Background: In Ethiopia, a large proportion of girls start having children at a young age. The primary cause of maternal and child morbidity and mortality, as well as the cycle of poverty and illness, is teen pregnancy.
Objective: To assess prevalence and factors associated with teenage pregnancy among HCG Positives at selected Governmental Health Centers of Addis Ketema sub city, Addis Ababa; Ethiopia; by August, 2023.
Method and materials: A health facility based cross-sectional study that employed quantitative research methods. Total of 287 in public health facility teenage girls aged 13-19 years were selected using multi-stage sampling technique. Interviewer administered questionnaire was used to collect data from participants. Analysis of data was performed using EPI info version 7.2.5.0 and exported to SPSS version 20 for descriptive and logistic regression analysis.
Results: The proportion of teenage pregnancy among respondents in Addis Ketema sub-city governmental health centers was 81(28.2%) with a 95% CI. The proportion of teenage pregnancy among respondents in Addis ketema sub-city governmental health centers was 81(28.2%) with a 95% CI. Those teenagers whose first intercourse is below 17 years are 8.8 times more exposed to pregnancy than and those 18 years and above (p-value = 0.02, AOR = 8.8, 7.06-52.7). Those teenagers not used family planning are 3.02 times more likely to get pregnant than those used (p-value = 0.04, AOR = 3.02 (2.33-4.250).
Conclusions: Magnitude of teenage pregnancy not used family planning, age of first sexual intercourse under 17 age were more exposed to pregnancy to have significant association with teenage pregnancy. The results indicate that encouraging the use of contraception, avoiding young marriage, and highlighting the negative effects of adolescent pregnancy are essential.
Teenage girls, pregnancy, Addis Ababa
AARHB: Addis Ababa Regional Health Bureau; AOR: Adjusted Odds Ratio; AYH: Adolescent and Youth Health; CI: Confidence Interval; EDHS: Ethiopia Demographic and Health Survey; HC: Health Center; OR: Odds Ratio; WHO: World Health Organization
Teenage pregnancy is defined by the United Nations Children Fund (UNICEF) as a pregnancy in a girl between the ages of 13 and 19 [1]. Above 90% of births occur in low- and middle-income countries [2]. According to data, 529,000 women worldwide may pass away each year as a result of complications associated with pregnancy and childbirth [3]. Over the world, teen victims of early marriage suffer from STIs, female genital mutilation, starvation, anemia, infertility, sexual and gender-based abuse, unintended pregnancies, and illegal abortions [4]. Also, A major health concern in teenage pregnancies is nutritional anemia during pregnancy [5].
Due its consequences teenage pregnancies are viewed as a death sentence in several nations. WHO’s a advise for lowering early marriage are supported by 21 studies, project reports, and expert panel recommendations. High prevalence of teenage pregnancies in low-income [6-8].
The WHO views teenage pregnancies as high-risk pregnancies because they are linked to unfavorable outcomes for both mother and foetus [9]. Adolescent pregnancy is highly correlated with early sexual activity [10]. Teenagers experience is 1/4 th of all the incidence of negative pregnancy and childbirth outcomes [11]. Teenage pregnancy can lead to depression, poor school performance, a lack of attachment to the labour force, low earnings [12]. Furthermore, Girls at this age are not mentally or physically prepared to take on the obligations of parenting [13]. Adolescents account for roughly one-sixth and one-fourth of the populations in the world and Sub-Saharan Africa (SSA), respectively [14]. Premarital intercourse pregnancy and early marriage are two factors that may contribute to high teen pregnancy rates [15].
Pregnancy negatively impacted educational levels than their rivals in terms of career [16]. Rates of teenage pregnancy and usage of modern contraceptives are among the lowest in Tanzania, Nigeria, and Ethiopia [17]. Adolescent pregnancy is linked to significant socioeconomic difficulties [18]. Teenagers are more likely than adults to have unsafe abortions, which causes more women to die [19]. Both in developed nations and low- and middle-income countries, excessive risk behavior and substance use frequently coexist also Most married are before 18 years and didn't attend school [20,21].
Adolescent pregnancies in Sub-Saharan Africa are influenced mostly by health service related factors [22]. Global Strategy focuses teenagers as being essential to achieving Sustainable Development Goals [23]. Misunderstanding about sexual and reproductive health (SRH), particularly among adolescents, inhibits efforts to make healthcare services more accessible to people of low and middle income [24]. Low birth weight, pre-eclampsia or eclampsia, premature delivery, and maternal and perinatal mortality, are likely to occur in adolescent pregnancies [25].
UNFPA analysis estimates that 14 million teenagers between the ages of 15 and 19 give birth each year, with more than 90% in poor nations [26]. Unmarried teenage females are commonly the objects of social isolation [27]. Guidelines for preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries were released by the WHO to improve health professionals awareness [28].
Significant progress on sexual and reproductive health since the 1994 International Conference on Population and Development (ICPD), Agenda 2063, and the Sustainable Development Goals (SDGs) were established [29].
Sub-Saharan Africa, had the highest rate of teen pregnancies in the world in 2013, accounting for more than half of all births [30]. Women between the ages of 15 and 19 account for one-fourth of the estimated 6 million unsafe abortions performed in Africa each year [31]. The factors in Africa are a lack of sexuality education, ineffective use of modern contraceptives, cultural obedience, females' socioeconomic dependence on males, and peer influence [32,33]. It needs a policy addressing teenage pregnancies in Africa due to effects of the high teenage pregnancy rate in Africa [34].
In Ethiopia with the highest rates occurring in the Afar and Somalia areas [35]. Studies show regions high prevalence Afar 23%, Somalia 19% and Oromiya 17% [36]. Each year, the majority of adolescent girls in Ethiopia's rural areas are pregnant outside of marriage [1].
To assess prevalence and factors associated with teenage pregnancy at selected Governmental Health Centers of Addis Ketema sub city, Addis Ababa; Ethiopia; 2023.
➢ To determine prevalence of teenage pregnancies in Addis ketema health cent
➢ To find out which factors mostly associated with teenage pregnancies.
The capital of Ethiopia is Addis Ababa. According to the 2007 census, it has a total population of 3,384,569, making it the largest city in the nation by population. The city has experienced a rapid annual population increase in recent years, and as of 2017, the population was getting closer to 4 million. Ethiopia's capital city has 527 square kilometers of land.
Almost 5,165 people are thought to live there in every available square kilometer. According to the population figures from the most recent census, there are more women than men living in Addis Ababa. The capital city has the highest adult literacy rate of any city in the nation, with over 93% for men and around 80% for women. With a population of 480,373 Addis Ketema Sub City is about 7.41 KM2 (2.86 sq. miles) in size [25]. The sub-city includes 14 health centers, and the study will be held in three of them that were chosen by lottery.
The study was conducted In June 1-June 30/2023.
Institutional based cross-sectional study was conducted at public health centers in Addis, Ketema Sub city, Addis Ababa Ethiopia.
All adolescent women in Addis Ketema Sub City during the study period.
All pregnant teenagers who visited the selected public health facilities in Addis Ketema and Addis Ababa during the study period.
Those teenage girls came to AYH clinic in selected public health Centers.
Inclusion criteria: All pregnant teenagers whose age is between 13-19 years who visited the selected public health facilities in Addis Ketema and Addis Abeba during the study period.
Exclusion criteria:
➢ Severely ill
➢ Severe Mental Health disorder
Outcome variable: Teenage pregnancy served as the study's outcome variable.
Independent variable:
Socio demographic traits
➢ Age
➢ Marital status
➢ Occupation
➢ Educational Status
Factors affecting families
➢ Family Income
Obstetrics history related factors
➢ Number of pregnancies
➢ Number of abortions
➢ Age of first sexual intercourse
➢ Family planning usage
➢ Condition of pregnancy
➢ Reasons declined to use family planning if not used
Teenage pregnancy/Adolescent pregnancy: A pregnancy who believe that they are pregnant and confirmed by a health care providers in a girl between the ages of 13 and 19 [1].
Early sexual intercourse: Is practicing of sexual intercourse before 18-years-old [37].
Peer pressure: Is when you do something because you want to feel accepted and valued by your friends. Peer influence can be positive or negative [38].
Unplanned pregnancies: A pregnancy that is either unwanted, such as the pregnancy occurred when no children or no more children were desired [39].
The sample size was calculated using Leslie Fischer’s formula for population > 10,000, the formula for sample size calculation that took the following assumptions into account: 13% of teenage pregnancy in Ethiopia based on 2016 EDHS, 5% level of significance (= 0.05), and 5% margin of error (= 0.05). The final sample size was adjusted to 287 by adding 10% non-response rate and accounting design effect.
The sample size was required to estimate a population proportion with a given level of precision and becomes as below:
Z = 1.96 reflects the confidence level
N = total population size
P = prevalence of teenage pregnancy in Ethiopia (13%)
d = degree of accuracy expressed as proportion (0.05)
Deff = 1.5
By using the above formula the sample size become 261 and by adding the non-response rate of 10% the final sample size becomes 26 + 174 = 287
Stage 1: A Town which is Capital city of Ethiopia was selected using a one-time ballot.
Stage 2: A sub-city was selected using simple random sampling from existing eleven.
Stage 3: Public health facilities were systematically selected within the Selected sub-city.
Participants of the study were all who fulfill eligibility criteria and signed consent to participate in the study in the specified study period.
The information was be gathered by five B.S.C. nurses under the guidance of a public health official. Throughout the two days of data collecting training, the Supervisor and data collectors learned how to conduct interviews and ascertain eligibility requirements.
The quality of the data was ensured by careful planning, questionnaire translation and pretesting, and effective data management. The data was periodically reviewed throughout the data collection process, and at the end of each day, the collected questionnaires was examined for consistency and accuracy.
The questionnaire-based information was entered into EPI info version 7.2.5.0 and examined using SPSS version 25. All variables related to the objectives of the study were having their frequencies and percentages calculated after the data have been cleaned. The link between the independent and dependent variables was examined using binary and multiple logistic regressions, and the odds ratio with a 95% confidence interval calculated. In binary regression, variables with p-values less than 0.25 was be subjected to multiple logistic regression. Substantially connected variables were ultimately defined as those in the multivariate analysis with a p-value of 0.05 or less.
Before the start of data collection, the Rift Valley University Lancha Campus Ethics Review Committee's ethical approval was given. Addis Ababa Public Health Research and Emergency Management Directorate granted ethical clearance. After receiving ethical approval, the administrative body of the Addis Ketema Sub-City Health Office was contacted to request permission to perform the study. To secure verbal agreement from all eligible participants in the study, an information sheet was created and distributed to them. All participants were made aware of the study's objectives, and they all willingly agreed to participate. To maintain secrecy during the course of the study, participants' names were not requested; instead, a code number was utilized. Also, to preserve anonymity, written informed consent was collected from every study participant. Participants were asked for their consent prior to the interview. Participants' names were not sought or recorded Girls under the age of 18 were also asked for their assent prior to the interview to sign. Participants' names were not sought or recorded.
Among 287 participants response rate was 100%. From total study participants majority 64.8% of respondent were 19 years of age group. The mean age of pregnant teenagers is 18.6 and the median age is 17. Most common occupation group seen was housewife 127(44.25%) and most of them are married 239(83.3%). Majority Teenagers pregnancy was Age 18 and above of first intercourse 51(62.96%). Majority of teenagers were with educational status college and above 111(38.7%). When we see occupation of teenagers most of them are house wives 127(44.25%). Those teenagers with family monthly income the least were <= 5000 etb 6(2.1%) and the highest 16334-27667 165(57.5%) (Table 1).
Table 1: Descriptive analyses of socio-demographic characteristic of Teenager girls. View Table 1
Those teenage girls majority felt Happy 65(80.3%) the latter were unhappy 9(11.1%). Pregnancy outcome those delivered were 22(79.4%) and aborted 59(20.6%) from all pregnancies planned ones were 65(22.6%) and unplanned is 14(4.9%) (Table 2).
Table 2: Sexual and reproductive health characteristics of participants. View Table 2
Large number of teenagers first sexual intercourse age were 18 years and below 182(64.4%). Most of teenagers family income is 16334-27667 etb 165(57.5%) and the least one <= 5000 etb. Those teenagers living with husband are majority accounting 235(81.9%) secondly living alone 24(8.4%) and those family planning not used due to peer influence were 11(3.8%) due to Husband and family influence were 45(15.7%) (Table 3).
Table 3: Descriptive analysis Teenage girls pregnancy Individual and Parent factors. View Table 3
From the total respondents 81(28.2%) of teenage girls had pregnancy and 206(71.8%) of them had no pregnancy (Figure 1).
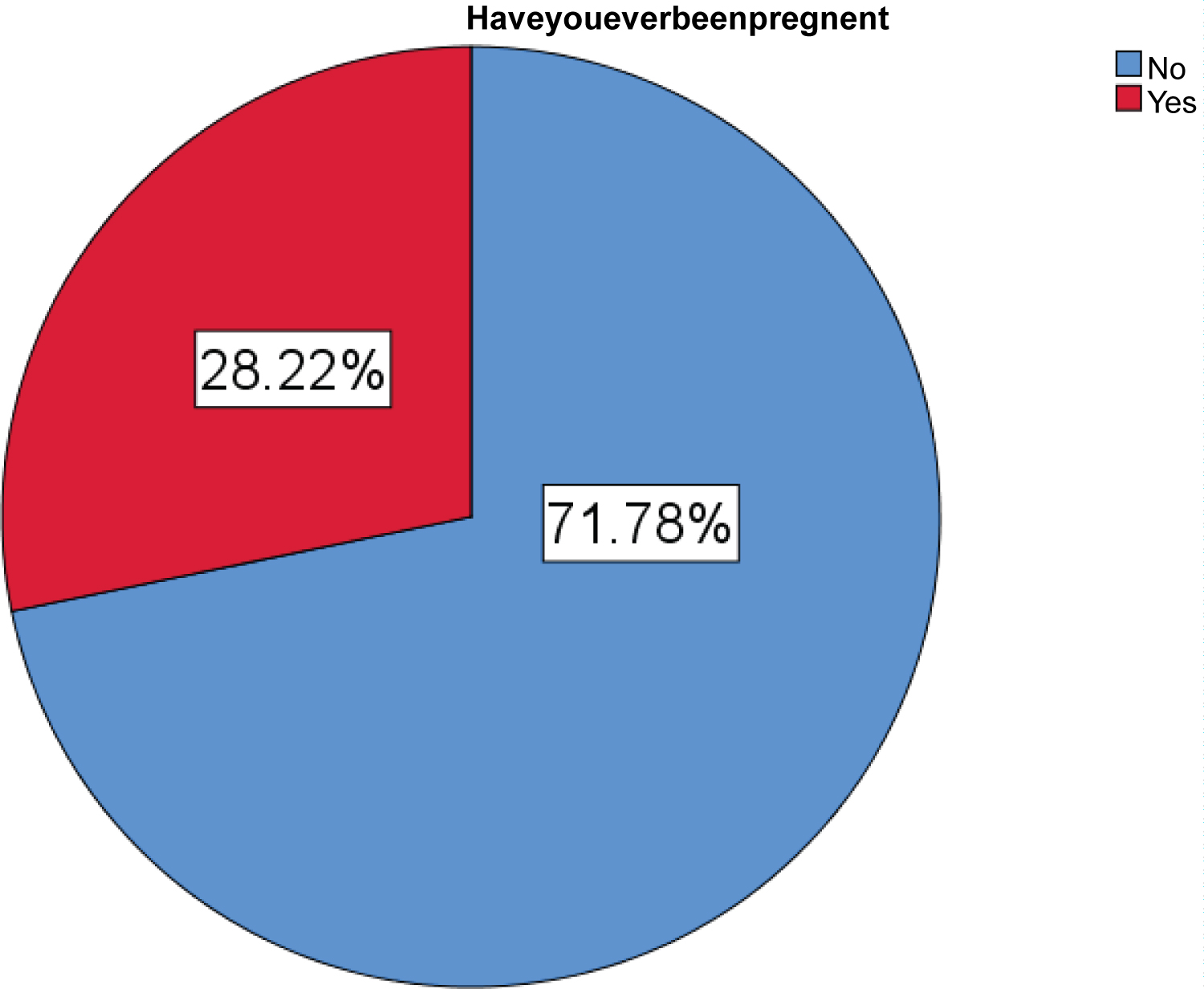 Figure 1: Teenage pregnancy prevalence.
View Figure 1
Figure 1: Teenage pregnancy prevalence.
View Figure 1
From socio demographic characteristics age of first intercourse is 17 years and below are 8.8 times more exposed to pregnancy than and those 18 years and above (p-value 0.02, AOR = 8.8, 7.06-52.7). Those teenagers not used family planning are 3.02 times more likely to get pregnant than those not used (P-value 0.04, AOR = 3.02(0.002-4.250) these are statistically significantly variable (Table 4, Table 5 and Figure 2).
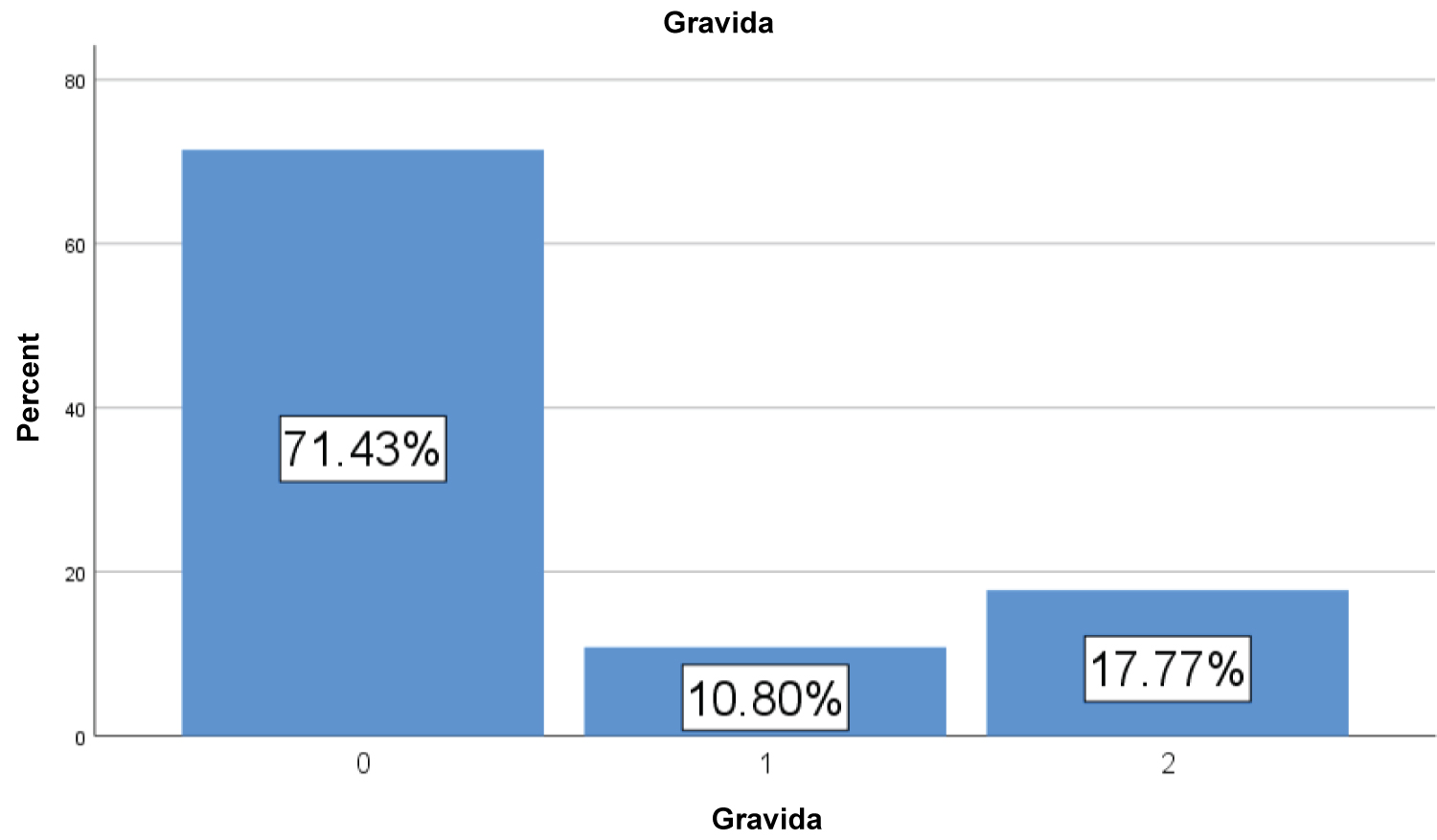 Figure 2: Teenage pregnancy related Data.
View Figure 2
Figure 2: Teenage pregnancy related Data.
View Figure 2
Table 4: Bivariate and multivariate analysis of Socio-demographic factors showing Risk factors among Teenage girls in Addis ketema sub city, Addis Ababa, Ethiopia, August 2023 (n = 287). View Table 4
Table 5: Bivariate and multivariate analysis showing sexual and reproductive health Risk factors among teenage girls in Addis Ketema sub city, Addis Ababa, Ethiopia, August 2023 (n = 287). View Table 5
There were 81 participants who get pregnant in this study 81(28.2%). One of the highest rates of adolescent pregnancies worldwide is seen in South Asia. At 35%, 21%, and 21%, respectively, Bangladesh, Nepal, and India have reported the greatest prevalence of adolescent pregnancy within the region it was Due to a lack of thorough sexuality education and low socioeconomic standing. The conventional social norms that favour early marriage and the limited autonomy of teenage girls reinforce this. This result is lower than Bangladesh but higher than Nepal and India [40].
There were a total of 24 nations from the sub-regions of East, West, Central, North, and Southern Africa. In Africa as a whole, the prevalence of adolescent pregnancies was 18.8% (95% CI: 16.7-20.9), while in sub-Saharan Africa, it was 19.3% (95% CI: 16.9-21.6). East Africa had the highest prevalence (21.5%), while Northern Africa had the lowest (9.2%). Adolescent pregnancy risk factors include, having ever been married (OR: 20.67), not attending school (OR: 2.49). This study is also shows majority of Teenage pregnancy were due to marriage (OR: 1.91) [41].
The result is somehow higher than the research done among high school students in Gondar (23.5%) and Nekemt (21.5%), two towns in Ethiopia. However, the results are in line with the results of research conducted among school-aged teenagers in Nigeria, and the Ethiopian Demographic and Health Survey (EDHS) report from 2011. 24.2% and 28.2%, respectively, were the results of these studies. The gap may be caused by methodological differences: This study only included health facility visiting teenagers, whereas EDHS included adolescents from the community [42].
Married teenagers were more likely than single teenagers to become pregnant. This result is consistent with research from Ethiopia, Nigeria, Uganda, and Ethiopia. This might be because married teenagers started having relationships without having access to or knowledge of family planning options, which increases their risk of getting pregnant. Additionally, only 7.5% of adolescent girls use family planning, despite having a substantial unmet demand (22.5%). Early marriage is one of the most prevalent and detrimental traditional practices in Ethiopia, despite national and international laws that forbid it. According to the EDHS 2016, nearly half (47%) of women were married before reaching the age of 18 [43].
This study shows major factor teenage pregnancy family planning not using due to family and peer influence (AOR = 3.02(2.33-4.250). It is estimated that 14 million unplanned pregnancies take place annually in sub-Saharan Africa, with women between the ages of 15 and 24 accounting for about half of these pregnancies. According to recent data, 21% of adolescent girls in the western or central region of Africa and 18% of adolescent girls in the eastern or southern region had started having children [44].
According to study conducted on Magnitude and its associated factors of teenage pregnancy among antenatal care attendees in Bahir Dar city by 2022 age at first sexual intercourse and not using contraception prior to this pregnancy 5.22(3.243, 11.675)] were significantly associated with teenage pregnancy this is in line with this study in both cases of predictive variables [45].
Determinants of Teenage Pregnancy in Ethiopia by 2019: Contraceptive use, and reasons for not using Family planning were higher among the cases and were statistically significant [44]. According to study done in Uganda Low use of contraceptives was the most cause of teenage pregnancy by 56% [46].
As strength, the study used data from a nationally representative large dataset, which results in adequate statistical power but it has limitations in that it doesn’t include family or husband educational level and awareness on family planning.
This study showed that there is a high prevalence of teenage pregnancy not used family planning, age of first sexual intercourse 17 and below were more exposed to pregnancy to have a statistically significant association with teenage pregnancy. The results indicate that encouraging the use of contraception, avoiding young marriage, and highlighting the negative effects of adolescent pregnancy are essential.
My special thanks to Addis Ketema sub city and public health centers for their cooperation for data collection and all study participants who give us baseline information for research preparation.
Dr. Faisel Abdo and Dr. Tefera Tezera from Rift valley University participated in data analysis, interpretation, manuscript drafting, wrote the paper, revised the manuscript participate on the data collection and data entry. Dr.Zelalem Negash designed the study edit the manuscript. All authors read and approved the final manuscript.
The authors declare that they have no conflicts of interest for this work.