Numerous studies have shown that music therapy (MT) and music listening (ML) can improve patient symptoms such as anxiety, pain, and relaxation. To investigate the effect of multiple ML sessions and the association between patient expectations and outcomes, patients were recruited from two nursing and rehabilitation centers in Roanoke, Virginia. Patients received three 30-minute ML sessions (experimental) or no intervention (control). Patient data included the Edmonton Symptom Assessment System (ESAS), vitals, and an expectations questionnaire. No difference was observed between the experimental and control groups when comparing symptoms and vitals. No correlation was observed between patient expectations and improvement in anxiety and pain (as measured by ESAS). However, patients who expected a clear improvement in anxiety demonstrated an improvement in systolic blood pressure and heart rate. Our results do not support the use of ML to improve anxiety and pain in chronically and terminally ill patients. Although no correlation was observed between patient expectations and symptom improvement, it may be helpful to utilize patient expectations when identifying those who may benefit from music interventions.
Music listening, Music therapy, Anxiety, Pain, Chronically ill, Terminally ill
Music interventions are used as complementary forms of treatment to help manage patients' symptoms, such as anxiety and pain [1-8]. They are used in a variety of settings including hospice and palliative care, perioperatively, and during hemodialysis and chemotherapy [1,5,9,10]. Music interventions are particularly beneficial for patients with chronic or terminal illnesses because these populations have a high prevalence of anxiety and pain [11-13]. In 2004, studies discovered 70% of terminally ill patients experienced either moderate anxiety (49%) or severe anxiety (21%) [12]. Anxiety and depression have been found to be the most common psychological problems in palliative care [13]. Terminally ill patients report fears stemming from a loss of control and the manner in which they will die. Medical treatments (prescriptions, doctor visits, etc.) can be viewed as intrusive and possibly increase the anxiety felt by the patient and their families. MT also provides an opportunity for both parties to express and share their emotions. Sometimes patients cannot overtly communicate their emotions through talking, due to their deteriorating state; music allows them to communicate without the need to talk [4,14].
Music therapy (MT) is "the clinical and evidence-based use of music interventions" in which "music is used within a therapeutic relationship to address physical, emotional, cognitive, and social needs of individuals" [15]. It is typically interactive and can include listening to live music played by the therapist, music-guided imagery and relaxation, or music improvisation by the patient (e.g. singing or playing instruments) [3,16]. Prior studies have shown that a single MT session can improve anxiety and pain in chronically and terminally ill patients [3,4,17]. However, there is some conflict about the evidence supporting the clinical use of MT amongst systematic reviews, which suggests that more studies are needed [16,18]. A Cochrane systematic review published in 2010 contradicted previous studies and reported there was no strong evidence that music therapy improved anxiety and pain in end-of-life care [16]. However, the results of a more recent systematic review suggest music therapy may be effective in reducing the pain of palliative care patients [18].
Music listening (ML) is defined as pre-recorded music administered by a healthcare professional who is not a music therapist [16,19]. It lacks the therapeutic relationship between patient and therapist and is often considered more passive. ML has been studied most frequently in the perioperative setting and has been shown to reduce patient anxiety and pain [5,6,10,20,21].
Most prior studies only utilized a single session of music intervention; therefore, the effect of multiple sessions is not well understood [2-5,10,17]. Various factors have likely played a role in the paucity of studies utilizing multiple sessions including decreased life expectancy of chronically and terminally ill patients and the use of ML in the perioperative setting (i.e. each patient has one music session associated with one operation).
During our literature review, we noted the impact of a patient's expectation (regarding a music intervention's effectiveness) on outcome measures (e.g. anxiety and pain) has not been well studied. The effect of patient expectations on outcomes has been studied in numerous other fields and the placebo effect is a well-known phenomenon [22-27]. Two systematic reviews concluded there is evidence to support the theory that positive patient expectations are associated with better outcomes [28,29].
The first objective was to investigate the effect of multiple ML sessions over a three-week period on patient symptoms in the chronically and terminally ill. These hypotheses were tested:
1. There will be a significant improvement between the experimental and control groups in pain, depression, anxiety, tiredness, drowsiness, and wellbeing as measured by the Edmonton Symptom Assessment System (ESAS).
2. There will be a significant improvement in anxiety between the experimental and control groups as measured by vitals (blood pressure (BP), heart rate (HR), and respiration rate (RR)).
The second objective was to investigate the association between patient expectations and the effect of multiple ML sessions over a three-week period on patient anxiety and pain in the chronically and terminally ill. These hypotheses were tested:
1. There will be a correlation between higher patient outcome expectations and greater improvement in anxiety and pain as measured by the ESAS.
2. There will be a correlation between higher patient outcome expectations and greater improvements in anxiety as measured by vitals (BP, HR, and RR).
This study was approved by the institutional review board (IRB) at Carilion Clinic. Participants were recruited from two nursing and rehabilitation centers in Roanoke, Virginia. These facilities are comprised of mainly chronically ill patients, with a small percentage of terminally ill patients.
One hundred and fifty-nine patients were recruited between April 2014 and January 2018. Patients were ineligible to participate if they were unable to hear, comatose, obtunded, or had conditions that prevented them from completing the ESAS and questionnaires. Patients with dementia were allowed to participate if a family member provided consent. After consent was obtained, the participant's name, age, primary illness, and facility location were recorded.
Patients were assigned to either the experimental or control group, based on their willingness to participate in ML sessions. The experimental group received three 30-minute ML sessions; one a week for three weeks. Patients listened to popular music from the 1940s, 1950s, or 1960s via compilation CDs or an iPod. They were assigned music from the decade in which they were in their 20s (or the closest of the three options). The compilations had a wide variety of music; there were softer ballads as well as more upbeat songs (e.g. "rock 'n roll" songs).
The control group did not receive ML sessions. Patients were visited once a week for three weeks to collect data (ESAS and vitals); visits typically lasted less than 10 minutes.
The ESAS is a commonly used tool that was developed to assess symptoms in palliative care patients [30]. It assesses the severity of the following symptoms: pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, wellbeing, and shortness of breath. The ESAS uses a scale from 0-10, where 0 typically designates "no symptom" (e.g. no pain) and 10 typically designates the "worst possible symptom" (e.g. worst possible pain). The validity and reliability of the ESAS has mainly been studied in cancer patients. A review by Richardson and Jones (2009) [31] looked at various articles that focused on patients with cancer and found that the ESAS is reliable but has restricted validity. We were unable to find articles discussing the use of the ESAS in other contexts. With regards to the expectations questionnaire we used in our study, we modeled that after some questions that were previously used by Linde, et al. (2007) [25], which we do not believe were tested for validity and reliability.
At the beginning of the study, baseline ESAS and vitals (BP, HR, and RR) were taken for all patients. The experimental group had additional ESAS and vitals taken after each of the three ML sessions (within 15 minutes of the session's completion). The control group also had ESAS and vitals taken once a week for three weeks.
A subset of patients in the experimental group (the last 63 patients recruited) also answered a baseline questionnaire regarding their expectations. The questions used "music therapy" instead of "music listening" for simplicity; we felt patients might be confused by the distinction between MT and ML. Questions 1-3 in the baseline questionnaire were previously used by Linde, et al. and were modified for our purposes [25].
The questionnaire included the following questions:
1. "How effective do you consider music therapy in general?" Answer options: Very effective, effective, slightly effective, not effective.
2. "Regarding your anxiety, what do you personally expect from the music therapy treatment you will receive?" Answer options: Clear improvement, slight improvement, no improvement.
3. "Regarding your pain, what do you personally expect from the music therapy treatment you will receive?" Answer options: Clear improvement, slight improvement, no improvement.
4. "Have you received music therapy before?" Answer options: Yes, no.
A power analysis for the first objective was performed; the study was powered to identify changes in pain and anxiety from baseline. The α value was 0.025, which was adjusted based on the Bonferroni correction (p-value divided by the number of primary questions). With a power of 80% and an α value of 0.025, a minimum sample size of 110 patients was required (55 control and 55 experimental).
Another power analysis was performed for the second objective. A previous study performed by Hui, et al. found that the minimally clinically significant change in ESAS scores is ± 1 (effect size = 0.4) [32]. With a power of 80%, an α value of 0.05, and a change in ESAS score of 1, a sample size of 63 experimental patients was needed.
All patients who had completed at least the baseline and week 1 sessions were included in the data analysis. Although 159 patients were recruited, 8 patients were excluded because they only completed the baseline session. The analysis for the first objective included 96 experimental patients and 55 control patients, and the analysis for the second objective included 63 experimental patients.
RStudio was used for our analysis. A two-sample t-test was used to compare the baseline values (nine ESAS variables and four vitals) of the control and experimental groups. An Analysis of Variance (ANOVA) was used to compare the baseline values (ESAS anxiety, ESAS pain, and four vitals) among the three expectation groups (clear improvement, slight improvement, and no improvement).
We used lme4 to perform linear mixed effects analyses of the various outcome measures and the various groups (e.g. control and experimental; patient expectations - clear, slight, or no improvement) [33]. Although our power analyses involved two different α values (0.025 and 0.05), a p value of 0.05 was used for simplicity during data analysis.
The Kruskal Wallis One-Way Analysis of Variance (ANOVA) was performed to compare the mean change in anxiety (change = baseline anxiety score - last session anxiety score) for patients who had completed one, two, or three ML sessions. A similar ANOVA was also performed for mean change in pain.
Data was analyzed for 151 patients; 96 experimental and 55 control patients. The age, sex, and primary (i.e. admitting) diagnosis were recorded for each patient (Table 1). Only one patient was in hospice care.
Table 1: Patient demographics. View Table 1
A two sample T-test was used to compare the baseline mean scores for all nine ESAS variables and the baseline mean vitals (systolic BP, diastolic BP, HR, and RR) of the control and experimental groups. There was a significant difference between the two groups' baseline nausea scores; the experimental group had a higher mean nausea score (p = 0.036, Table 2). No significant differences were observed for the other ESAS variables or vitals (Table 2).
Table 2: Comparison of baseline ESAS scores and vitals between the control and experimental groups. View Table 2
An ANOVA was used to compare the baseline mean ESAS anxiety score and the baseline mean vitals between the three expectation groups (clear improvement, slight improvement, and no improvement; patients were separated based on their expectations regarding ML's effect on anxiety). An ANOVA was also used to compare the baseline mean ESAS pain scores among the three expectation groups (patients were separated based on their expectations regarding ML's effect on pain). No significant differences at baseline were observed when comparing the three expectation groups (Table 3).
Table 3: Comparison of baseline ESAS scores and vitals between the three expectation groups. View Table 3
Of the 151 participants included in our analysis, 40 patients (26.5%) did not complete the study (Figure 1). Reasons included: disinterest, discharge from facility, hospitalization, deterioration of condition to an extent that participation could no longer be expected, and death. Discharge from facility was the most common cause of attrition (21 patients, 13.9%).
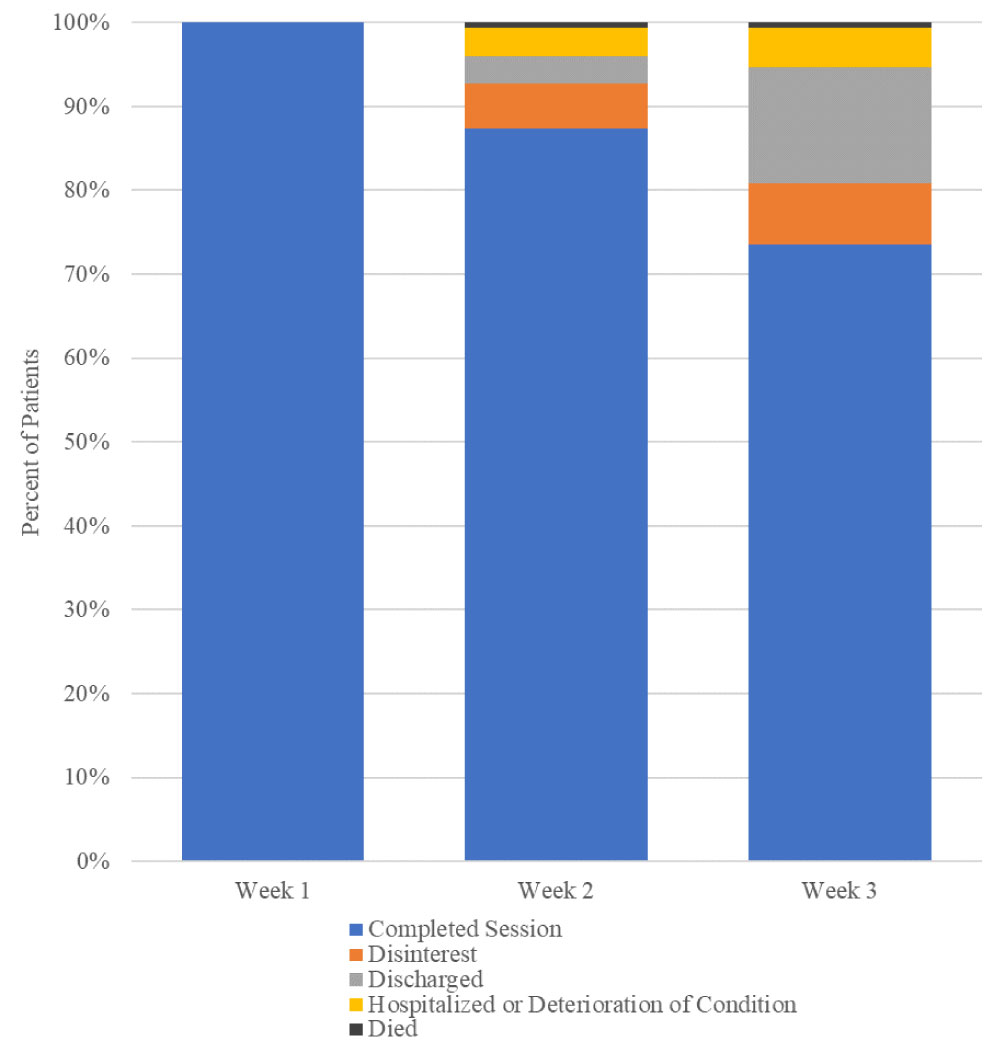 Figure 1: Patient attrition.
View Figure 1
Figure 1: Patient attrition.
View Figure 1
(Figure 1) Forty patients (26.5%) did not complete the study for various reasons (n = 151). Reasons for attrition included: discharge from facility (13.9%), disinterest (7.3%), hospitalization or deterioration of condition (4.6%), and death (0.7%).
The first hypothesis, that there will be a significant difference between the experimental and control groups in pain, depression, anxiety, tiredness, drowsiness, and wellbeing as measured by the ESAS, was not supported. A mixed model analysis showed no significant difference in patient symptoms between the two groups (Figure 2 and Table 4).
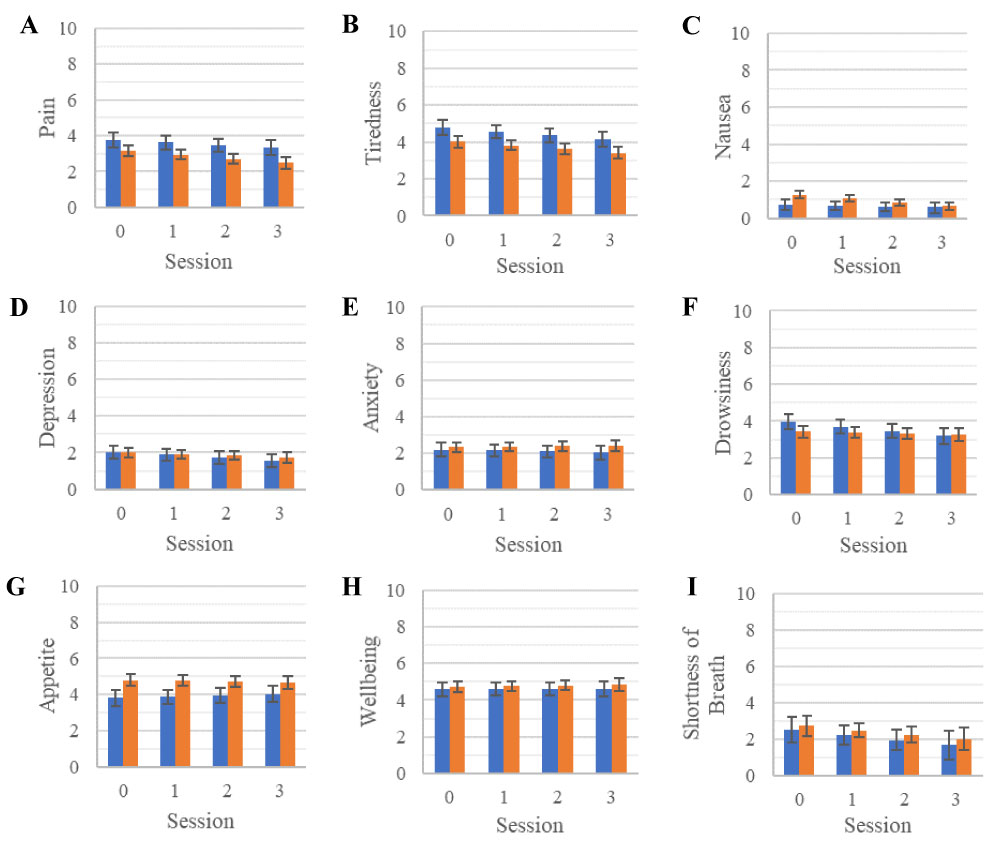 Figure 2: Vitals for the control and experimental groups.
View Figure 2
Figure 2: Vitals for the control and experimental groups.
View Figure 2
Table 4: P Values for mixed model analyses of ESAS scores and vitals by treatment group. View Table 4
(Figure 2) A mixed model analysis was performed to compare the ESAS symptom scores of the control group (n = 55; blue) and the experimental group (n = 96; orange). Symptoms measured by the ESAS include: pain (a), tiredness (b), nausea (c), depression (d), anxiety (e), drowsiness (f), appetite (g), wellbeing (h), shortness of breath (SOB, i). Baseline ESAS scores are represented as Session 0 and ESAS scores from weeks 1-3 are represented as Sessions 1-3. Error Bars = Standard Error.
The second hypothesis, that there will be a significant difference in anxiety between the experimental and control groups as measured by vitals (BP, HR, and RR), was not supported. A mixed model analysis showed no significant difference in vitals between the two groups (Figure 3 and Table 4).
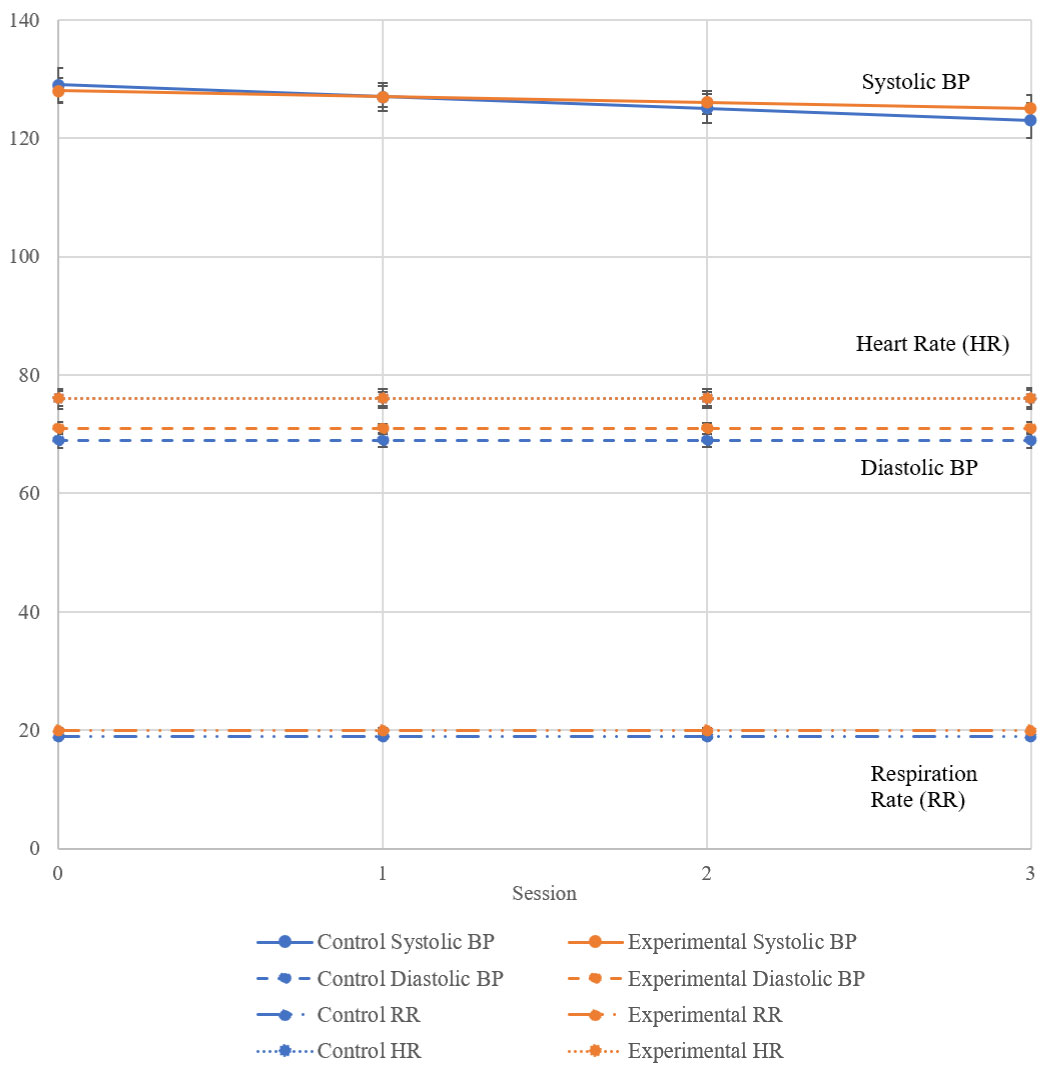 Figure 3: Vitals for the control and experimental groups.
View Figure 3
Figure 3: Vitals for the control and experimental groups.
View Figure 3
(Figure 3) A mixed model analysis was performed to compare the vitals of the control group (n = 55; blue) and the experimental group (n = 96; orange). Baseline ESAS scores are represented as Session 0 and ESAS scores from weeks 1-3 are represented as Sessions 1-3. The line for Control HR is unable to be seen clearly because it closely overlaps with the line for Experimental HR. Error Bars = Standard Error.
Kruskal Wallis One-Way ANOVAs were performed to compare the mean changes in anxiety and pain (e.g. change = baseline anxiety score - last session anxiety score) for patients who had completed one, two, or three ML sessions. There were no significant differences in the mean change in anxiety and pain between the patients who received one, two, or three sessions.
Sixty-three patients in the experimental group answered the baseline expectations questionnaire (Table 1).
The first hypothesis, there will be a correlation between higher patient outcome expectations and greater improvements in anxiety and pain as measured by the ESAS, was not supported. The patients who expected a clear or slight improvement in anxiety did not have a significant change in anxiety over the three-week period (Figure 4). However, there was a significant interaction between expectation and anxiety in patients who expected no improvement in anxiety. This group had an increase in anxiety over the three-week period (p = 0.006, Figure 5 and Table 5). There was no significant interaction between expectation and pain. However, all patients trended towards an improvement in pain (p session number= 0.094, Figure 4).
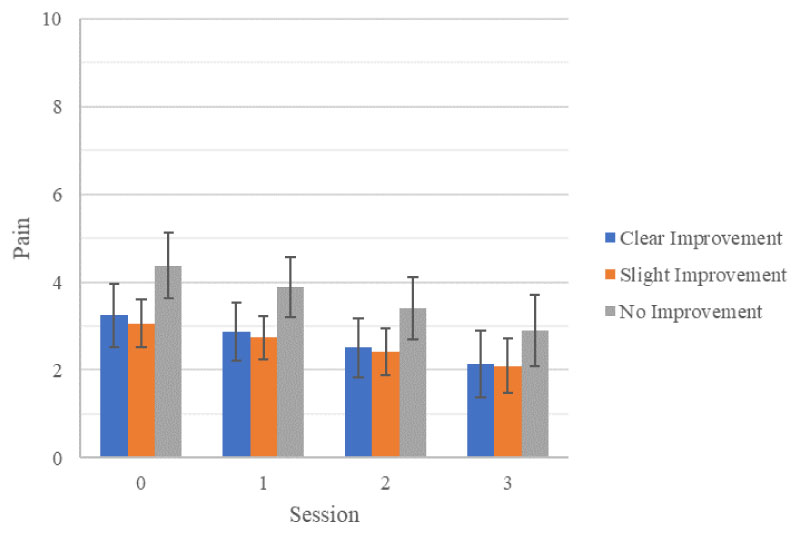 Figure 4: ESAS pain score by patient expectation.
View Figure 4
Figure 4: ESAS pain score by patient expectation.
View Figure 4
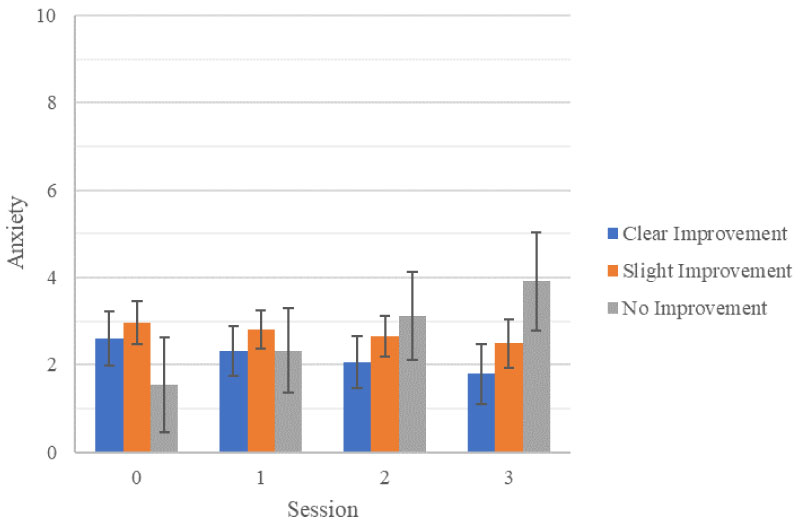 Figure 5: ESAS anxiety score by patient expectation.
View Figure 5
Figure 5: ESAS anxiety score by patient expectation.
View Figure 5
Table 5: P values for mixed model analyses of ESAS scores and vitals by expectation group. View Table 5
(Figure 5) A mixed model analysis was performed to compare the ESAS anxiety scores of experimental patients (n = 63). Patient data was stratified by expectation regarding ML's impact on anxiety into three groups: clear improvement (n = 21; blue), slight improvement (n = 35; orange), and no improvement (n = 7; gray). Error Bars = Standard Error.
(Figure 4) A mixed model analysis was performed to compare the ESAS pain scores of experimental patients (n = 63). Patients were separated by expectation regarding ML's impact on pain into three groups: clear improvement (n = 17; blue), slight improvement (n = 30; orange), and no improvement (n = 16; gray). Error Bars = Standard Error.
The second hypothesis, there will be a correlation between higher patient outcome expectations and greater improvements in anxiety as measured by vitals (BP, HR, and RR), was supported in the following categories: Systolic BP and HR.
There was a significant interaction between expectation (clear improvement: p = 0.025, slight improvement: p = 0.035) and systolic BP (Figure 6 and Table 5). Patients expecting a clear improvement in anxiety had a decrease in systolic BP, while those expecting a slight improvement in anxiety had an increase in systolic BP. Patients who expected no improvement in anxiety did not experience a significant change in systolic BP over the three-week period (p = 0.175, Figure 6 and Table 5).
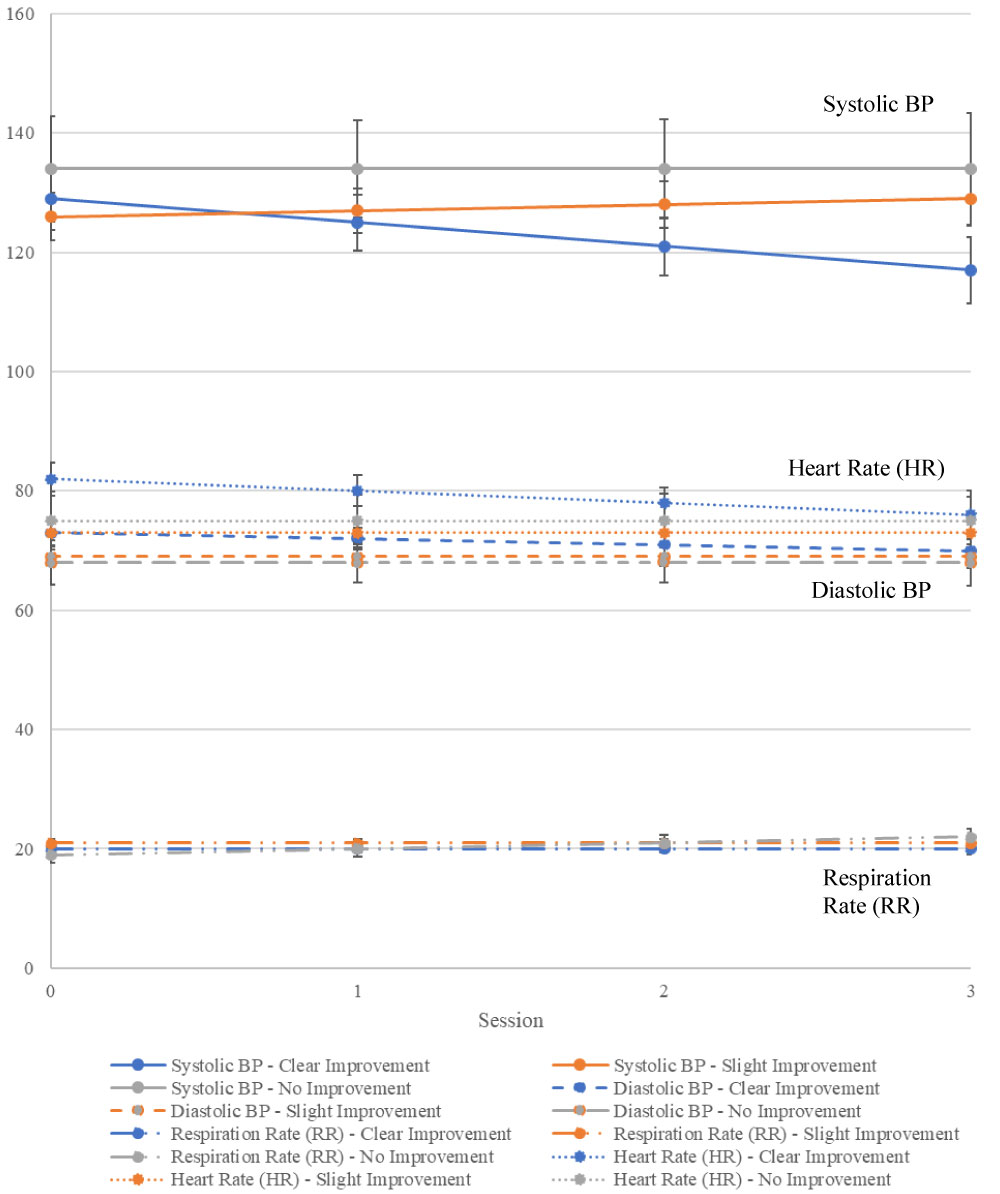 Figure 6: Vitals by patient expectation.
View Figure 6
Figure 6: Vitals by patient expectation.
View Figure 6
There was no significant change in diastolic BP over the three-week period across all expectation groups (Figure 6 and Table 5).
There was a significant interaction between expectation and HR for patients who expected a clear improvement in anxiety as demonstrated by a decrease in HR (p = 0.022, Figure 6 and Table 5). The patients who expected a slight improvement or no improvement in anxiety did not experience a significant change in HR (p = 0.086 and p = 0.325, respectively; Figure 6 and Table 5).
Patients who expected either a clear or slight improvement in anxiety did not experience a significant change in RR over the three-week period (p = 0.583 and p = 0.307, respectively; Figure 6 and Table 5). However, there was a significant interaction between the expectation of no improvement in anxiety and RR as evidenced by an increase in RR (p = 0.017, Figure 6 and Table 5).
(Figure 6) A mixed model analysis was performed to compare vitals (BP [systolic and diastolic], HR, and RR) of experimental patients (n = 63). Patients were separated by expectation regarding music listening's impact on anxiety into three groups: clear improvement (n = 21; blue), slight improvement (n = 35; orange), and no improvement (n = 7; gray). Error Bars = Standard Error.
No significant difference was observed when comparing patient symptoms (as measured by ESAS) and vitals for the experimental and control groups. Although a significant difference existed at baseline between the two groups for nausea, it was not thought to be clinically significant because the mean scores for both groups were low (control = 0.67, experimental = 1.46; p = 0.036; Table 2). Additionally, there are numerous factors (e.g. illnesses, medications, diet) that can influence a patient's baseline level of nausea.
Our results differ from those of prior studies that demonstrated ML can reduce anxiety, decrease pain, improve mood, and increase relaxation in the non-perioperative setting [6,10,20]. One notable difference is that previous studies incorporated patients' music preferences, whereas we assigned music based on age. There have been conflicting results regarding the impact of patient-selected music, so the importance of patient music preferences in ML studies is currently unclear [34,35].
This study's results also differ from the results of numerous MT studies, which demonstrated MT can decrease anxiety, pain, tiredness, and drowsiness, as well as improve mood and relaxation [2-4,17]. As mentioned previously, MT and ML are two distinct types of music intervention. We believe our music intervention did not significantly improve patient symptoms because ML lacks the therapeutic relationship present in MT. Our results suggest ML is not an adequate substitute for MT.
However, it is interesting to note that a 2015 study performed a randomized cross-over trial, which compared the effects of two MT sessions and two ML sessions (utilizing individualized playlists) in cancer patients. Their results suggested that both MT and ML were equally effective in improving anxiety, pain, mood, and relaxation [20]. It is possible different patient populations could account for differing results; the 2015 study involved only cancer patients whereas our study involved patients with a wide range of diagnoses.
Our results showed no significant difference in vitals between the experimental and control groups. We used vitals as a physiologic indicator of anxiety. However, vitals are affected by many factors, including but not limited to: medications, presence or absence of cardiac and/or pulmonary disease, psychosocial stressors, pain, and anxiety. Therefore, the ML sessions were only one of the many factors affecting our patientsí vitals. A prior study by Horne-Thompson, et al. also reported no significant difference in HR between the control and experimental groups when using MT. In fact, they proposed that MT may have energizing effect, leading to an increased HR [3].
Our data analysis demonstrated no significant difference in the mean change in symptom (i.e. anxiety, pain) based on the number of ML sessions received (i.e. one, two, or three). This suggests there was no additive effect. However, an additive effect could possibly be achieved with more sessions over a longer period of time.
No correlation was observed between patient outcome expectations and improvement in anxiety and pain (as measured by ESAS). However, our analysis showed patients who expected no improvement in anxiety had a significant increase in anxiety over the three-week period (p = 0.006, Figure 5 and Table 5). This may suggest that patients who expect no improvement in anxiety are less likely to experience any anxiety-reducing benefits ML has to offer. It is unclear why patients who expected no improvement in anxiety from ML had a significant increase in anxiety. It is possible that this group of patients' belief that ML does not improve anxiety negatively influenced their experience with ML (i.e. thinking negative thoughts can lead to a negative outcome). It is important to note that our expectations questionnaire did not have worsening of a symptom (e.g. worsening of anxiety or pain) as a possible response; this group of patients may have actually believed that ML can worsen anxiety. It is also possible that this group of patients had a particularly negative experience with the popular music that we played for them during the ML sessions. Over the three-week period, all three expectation groups trended towards improvement in pain. This may suggest that expecting no improvement in pain does not prevent a patient from receiving the potential pain-reduction benefits that ML has to offer. This information could be used to help healthcare professionals and music therapists identify patients most likely to benefit from music intervention.
Our analysis demonstrated a correlation between high patient outcome expectations and greater improvements in anxiety as measured by systolic BP and HR, but only for the clear improvement group. We did not observe a similar correlation with diastolic BP and RR. These results are inconsistent with a prior meta-analysis that found positive expectations were associated with better patient outcomes across various medical conditions [31].
Patient recruitment was based on patients' willingness to participate in ML, which prevented patient randomization. Additionally, our investigation of patient expectations may have had a biased patient sample. Patients who do not believe that MT and ML are beneficial (in general and/or with regards to anxiety and pain) were probably less likely to want to participate in our study. The population that did participate was heterogeneous as demonstrated by the variety of diagnoses in the results section. This lack of homogeneity could introduce confounding variables, which could impact the validity of this study. Within this population, due to constantly changing medication regimens, it was not addressed if participants were being treated with pain medication (opioid and non-opioid), which could obviously augment their levels of pain. Finally, due to various reasons (e.g. patient discharge, disinterest, deterioration of condition), roughly 28% (Figure 1) of patients did not complete all three sessions.
Although a prior study directly compared MT and ML, it studied a different patient population (cancer patients) [20]. A potential future direction for our research would be to conduct a study that directly compares MT and ML in the chronically and terminally ill. This would allow us to further investigate our patient population and the clinical implications of both music interventions.
The results of this study do not support the use of ML to improve anxiety and pain in the chronically and terminally ill. Although no correlation was observed between patient expectations and symptom improvement, it may be helpful to utilize patient expectations when identifying those who may benefit from music interventions. Future directions could include the direct comparison of MT and ML in the chronically and terminally ill.
None.
None.
We would like to thank all of the patients who participated in the study. We also want to thank the staff at both Friendship Health and Rehab Center and Brandon Oaks Nursing and Rehabilitation Center, Danielle Guilliams, and Dr. Crystal Truong for their support and assistance with this study. Finally, we want to thank Allison N. Tegge, PhD and Katherine Shaver for their help with the statistics for this study.