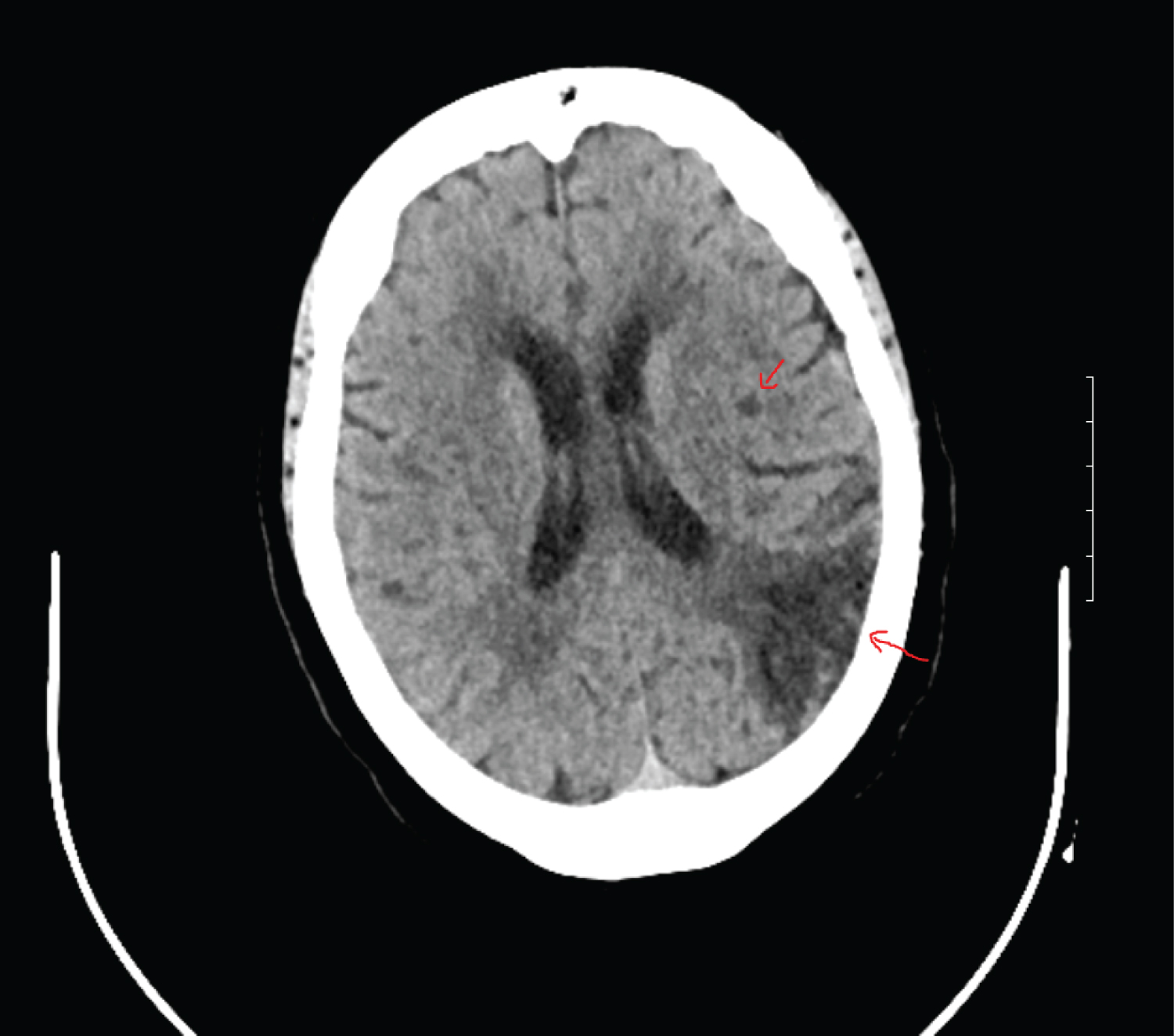 Figure 2: This MRI of the brain shows evidence of hypo-attenuation in the left posterior centrum ovale without any associated ex vacuo dilation of the left lateral ventricle which is indicative of a recent infarct.
View Figure 2
Figure 2: This MRI of the brain shows evidence of hypo-attenuation in the left posterior centrum ovale without any associated ex vacuo dilation of the left lateral ventricle which is indicative of a recent infarct.
View Figure 2
ZD was discharged home 4 days after her admission with home care services. She was placed on enoxaparin 40 mg subcutaneously every12 hours for 4 days and continued on her prescribed antihypertensive medications. Home skilled nursing, physical therapy (PT), occupational therapy (OT), and speech therapy were initiated through a home health agency and focused on speech and communication, gait training, conditioning, and assistance with ADLs. Other discharge instructions included clopidogrel 75 mg daily, Aspirin (ASA) 81 mg daily, and atorvastatin 80 mg daily. The patient was seen for an in-office visit with her primary care provider following hospitalization and reported lower extremity joint pain, intermittent shortness of breath, and continued right sided weakness but overall felt much better. On exam she had expressive aphasia, decreased breath sounds in her lung fields, and hemiparesis with 4 out of 5 strengths in her right upper and lower extremities.
As research has evolved, we have seen the novel coronavirus can cause microthrombi or small blood clots which can develop and travel throughout the body. This can obstruct blood flow to the brain and cause an ischemic stroke similar to the one seen in this case [8].
The increased inflammation associated with COVID-19 leads to plaque build-up in the arteries as well as clots in the vein causing said strokes [9,10]. Identifying and treating COVID-19 at its early stages has been shown to decrease complications associated with COVID-19 such as strokes, myocarditis, and pneumonitis [11]. Current testing procedures available such as RT-PCR and antigen testing have been shown to have at least a 30% false negativity rate. With this high false negativity rate, it is possible to misdiagnose a patient who is truly positive delaying potentially life-saving treatment. This makes the need for additional confirmatory testing imperative in symptomatic patients with suspected high-risk exposure [12]. Furthermore, patients with underlying conditions have also been shown to do poorly with increased morbidity and mortality when infected with COVID-19 [12]. The increase in morbidity and mortality can also be extended to vulnerable populations such as patients over the age of 65 and minorities. CT Scans have classic findings which are pathognomonic of COVID-19 and when used early by providers to guide treatment can aid in the prevention of worsening complications of COVID-19 such as strokes. Hester, et al. noted that the accuracy of a CT scan in symptomatic patients after a high-risk exposure should not be used as a stand-alone test but instead as a tool to help categorize patients into probable positive and probable negative cohorts [13]. Pulmonary imaging using chest CT and or chest radiographs may be helpful in identifying radiological abnormalities suggestive of a COVID-19 infection. This may even occur at earlier stages of infection when the patient is asymptomatic. In a small but significant proportion of ischemic stroke patients, typical symptoms of COVID-19 were not reported in 24.0% of participants [14]. Patients with COVID-19 infection carry a high risk of developing acute stroke especially in those with multiple organ dysfunctions [14]. There is a possibility that acute stroke patients may have undiagnosed COVID-19 infection in the following settings: 1) Patients may be in the COVID-19 prodromal period because, 2) Patient is an asymptomatic carrier, or 3) Neurological deficits seen in the early period of COVID-19 infection prompts and immediate stroke evaluation [14]. Providers must be very conscientious of these three settings due to the residual neurological deficits that often accompany anischemic stroke which can lead to long term morbidity and mortality. Additional testing including but not limited to D-dimer levels, cardiac troponin I, NT-proBNP, and interleukin-6 should also be considered as these levels can as be indicative of ischemic stroke in COVID-19 patients [1,2]. A limitation of this case report is only a D-dimer and troponin level was drawn while ZD was hospitalized.
The presented case demonstrates early CT findings consistent with COVID-19 in the setting of a negative RT-PCR test with symptoms, elevated D-dimer and troponin levels, following a high-risk exposure. The patient also has several underlying comorbid conditions, is over the age of 65, and a minority. Although the CT findings were consistent with COVID-19, the patient did not have a positive RT-PCR until her fourth test and 14 days after the abnormal CT findings. Due to the serious complications including but not limited to ischemic stroke in COVID-19 patients, it is imperative that primary care providers go the extra mile to order radiologic studies specifically chest CT scans where possible to aid in the diagnosis of COVID-19 in patients that have a history of high-risk exposure, underlying medical conditions, are a part of a high-risk group, and are presenting with clinical symptoms suggestive of COVID-19. Relying solely on the COVID-19 RT-PCR may lead to missed opportunities for diagnosis because there is a 30% false negative rate [12]. Early detection can lead to earlier treatment of COVID-19 along with earlier management of underlying conditions that in conjunction with COVID-19 can lead to more complications associated with higher rates of morbidity and mortality. Early treatment will ultimately reduce health care cost and aid in decreasing illness and death in already vulnerable populations.
No relevant financial affiliations or conflicts of interest.