We characterize the evaluation and initial management of patients with vulvar pruritus, including elements of history-taking, physical examination, laboratory testing, and treatments. We propose an algorithm for approaching this common clinical problem in a systematic way.
A retrospective chart review of patients with vulvar pruritus who presented to Gynecology or Vulvology Clinic at Parkland Health and Hospital System in 2012 informed this descriptive study.
A total of 46 patients aged 19 to 70 years presented with a primary symptom of vulvar itching, of which 41% had additional irritative vulvar complaints. The average duration of symptoms was 24 months; 67% had used at least one self-treatment unsuccessfully prior to their visit. Only 13% of patients received a non-genital skin examination; 46% received a vaginal culture, and 20% underwent vulvar biopsy. The most common diagnoses were "nonspecific" (39%), and "dermatitis" (22%). The most common treatment prescribed was a topical steroid (78%). Vulvar skin care counseling was documented for 67% of patients. At 18 months, 46% were lost to follow up and of those who returned, 48% reported resolution of initial vulvar symptoms.
The assessment and treatment of vulvar pruritus is variable. An algorithm for the evaluation of this common clinical complaint is proposed.
Vulvar itching, Vulvar irritation, Vulvar pruritis
DNA: Deoxyribonucleic Acid; ICD-9: International Classification of Diseases, 9th Revision; HRT: Hormone Replacement Therapy; PHHS: Parkland Health and Hospital System; VI: Vulvar Irritation; VP: Vulvar Pruritus, CG/CT: gonorrhea/Chlamydia
Vulvar pruritus (VP), along with other symptoms of vulvar irritation (VI), is a common complaint for which women present to obstetrician-gynecologists and other primary care providers. In addition to itching, VI includes a sensation of irritation, chafing, pain or burning, for which women commonly self-treat with increased washing and over-the-counter hygiene or medicinal products. With a $3 billion feminine care product industry, women have become regular users of products that contain known vulvar irritants [1-5]. Paradoxically, products meant to treat VP/VI can cause vulvar dermatitis and worsen preexisting symptoms [6]. While the exact prevalence of vulvar dermatitis is unknown, it has been shown to occur in up to 20 to 64% of patients with chronic vulvar symptoms [7,8]. It appears that both contact and irritant dermatitis play more significant roles than infection in the etiology of vulvar complaints [4,5,9,10].
Despite being common, vulvar symptoms can be challenging both diagnostically and therapeutically due to a lack of a standardized clinical approach. Additional obstacles in the management of VP/VI include the fact that no one specialty claims or prioritizes vulvar disease, and evaluation of these complaints is not always included in training programs [5,11]. While a small amount of expert opinion and recommendations are available, there are no widely practiced or standardized guidelines for clinicians. Additionally, there is little data regarding the relevance of personal hygiene habits and their impact on vulvar disease, and a targeted history to elicit these behaviors is not consistently obtained [12]. Moreover, vulvar dermatoses can be difficult to recognize clinically as findings on exam may be subtle [5,13]. We suspected that both the assessment and management of patients with vulvar pruritus and related symptoms are inconsistent at our own institution, and this may be the case elsewhere. The lack of a systematic approach likely contributes to delayed diagnosis, multiple clinical visits, and patient or physician frustration. We characterize patients presenting with VP and other VI symptoms in a specialized clinic setting, describe provider approaches to patients with these complaints, and propose an algorithm (Appendix) to guide the evaluation and initial management based on these findings [14,15].
With Institutional Review Board approval from the University of Texas Southwestern Medical Center, we performed a retrospective chart review of all female patients 18 to 80 years of age who presented to Parkland Health and Hospital System (PHHS) from January to December, 2012 and whose charts were coded with ICD-9 698.1: pruritus of genital organs. Of these patients, we selected those who presented for an initial visit to the general Gynecology Clinic or the specialized Vulvology Clinic within the Gynecology Clinic. Charts were reviewed to confirm that the diagnostic code pertained to an actual vulvar complaint. We tabulated demographic and historic information including age, symptom duration, presence of additional irritative symptoms (irritation, burning, or pain), whether associated vaginal complaints (including discharge) were present, as well as the use of any self-treatments prior to the initial visit. We recorded whether the provider questioned the patient specifically regarding vulvar hygiene habits. Elements of physical examination were recorded including whether the patient received targeted vulvar, vaginal, non-genital skin, and oral mucosa exams. Any testing obtained was recorded including saline wet prep of vaginal secretions, vaginal fungal or aerobic culture, gonorrhea and Chlamydia DNA polymerase testing, and vulvar skin biopsy. We tabulated up to three consecutive treatments each patient received and whether the patient was counseled regarding vulvar skin care recommendations as part of management. The presumptive clinical diagnosis was recorded as well as whether the diagnosis changed by 18 months of surveillance. Charts were also reviewed to determine the number of additional visits the patient had for the same complaint by 18 months of follow up, and whether their symptoms were persistent, improved or resolved at their latest visit. Chart abstraction was performed by two of the authors (SLB and AAL) with reconciliation of any discrepancies by repeat, joint chart review. Analysis of the selected parameters was performed using simple descriptive statistics.
During 2012, a total of 1,175 female patient visits at PHHS were coded as ICD-9 698.1: pruritus of genital organs; this included all outpatient and Emergency Department encounters. Of these patients, only 123 patients were seen in the Gynecology or Vulvology Clinics. Patients whose vulvar complaint was not the primary purpose of the visit, who had a specifically vaginal complaint, or who were not seen for an initial evaluation (i.e. surveillance visits only) were excluded (n = 77). Information was tabulated for the remaining 46 patients seen for initial evaluation of a vulvar complaint. The average age of these patients was 46 years with a range of 19 to 70 years. Patients were seen in the general Gynecology Clinic (22%) or a specialized Vulvology Clinic (78%) at PHHS. Symptom duration prior to presentation ranged from 1 to 120 months, with an average of 24 months. Concurrent additional complaints of vulvar burning, pain, irritation, or vaginal discharge were reported in 41% of patients while 30% also reported vaginal itching. Inquiry regarding vulvar hygiene habits such as methods of genital cleansing, soaps and/or laundry detergents used (names, amounts, frequency of use) was documented for 70% at initial patient encounters.
For 91% of patients, there was documentation of prior self-treatment; of these, 67% of patients used one, 25% used two, and one patient (4%) used three products before initial presentation. The most commonly used self-treatments were topical anti-fungals (36%), topical steroids (29%) or topical estrogens (14%) acquired previously (Table 1). Regarding physical examination, all patients received a vulvar examination by unaided or magnified inspection, 96% underwent a vaginal speculum examination and 13% underwent a documented non-genital skin examination. During initial evaluation, testing included a saline wet prep of vaginal secretions for 65% of patients, an aerobic vaginal culture for 46%, gonorrhea/Chlamydia testing for 46% and a vulvar biopsy for 20% of patients.
Table 1: Treatment(s) used by patients with complaints of vulvar itching prior to their initial visit. View Table 1
The most common initial clinical diagnoses were non-specific, including a restatement of patient symptoms (39%), irritant or contact dermatitis (22%), or specific vulvar dermatoses including lichen sclerosus, lichen planus or lichen simplex chronicus (17%) (Table 2). Of note, for 7% of patients, providers were unable to distinguish if a patient's symptoms were the result of a dermatitis or Candida. Patients received information regarding recommended vulvar care measures in the form of counseling and/or a printed handout at 67% of initial encounters. Approximately 87% were prescribed at least one treatment during their initial evaluation; of these, 33% received two treatments and 2% received three. The most commonly prescribed treatments were topical steroids (78%), topical anti-fungals (20%) and topical lidocaine (10%) (Table 3).
Table 2: Clinical diagnosis at the patient's initial visit. View Table 2
Table 3: Treatment(s) prescribed by providers at the patient's initial visit. View Table 3
Within 18 months, 54% of patients had encounters for vulvar symptom reassessment. Of these patients, 11% received a change in diagnosis. Of the 9 patients who underwent vulvar biopsy, 8 had a histologic diagnosis consistent with their clinical diagnosis; four showed lichen sclerosus, four demonstrated findings consistent with contact or irritant dermatitis, and one was consistent with a hidradenoma papilliferum, a benign apocrine tumor. Patients had an average of two return visits (range 0 to 8) for complaints of vulvar itching in the following 18 months. At 18 months, 20% of patients experienced recurrent or persistent symptoms, 32% had improvement, and 48% of patients reported resolution of their symptoms.
Complaints of vulvar itching and/or irritation, particularly itching, are common and affect a wide age range; the duration of symptoms at presentation is highly variable. They often lead to multiple outpatient visits for evaluation and treatment. Over 1,100 visits in one year to our hospital system were related to such vulvar complaints. A detailed, focused history and knowledge of the common causes of vulvar irritation inform the proper diagnosis and management of these patients. In our experience, patients often assume that their symptoms are due to inadequate hygiene or infection, triggering escalating hygiene practices that in turn exacerbate irritation and lead to ineffective self-treatment. This study is consistent with previously published investigations demonstrating that patients frequently misdiagnose themselves, leading to the unindicated or ineffective use of nonprescription anti-fungals, anti-itch creams, and topical antibiotics [16]. For example, more than a third of our patients self-treated with anti-fungals prior to presentation. Without a careful history, these potentially contributory behaviors can be overlooked and go unaddressed. Symptom duration is often prolonged, with an average time of 2 years reported by our patients. Our study confirms that the majority of vulvar itching and related complaints are due to noninfectious etiologies, and treatment with topical steroids are most often prescribed [10] followed by antifungals. Aerobic cultures to identify fungal vulvovaginitis not detected by vaginal wet prep did not change the diagnosis in any case at initial encounter. Likewise, vulvar biopsies failed to alter the initial diagnosis. This implies that these two tests can be reserved for subsequent evaluation of refractory cases.
The strengths of our study include the careful and adjudicated data collection completed by two of the authors. The restriction of patients to those seen under one specific diagnostic code commonly used at our institution allowed focus on patients presenting specifically for the vulvar symptoms addressed by this study. Limitations include a relatively small number of study subjects. The inclusion of patients within only one diagnostic code for genital pruritus likely excluded a much larger number of patients coded for other specific vulvar complaints such as vulvar irritation, pain, and burning, or as having vaginal, vulvovaginal, or other coexistent gynecologic complaints. Indeed, approximately two-thirds of patients coded for vulvar pruritus were eliminated from the study due to miscoding of the primary complaint in the electronic medical record. Limiting this review to visits within the Department of Gynecology (including a specialty clinic for vulvar complaints) surely underestimates the number of visits to all types of providers for vulvar pruritus and irritation as well as the variation in evaluation and management that patients experience within this hospital system. Indeed, approximately ten times more visits coded as vulvar pruritis took place outside the Gynecology or Vulvology Clinics at PHHS. Treatments beyond the maximum of three per patient were not recorded during the study time period. Furthermore, a co-existing diagnosis of diabetes was not elicited. As such, the degree to which this affects patient symptoms and number of clinic visits was not studied, however this likely does contribute to persistent symptoms of vulvar pruritis, especially via infectious agents.
The clinical assessment and monitoring of patients with vulvar pruritus and additional irritative vulvar complaints is variable, even in a specialized clinical setting. The standardization of clinical evaluation and initial management of this common complaint is warranted in order to study best approaches to initial evaluation and management. A clinical algorithm is proposed in the Appendix that follows as a potential move toward this goal, encouraging a thoughtful, detailed, organized approach that will more efficiently and accurately aid the diagnosis, management, and study of vulvar pruritus and other irritative complaints (Figure 1).
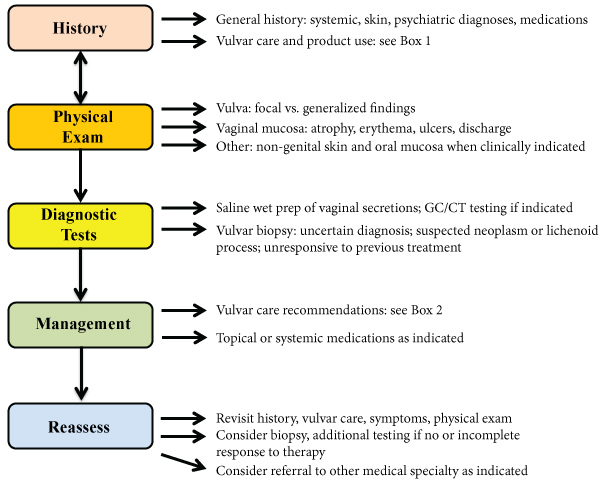 Figure 1: Proposed algorithm for the evaluation and initial management of patients with irritative vulvar symptoms (Box 1 and Box 2).
View Figure 1
Figure 1: Proposed algorithm for the evaluation and initial management of patients with irritative vulvar symptoms (Box 1 and Box 2).
View Figure 1
The authors have no conflicts of interest to declare. The authors have no financial support disclosures.