Pregnancy-related structural changes to the abdominal-pelvic region can cause perinatal and postpartum disorders such as diastasis recti (DRA) and pelvic floor dysfunction (PFD).This research describes the occurrence of DRA and PFD symptoms, diagnosis, use of prevention/treatment methods and sources of education among 152 women < 15 months post-partum. Data was gathered using an online survey.150 and 122 participants reported at least some symptoms of PFD and DRA, respectively; 8 and 11 women, respectively, received a formal diagnosis. There were no significant differences between women scoring in the top 25% vs. bottom 25% on the Pelvic Floor Disability Index short form (PFDI-20) or between participants who did or did not receive formal diagnosis on measures of maternal weight changes, parity, or months post-partum (p > 0.05). Abdominal support garments were the most common (n = 49) form of prevention and/or treatment method used. The most common source of information on abdominal support garments was a friend/colleague (n = 8). No significant difference was found between women who used any intervention method compared to those who did not on PFDI-20 score or number of DRA symptoms (p > 0.05). Findings indicate a high incidence of PFD/DRA symptoms. Formal diagnosis and medical counseling on treatment/prevention is lacking.
Pregnancy, Pelvic floor distress inventory, Abdominal support garment, Maternal health, Abdominal-pelvic dysfunction
A mother's physical health impacts other dimensions of personal health (e.g. psychological, emotional), [1,2] as well as the health of her offspring [3-5]. For many women, the childbearing process is a significant and highly anticipated part of life. During pregnancy, the female body adapts to support the growing fetus and anatomical changes are made specifically in the pelvic region to support delivery. These adaptations can impair a mother's functional capabilities during and after pregnancy.
Commonly consequential of pregnancy and parturition, diastasis recti abdominis (DRA) and pelvic floor dysfunction (PFD) challenge the structural integrity of the abdominal-pelvic region creating functional deficiencies throughout the kinetic chain. DRA occurs as the muscle bellies of the rectus abdominis elongate and separate in response to pregnancy [6]. Consequences may include cosmetic alterations such as a bulge or recess, limitations to trunk movement and strength in all planes of motion, compromised trunk stability and posture, lack of muscular control throughout the abdominal-pelvic region, and a higher susceptibility to injury [6-10]. As well, PFD can cause urinary and fecal incontinence, disordered sexual function, pelvic organ prolapse, and general pelvic pain [11,12]. The symptoms of these disorders limit a mother's ability to complete a variety of tasks, including various forms of physical activity from playing with their children to exercising. Research shows that the majority of parous women do not return to their pre-pregnancy levels of physical activity after childbirth [13,14]. Prolonged inactivity leads to a plethora of mental and physical health issues, namely depression, unhealthy body weight, loss of coordination and strength, and lack of general self-confidence [1,2,5]. Although gaining weight is advised during pregnancy, excessive/unhealthy weight gain and retention of excessive body weight after pregnancy can lead to chronic metabolic and cardiovascular health conditions [1,5]. Minimizing factors that contribute to these physical, mental, and emotional issues should be a priority in maternal healthcare. Because of the significant role that mothers play in societal health, it may be no stretch to say the ramifications of DRA and PFD are public health issues.
Among the few studies that address the prevalence of DRA in the pregnant and postpartum population, variance ranges from 33% to 100% during mid- to late-term pregnancy and 39% to 60% six-weeks postpartum and beyond [15-17]. Current, but limited, data regarding PFD shows that pregnancy beyond 20 weeks gestation increases the prevalence of PFD [18]. Specifically, PFD prevalence among parous women ranges from 18.4% to 32.4%, depending on parity, compared to 12.8% in nulliparous women [19]. Interest in the prevalence of DRA and PFD has increased as the impact of the consequences of these disorders becomes more apparent. However, many women and healthcare professionals consider symptoms of DRA and PFD to be unfortunate, but natural consequences of the childbearing process. Because of this, these disorders often go undiagnosed and prevalence estimates likely under represent actual occurrence. As well, specific characteristics associated with increased symptom severity of both PFD and DRA, and the consequences of experiencing these symptoms, are not well explored.
To date, there is relatively limited research concerning prevention and treatment options for DRA and PFD. While surgical interventions are some of the most common solutions, these procedures come with relatively high rates (up to 40%) of patient dissatisfaction and complications [20]. Moreover, 30% of women who undergo surgery for any symptom of PFD require additional operative intervention(s) [21]. Non-invasive approaches, such as therapeutic exercise and kinesio taping (KT), may be an efficacious means to improve number and severity of DRA and PFD-related symptoms [8,20,22-24]. To our knowledge, no studies indicate that therapeutic exercise or KT can be detrimental. At their worst, these intervention methods may have no significant benefit for symptoms of DRA and PFD [25].
The use of abdominal support garments is becoming more popular, primarily because of the conveniences (i.e, wide commercial availability, generally affordable options, easy application). As a sole intervention method, an abdominal support can help reduce abdominal-pelvic pressure, strain and fatique [26]. By assisting in the stabilization of the spine and sacroiliac joint, they can also help alleviate pregnancy-related lower back and pelvic girdle, specifically symphyseal, pain [27-30]. Enhanced stabilization of the spine and pelvic girdle, as the result of wearing an abdominal support, has also been shown to increase proprioception and functionality and decrease fall risk in the pregnant population [30,31]. As an adjunct intervention method with corrective exercise and when worn appropriately, an abdominal support may also help alleviate pain and minimize the physical stress applied to the muscles and connective tissues of the abdominal-pelvic region during the childbearing process and the postpartum period [9,24]. Abdominal supports are easy to use, comfortable, and accessible; therefore, justification for prescribing an abdominal support during pregnancy or the postpartum period is apparent. To our knowledge, a single observational study exists describing the prevalence of planned abdominal binder use [32], however the actual incidence of abdominal support prescription or voluntary use during the postpartum period is unknown. Likewise, with the rise of interest and evident efficacy of abdominal support use, a simultaneous rise in the number of women receiving education from their healthcare provider on the use of these devices would be expected. Whether women are receiving any amount of education from their healthcare providers about wearing an abdominal support as a sole or conjunct intervention method for symptoms of pregnancy-related DRA and/or PFD is unclear.
Complication-free exercise, normal sexual function, self-confidence in one's personal coordination and strength, and proper fecal and urinary function are all critical components to return to and maintain an ideal level of physical health and general wellbeing after childbirth. Failure to provide proper DRA and PFD diagnoses and education to women during pregnancy and in the post-partum period puts mothers in jeopardy of unnecessary mental and physical hardships and health risks. Currently, it is unclear how many women receive such diagnoses and/or education on use of an abdominal support; therefore, the purpose of our research is to:
1. Quantify any discrepancy between the prevalence of self-reported symptoms and formal diagnoses of DRA or PFD in a sample of women who have given birth within the last 15 months.
2. Compare the delivery method, PDFI-20 scores, age, pre- to post-childbearing weight change, parity, and amount of time since birth of the top 25% to the bottom 25% of PFDI-20 scores. These variables will also be compared and examined between women with1or fewer DRA symptoms to those who reported 2 or more DRA symptoms.
3. Describe self-reported consequences of experiencing DRA and PFD symptoms, types of intervention methods used to prevent and/or treat these disorders and the perceived benefit of these intervention methods. Compare PFDI-20 scores and number of reported DRA symptoms between women who chose to use any type of intervention method during pregnancy or post-pregnancy to those who did not.
4. Survey women on knowledge of, source of knowledge, and use of an abdominal support as an intervention method for DRA and PFD, and if used, the timing of use and conditions under which the abdominal support was used.
It was hypothesized that the prevalence of women experiencing symptoms of DRA and/or PFD would be much higher than the number of formal diagnoses. Likewise, education provided by healthcare professionals concerning the use of abdominal supports garments would be inadequate.
Prior to any collection of data, permission was obtained from the Southern Utah University (SUU) Institutional Review Board (IRB), #06-102021a. Participants were recruited through social media platforms Facebook and Instagram. A public post briefly describing the purpose and length of the questionnaire, with an open link to the survey, was posted to Facebook and Instagram. The survey link was "shareable", therefore, it is possible that it was shared on platforms outside Facebook and Instagram. Question 1 of the survey was the informed consent document which, to complete the survey, participants would have had to select "Yes, I understand" after reading the informed consent. All data was anonymous and unable to be traced back to an email address, IP address, social media account etc.
The sample was comprised of parous, biological females. All participants were 20-40 years-old, ≤ 15 months postpartum, not currently pregnant, and had no history of abdominal or pelvic surgeries other than a cesarean section. Participation was voluntary and each participant was required to acknowledge their consent prior to accessing survey questions. Personal identities and data collected from individual responses was anonymous. No compensation or incentives were provided for those who chose to participate.
A 15-20-minute electronic Qualtrics survey was used to collect participants' responses virtually. The survey asked preliminary questions to eliminate potential participation from those who did not meet the inclusion criteria and to gather information on general demographics. Participants were asked if they had received a DRA and/or PFD diagnosis from their healthcare provider and, if so, the timing of that diagnosis. Regardless of diagnosis status, participants were asked about prevalence and severity of PFD symptoms using the Pelvic Floor Disability Index Questionnaire (PFDI-20) [33]. The PFDI-20 has been shown to have a high test-retest and inter-rater and intra-rater reliability (ICC = 0.93, r = 0.93 and r = 0.93, respectively) and is valid for measuring the symptom severity of pelvic floor disorders [33,34]. Within the PFDI-20, a Likert scale is used to rank the level of bother each participant has experienced from symptoms of urinary distress, colorectal-anal distress, and pelvic organ prolapse (0, being "no", to 4, being "quite a bit"). The PFDI-20 (Figure 1) is scored by taking the mean value of all questions answered and multiplying that number by 25. Possible scores range from 0 - 300, the higher the score, the greater the number and severity of symptoms. No such survey currently exists to determine the presence or severity of DRA, however, participants were asked if they experienced any or all of the following symptoms: A visible separation or bulge down the midline of the abdomen, lower back pain, and/or a reduction in abdominal strength. These are well-understood symptoms of DRA [6-10,35].
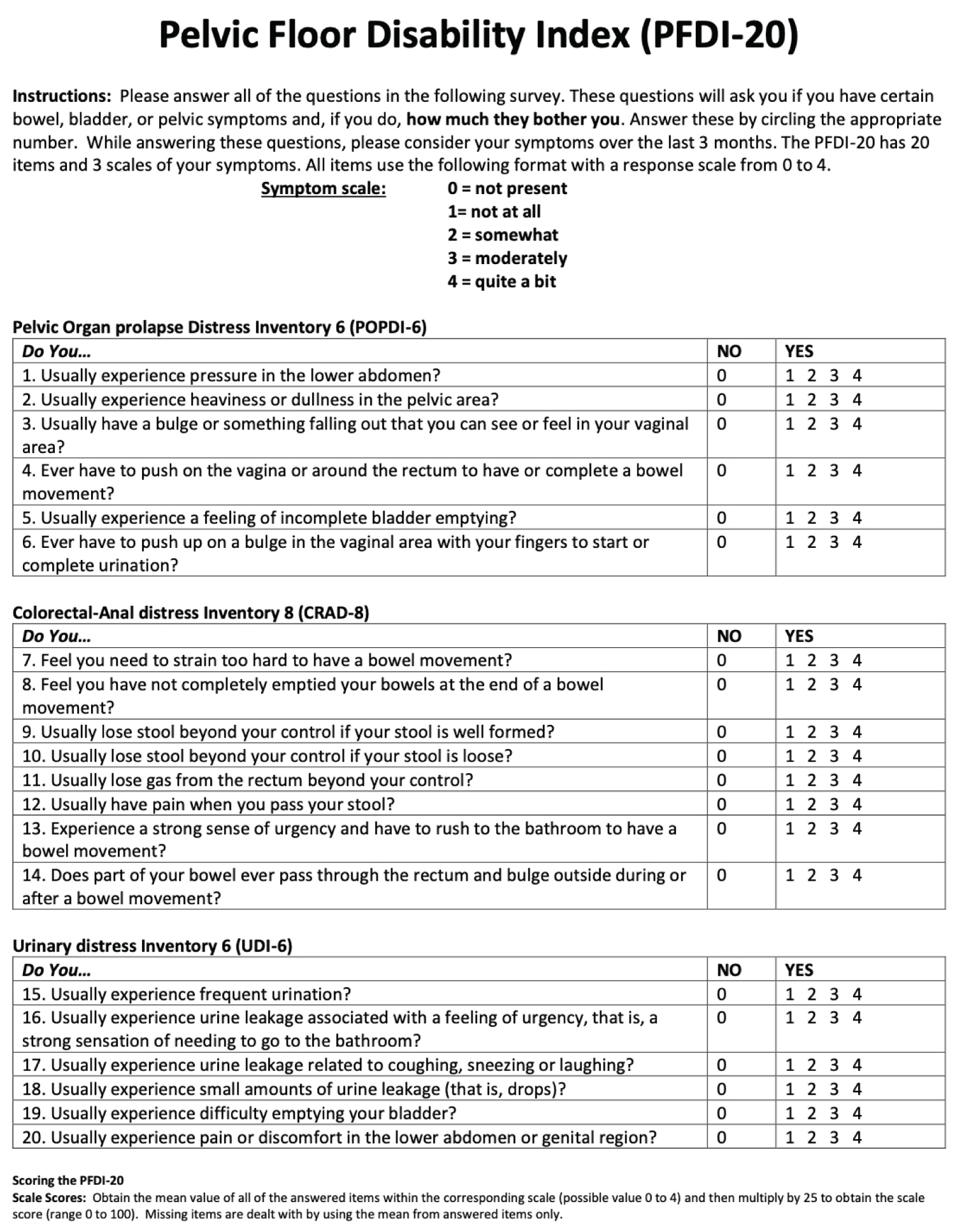 Figure 1: Pelvic floor disability index.
View Figure 1
Figure 1: Pelvic floor disability index.
View Figure 1
If applicable, participants were given a series of options to describe how their life has been affected as a consequence of these muscular disorders and to select all that apply. Options for consequences of DRA included cosmetic concerns, such as a belly bulge, lordosis of the back, poor posture, low back pain, reduced abdominal strength, hernia, or other. Consequences of PFD included interference with playing with your kids, discomfort/pain during intimacy, no or limited return to exercise, body image issues, or other.
Mothers were also asked if any intervention method was employed. Participants reported what intervention they used and if they believed it to be beneficial. Options for intervention methods included surgery, special exercise (including physical therapy), kinesiotaping (KT), abdominal bracing, or other. Women were also specifically asked about existing knowledge of abdominal supports/bracing and any source of education including: Doctor, social media, internet, a friend/colleague, book/magazine, or other. If a participant reported use of an abdominal support at any time during the childbearing process, they were asked to also report the timing (i.e. during pregnancy and/or the postpartum period), frequency, and conditions (i.e. exercise, daily tasks, and/or resting) under which they chose to wear it.
Once closed, results from the survey were exported from Qualtrics to Excel for data analysis. Frequencies were used to quantify the prevalence of DRA and PFD symptoms among women, as well as how many of these women have received a formal diagnosis of either disorder. Independent t-tests were used to find significant differences between women who scored in the top 25% vs. bottom 25% on the PFDI-20 scores in regard to PFDI-20 score, age, pre- to post-childbearing weight change, and amount of time since giving birth. Chi-square tests were used to determine if there were differences between women who scored in the top 25% vs. bottom 25% on the PFDI-20 in regard to cesarean section and parity. Independent t-tests were used to find any significant difference between women with 1 or fewer DRA symptoms and those who reported 2 or more DRA symptoms in regard to PFDI-20 scores, age, and pre- to post-childbearing weight change. A Chi-square test was used to find any differences between women who reported 1 or fewer DRA symptoms vs. 2 or more DRA symptoms and parity. Frequencies were used to describe self-reported consequences of DRA and/or PFD symptoms, to determine number of women who utilized any type of intervention method for these disorders either during pregnancy or the postpartum period, and to identify the perceived benefit of these intervention methods. Independent t-tests were used to identify any difference in PFDI-scores and the number reported DRA symptoms between women who chose to use any type of intervention method and those who did not. The use of an abdominal support garment was individually analyzed using frequencies to describe the extent, timing, and conditions of use. Frequencies were used also to calculate the number of women who had preexisting knowledge of the use of an abdominal support and the source of that knowledge. The significance level was set at p < 0.05 for all.
One hundred and fifty two of the 202 women who accessed the survey completed it adequately. The demographics of all 152 participants are presented in Table 1. Of the 122 (80.3%) women who reported experiencing at least 1 symptom of DRA during pregnancy or post-childbirth, 11 (9.0%) women received a formal diagnosis. The average number of DRA symptoms was 1.5 ± 1.1. Of the 150 (98.7%) women who experienced PFD symptoms, 8 (5.3%) women received a formal diagnosis. Average PFDI-20 score for all 152 women was 94.3 ± 46.9; PFDI score was not associated with a medical diagnosis of PFD (p > 0.05) (Table 2).
Table 1: Sample demographics. View Table 1
Table 2: Range and frequency of Pelvic Floor Disability Index -20 (PFDI-20) scores and occurrence of medical diagnoses. View Table 2
Women in the top 25% of PFDI-20 scores were compared to those who scored in the bottom 25% and no significant differences were found in regard to delivery method, age, weight changes, parity, and amount of time since birth (p > 0.05) (Table 3). Women with 1 or fewer DRA symptoms (n = 70) were compared to those with 2 or more DRA symptoms (n = 61) and significant differences were found in regard to PFDI score, age, and parity (p = 0.000007, 0.01, and 0.01, respectively), and no significant differences were found in regard to weight changes and amount of time since birth (p > 0.05) (Table 4). Symptoms of DRA were reported by 85 women while 111 women reported at least one life-limiting consequence of PFD (Table 5).
Table 3: Characteristics of women who scored in the top 25% vs. bottom 25% on the Pelvic Floor Disability Index (PFDI-20). View Table 3
Table 4: Characteristics of participants with ≤ 1 diastasis recti abdominis (DRA) symptoms and ≥ 2 symptoms. View Table 4
Table 5: Symptoms of Diastasis Recti (DRA) and reported consequences of Pelvic Floor Dysfunction (PFD). View Table 5
Of 150 women who indicated whether they employed an intervention method, 69 (46%) reported using one method of intervention or more. Table 6 shows the frequency of use for each type of intervention method. There was no significant difference found between PFDI-20 scores or number of DRA symptoms in participants who used any method of intervention (p = 0.5 and p = 0.4, respectively). Abdominal support garments were the most common method used. Forty-nine (29.9%) women reported wearing a support at some point during their pregnancy or post-childbirth. There was no significant difference in PFDI-20 scores or number of DRA symptoms in participants who wore an abdominal support during pregnancy and/or the postpartum period compared to women who did not (p = 0.4 and p = 0.4, respectively). Table 7 outlines the timing of use and conditions under which an abdominal support was used. All women who chose to use a method of intervention believed it to be either "beneficial" or "maybe beneficial".
Table 6: Methods of DRA/PFD prevention and/or treatment used during or after most recent pregnancy. View Table 6
Table 7: Timing and conditions of abdominal support use. View Table 7
The number of women who had no knowledge of the use of an abdominal support (n = 94) was greater than those who reported having knowledge (n = 53). Of those who had knowledge, 20 provided feedback about how or where they received their information on abdominal support use. The most common source of information was a friend or colleague (n = 8). A doctor or healthcare provider (n = 4), social media (n = 4), or the internet (n = 4) were other, less reported sources of information.
The primary objectives of the present study were to identify any potential discrepancy between the prevalence of symptoms versus diagnoses of DRA and/or PFD in recent mothers; analyze characteristics that influence occurrence and severity of DRA and PFD symptoms; describe the consequences of these disorders; report the use of different intervention methods and their perceived benefit and compare DRA and PFD symptoms between women who used an intervention method and those who did not; and finally to assess mothers' knowledge of abdominal support garments as an intervention method of DRA and PFD.
In regard to our first objective, data demonstrate a considerable difference between the number of women who reported having symptoms and those who received a diagnosis (DRA: 122 women reported at least one symptom, 11 were diagnosed; PFD: 150 reported symptoms of PFD, 8 were diagnosed). This discrepancy is likely multifactorial and does not appear to be related to the number or severity of symptoms. The most likely reason for under diagnosis of either condition is lack of assessment on the part of the healthcare provider, however since the survey did not include questions related to if and how women were assessed by their healthcare providers, this represents a limitation to the current study. It is possible that many women do not bring these concerns to the attention of the healthcare provider as such, the subsequent assessment of the condition is not performed. In addition, the criteria for DRA diagnosis can vary and it is unclear what diagnostic criteria, if any, individual medical professionals use. This observation is consistent with other research [36]. Normative values for inter-recti distance (IRD) before, during, and after pregnancy vary depending on the location of the measurement along the linea alba, but also vary within each location. After examining 150 nulliparous women, Beer, et al. concluded that a normal width of the linea alba at 3 cm above the umbilicus and 2 cm below the umbilicus could be any measurement up to 2.2 cm and 1.6 cm, respectively [37]. Rath, et al. determined the definition of pathological DRA to be any width greater than 2.7 cm at the umbilicus while a maximum width of 2 cm is also commonly used to classify healthy IRD [38]. Boissannault and Blaschak classified DRA as any measurement greater than two finger widths at the umbilicus [39]. We do not know if participants of the present study were diagnosed with DRA based off of any of these standards. It is likely many women go undiagnosed unless she specifically brings attention to these issues with her healthcare provider, as such, most participants have likely never been assessed for DRA regardless of the method and criteria used.
Because the muscle bellies of the rectus abdominis are inevitably going to stretch and separate during pregnancy, the IRD of pregnant and parous women may be considered "normal" at wider measurements than nulliparous women. After examining 84 primiparous women, Mota, et al. concluded that the 20th - 80th percentiles at gestational weeks 35-41 ranged from 5.4 cm to 8.6 cm at 2 cm above the umbilicus and had lowered to 1.7 cm to 2.8 cm at 6 months postpartum [40]. Based on the definition of pathological DRA as 2.7 cm at the umbilicus, women in the 20th-80th percentile fall well into the "diagnosable range". Yet in the present study, out of those who were diagnosed with DRA, only 4 women received their diagnosis while pregnant. Mota, et al. found that all women had DRA by 35 weeks gestation and a wider than normal IRD continued in 39.3% of these women through 6 months postpartum [16]. Similarly, Made reported that more than 60% of women affected by DRA during pregnancy were also affected puerperium (within six-weeks post-childbirth) [20].
Another primary objective of the present study was to quantify number and severity of PFD symptoms among postpartum women and the prevalence of formal PFD diagnosis. Although almost all women reported PFD symptoms, as measured by the PFDI-20, only 8 had ever received a formal diagnosis. Furthermore, PFDI-20 score did not predict diagnosis status. Although other research indicates that maternal age, delivery method and [11,41,42] are potential risk factors for pregnancy-related PFD, we found no significant differences when comparing these variables between women in the top 25% and bottom 25% of PFDI-20 scores or between those who received a medical diagnosis and those who did not. PFD includes a spectrum of clinical disorders such as urinary and fecal incontinence, sexual dysfunction, pelvic organ prolapse (POP), and general pelvic pain. A system of basic evaluation followed by diagnostic tests has been developed to examine a variety of these issues. In theory, with this process of evaluation, more consistency between diagnoses would be expected. Like DRA, misconceptions about PFD and reluctance to communicate the presence of symptoms with the healthcare provider likely interfere with the application of and appropriate timing of care. Unfortunately, multigravid women whose PFD has not been addressed during or following previous pregnancies are likely to experience exacerbated symptoms that may become more challenging to correct [12]. The same is true for women with DRA. Consistent with other research [42,43] our data does show significant differences in the age and parity of women who reported experiencing ≥ 2 DRA symptoms compared to those with ≤ 1 symptom. This information highlights the need for early DRA and PFD preventative care and treatment.
The next objective was to describe the use and usefulness of DRA and/or PFD intervention methods, specifically abdominal support garments. Conservative methods of prevention and treatment (i.e. therapeutic exercise and KT taping) are becoming more common and better studied. In the current study, all women who chose to use any type of intervention method during the childbearing process (n = 69) reported that it was either "beneficial" or "maybe beneficial". Using an abdominal support garment is becoming more popular and was the most common intervention method employed among our participants (n = 49). In general, current literature advocates for the use of an abdominal support belt during the childbearing process for pregnancy- and childbirth-related issues. Wearing an abdominal support may reduce pregnancy-related symphyseal pain and back pain during pregnancy [27,29,30], as well as help mothers regain functionality and strength after childbirth [44]. Our findings indicated that wearing an abdominal support made no significant difference on the number of DRA symptoms reported or PFDI-20 scores. However, it is possible that use of an abdominal support improved DRA and/or PFD symptoms leading to less reported symptoms and lower PFDI-20 scores. Because there has not been a valid or reliable survey created to measure the severity of DRA, our study does not account for DRA severity beyond counting the number of DRA-related symptoms a woman experienced and represents a limitation to the current study. It could be that women who wore an abdominal support experienced less severe symptoms than those who did not. More research is needed to support and explore this possibility.
Another study objective was to outline mothers' knowledge of abdominal support garment use. No matter the source of knowledge, 47 out of the 53 women who knew about the option to wear an abdominal support chose to wear one either during pregnancy or after childbirth. This implies that providing education could be enough to encourage general proactivity. To our knowledge, no other study has sought to identify the source/s of education on the use of an abdominal support garment during pregnancy or the postpartum period and only four participants of the current study specified that their healthcare provider provided information. For safety and efficacy, it is important that medical advice, such as that pertaining to the prevention/treatment of DRA and PFD, comes from a medical professional who understands the patient's personal situation. With our findings on the occurrence and consequences of DRA and PFD symptoms, it could be expected that more than four women would have received education from their healthcare provider.
Use of a self-reported, unvalidated survey is a significant limitation of this study. While the reliance on self-reported feedback can offer pragmatic and original insight, it is inherently vulnerable to reporting inaccuracies and without validation data, evaluation is susceptible to personal assumption/biased interpretation. As well, while useful for guidance of prospective research, observational studies have limited ability to pinpoint causality. Therefore, our intention is not to promote specific health practices but to bring attention to potential shortcomings or provide the framework for future hypotheses.
Our findings indicate a high prevalence of DRA and PFD symptoms among postpartum women with disproportionate medical diagnoses of these disorders. This needs to be further addressed within the medical community. The need for standardized diagnostic criteria for DRA and PFD is imminent. Unclear diagnostic criteria hinder a health practitioner's ability to adequately meet the needs of a mother experiencing DRA and/or PFD. As well, healthcare providers should be accountable for providing the most up-to-date information of DRA and PFD treatment methods and our findings suggest this is currently not the case. Our data also indicate many women are exploring prevention and treatment options on their own with abdominal bracing/support being the most common choice. Although all women in the present study who used some form of treatment or prevention reported it as "beneficial" or "maybe beneficial", future research should quantitatively and objectively evaluate the usefulness of conservative prevention and treatment methods. Future research should examine the healthcare providers' knowledge of DRA and PFD symptoms and consequences, diagnostic criteria, and prevention and treatment options.
Proper function of the abdominal-pelvic region is important for the maintenance of and return to everyday activities during pregnancy and after childbirth. Compromised strength and coordination, trunk and pelvic instability, lower back pain, and risk of injury are only a few of the consequences of pregnancy-related muscular deficiencies, such as DRA and PFD. As well, these issues interfere with a woman's ability to exercise during and after pregnancy, sexual function, the completion of everyday tasks, and, consequentially, mental and emotional wellbeing. Data from the present study suggest most postpartum women experience symptoms of DRA and PFD without receiving diagnoses or education on prevention and treatment of these conditions from their healthcare providers. Existing literature suggests the usefulness of conservative interventions methods, specifically abdominal support garments. Within this study, use of an intervention method did not appear to influence diagnosis of either disorder, severity of PFD, or number of DRA symptoms. It is important that future research better explores conservative intervention options. Healthcare professionals should educate themselves and their patients on available interventions for these disorders to ensure optimal physical and mental postpartum health. As well, comparing the top 25% and bottom 25% of PFDI-20 scores and the women with ≤ 1DRA symptoms to those who reported ≥ 2DRA symptoms highlighted inconsistencies between diagnoses. Criteria for diagnosis of DRA and PFD needs to be standardized and the assessment of these disorders by the healthcare provider should be routine practice. It is important to close the gap between intervention and symptom experience.
A special thanks is extended to Dr. Camille Thomas. Your expertise and experience are invaluable. Thank you for making the time to review this work, your efforts are not taken for granted. Of the many people who deserve a vote of thanks for their role in the completion of this study, I also want to extend my heartfelt appreciation for those who serve on the staff at Southern Utah University. Thank you all for creating an environment that so fluidly integrates foundational knowledge and progressive creativity within the world of academia.