Simulation is a teaching learning and assessment strategy used in medical education to prepare medical laboratory students for clinical practice. Simulation-based learning is aimed at bridging the gap between theory and practice through the use of innovative teaching strategies and thus it is considered the best alternative teaching, learning and assessment tool in preparing medical laboratory students for practical and professional life. Traditional methods of educating medical laboratory students are no longer sufficient in the present times largely influenced by the emergence of new infections, technology, and multimedia. In general, scarce literature supports the use of simulation to benefit medical laboratory students in areas of knowledge, value, and realism. However, little emphasis has been placed to make application of the method. The aim of the study was to determine the extent of the application of innovative simulation-based medical teaching and learning among staff in selected Kenya medical training campuses offering medical laboratory sciences in Kenya, with a view to improving the application of the simulation strategy. The study employed the census sampling technique. Data collection tools were structured questionnaires, interviews, checklists, and observations which were used for data collection to obtain information from the respondents.
Quantitative data analysis was conducted using the Statistical Package for Social Science (SPSS) software version 22 for windows. Qualitative data was analyzed using content analysis. Both descriptive and inferential statistics particularly the Chi-square test statistics were used in data analysis. P-value was used to test the normality of the spread of the ages. From the findings, 35 (74.5%) of the lecturers were males while 12 (25.5%) were females. The age of the respondents was not normally distributed but had positive skewness of 0.845. The results showed that there was a significant relationship between gender and the age of the respondents, Pearson Chi-Square 0.016 (p < 0.05). The majority of the lecturers, 39 (83.0%) indicated that they understood and defined simulated medical laboratory experiences as both actual and anticipated. The respondents reported that simulation-based teaching and learning enable them to earn continuous professional development (CPD) points. All the lecturers 47 (100%) agreed that the educational validity of simulation-based teaching and learning was one of the factors that shaped their decision to implement simulations. The principals cited issues such as untrained simulator instructor staff in MLS, and lack of adequate infrastructure, as part of the challenges they encountered while implementing innovative simulation-based teaching and learning. From the study, it was concluded that simulation-based teaching and learning were not applied uniformly across the MLS department, indicating a lack of standardization in training hence the knowledge, attitudes, as well as skills acquired by the students before they graduate, were not in line with the public expectation. There is a need for KMTC management to ensure uniform application of innovative simulation-based teaching and learning across all MLS departments and hence standardization in the training of medical laboratory sciences professionals.
Application of simulation-based medical education, Teaching, Learning, Medical laboratory education, Kenya medical training college, Medical laboratory science department, Medical education
Simulation-based teaching and learning have been defined as the “reproduction of some aspect of reality to better understand, manipulate or predict real behaviour” [1]. Other terms associated with simulations include ‘surrogate’ or ‘recreation’ of reality, an activity that mimics reality, a controlled environment, immersive or guided experiences, and fully interactive tasks. Simulation activities comprise techniques rather than technology, a replacement or amplification of real experiences with guided experiences that are often immersive in nature [2,3].
Medical laboratory educational programs have been implemented but given the potential they possess, units/topics/modules contained therein have not been given the attention expected [4].
There has been a lag in classroom learning that has led to the underachievement of goals regardless of inspirational examples of teaching that are innovative. This gap between the idealism of change and the realism that is witnessed in a classroom is attributed to the inaccessibility of resources, low levels of training, and inadequacy in the overall objectivity of the systems. The current systems in medical laboratory education although organized, are still inclined to the traditional or rather conventional measures of achievement. The majority of the students are subjected to lecture- based methodological practices that are deficient of technological advancements [5].
Hence, the question remains; which mitigation measures should be used to redress this persisting conservative approach to preparing medical laboratory health professionals better?
Like other programs such as Nursing and dentistry, medical laboratory science programs are also adopting and showing interest in simulation-based learning experiences for their students which previously was not the case. This has been brought about by the need to decrease reliance on clinical training sites which have not been reliable of late hence the need to shift to simulation [6].
The changing healthcare environment, with the movement of medical care from the traditional hospital setting to ambulatory medicine (medical services performed on an outpatient basis, without admission to a hospital or other facility, e.g. Offices of physicians and other health care professionals, hospital outpatient departments, ambulatory surgical centres, specialty clinics or centres, e.g., dialysis or infusion, Urgent care clinics), has necessitated the ability to provide care in a much shorter period and requires changes in documentation with all information, including both health knowledge and medical records, becoming digital [7].
Medical education has undergone significant changes all over the world because of concerns for the patient safety [8]. Preventable medical errors result in more than 400,000 deaths among American citizens each year and are the third cause of death in the United States, followed by cardiovascular diseases and cancer [9]. Non-fatal iatrogenesis (unintended adverse patient outcome because of a health care intervention) resulted in disability in 3.5 million American patients per year. The major cause of such alarming statistics may be related to the medical education culture characterized by the mere acquisition of knowledge [10].
Many advances have been made in technology and teaching strategies [7]; however, it is still not unusual for medical laboratory students to be taught in a traditional classroom the same way they were decades ago because questions are being raised as to how should the medical curriculum be redesigned to serve the scientific foundations of medicine in the 21 st century [11].
Medical education is rapidly changing, influenced by many factors including the changing health care environment, the changing role of the physician, altered societal expectations, rapidly changing medical science, and the diversity of pedagogical techniques [12]. Changes in societal expectations put patient safety at the forefront, and raise the ethical issues of learning interactions and procedures on live patients, with the long-standing teaching method of “see one, do one, teach one” no longer acceptable [13]. The goals of using technology in medical laboratory education include facilitating basic knowledge acquisition, improving decision making, enhancement of perceptual variation, improving skill coordination, practicing for rare or critical events, learning team training, and improving psychomotor skills. Different technologies can address these goals [14].
Healthcare simulations have been used worldwide to reduce adverse outcomes in patient care settings [15]. In recent decades, globally, nursing instructors have tended to use skills laboratories in training for pre-service nursing students rather than traditional methods due to benefits such as increased self-confidence and competency levels [16]. In the training of medical Laboratory students, there is a need for medical laboratory students to expose live patients to some procedures so that they get the necessary adequate skills [17]. On the other hand, students are obligated to offer optimal treatment and also to ensure their patients’ safety and general well-being. As much as medicine is considered a science, it is also an art and so repeated exposure together with enhanced experience are required to improve skills and the much-needed confidence [18].
In the medical field, simulation finds its origin in antiquity, when models of human patients were built in clay and stone to demonstrate the clinical features of diseases and their effects on humans [19]. An obstetrical mannequin made of a human pelvis and a dead baby was developed in the USA in the 18 th century. This mannequin enabled obstetricians to teach delivery techniques which resulted in a reduction of maternal and infant mortality rates [20]. Historically, animals were used in the training of surgical skills since the Middle Ages throughout modern times [21].
According to Kihuba, et al. [22], the provision of safe healthcare cannot be guaranteed in a majority of healthcare facilities both public and private facilities. In a MoH survey done in collaboration with the World Bank, of the 13 healthcare facilities surveyed, the overall Patient Safety compliance was relatively poor at 97% and less than 1% of the public healthcare facilities and only 2% of private facilities met some minimal standards on Patient Safety further widening the gap as far as quality healthcare to all is concerned.
According to Jha, et al. [23], unsafe and harmful healthcare practices are a major source of morbidity and mortality. World Health Organization [24], estimates that millions of patients are harmed each year due to unsafe medical practices. Medical errors in many healthcare settings result in either temporary or permanent injuries as well as an increased length of hospitalization or in extreme cases the death and disability of the patients.
Most studies on simulation learning have been done in other departments with very little if any being done and documented in the literature concerning medical laboratory science. The public has become more aware of their health needs hence increasing the demand for laboratory services, which also includes the use of technology and techniques that were not available previously. Again, more than 70% of the information a doctor needs to actually treat the patient comes from diagnostic laboratories. This raises the question “Is innovative simulation- based medical teaching and learning applied for the teaching of medical laboratory students? Simulation-Based Learning (SBL) interventions have been under-utilized due to the shortage of well-trained staff and shortage of equipment in resource-limited areas which includes Kenya [25].
New information, new laboratory tests, and new protocols are constantly being added to the laboratory profession and hence adding new content to the curriculum is inevitable [26].
In recent years, budgetary pressures, increasing student enrolments, limited access to laboratory equipment, and extremely expensive clinical simulation laboratory infrastructure have resulted in reduced staff-student contact hours in medical laboratory science education. While this restructuring in resources has been challenging, it has encouraged innovation in simulation-based learning as well as online blended learning [27].
In medical laboratory science education, some of the traditional teaching strategies include traditional lectures, face-to-face learning, laboratory lessons using manual procedures, and assignments/homework. These strategies do not encourage student interaction and independent thinking by the students but the innovative teaching strategies characterized by so many challenges such as the use of expensive equipment and a decreased equipment budget, reduced staffing, experiments involving animal dissection, experiments taking days to months to give results, patients awareness on their personal safety and congestion during students’ clinical experience do encourage student interaction and independent thinking. These innovative teaching strategies utilize recorded lectures; interactive online modules; web-based learning; virtual or simulated learning, mobile device learning (tablet or phone), learning management systems, e-Learning; and learning platforms facilitated through asynchronous internet tools [28]. To address the above issues Appiagyei, et al. [29] recommended the application of innovative simulation-based teaching in training institutions and more so for medical laboratory science students.
The training of the medical laboratory sciences practice in Kenya is regulated by the Kenya Medical Laboratory Technicians and Technologists Board (KMLTTB) which is an agency established by the Act of Parliament No. 10 of 1999. This board plays a critical role in the National Health infrastructure by assuring that medical diagnostic services holistically meet expected standards, from personnel, equipment, reagents to safety requirements. It works with local, regional, international, regulatory and scientific partners to ensure that Kenya’s Medical Laboratory Science Sector is reliable and fully compliant to current and emerging capacities [30].
The workload of medical laboratory officers include; sample collection, reception, preparation, analysis, manage and supervise the removal and destruction of medical laboratory wastes, validation, interpretation and the dispatch of results to the relevant departments and offices, results analysis, carrying out internal/external quality controls in the laboratory to ensure quality and accuracy of results, attending departmental meetings, participating in the ward rounds, keeping an inventory of laboratory reagent and materials needed, used and requested, developing, improving and updating laboratory standard operating procedures [31].
In conclusion, it is not anticipated that innovative simulation-based learning should completely replace the physical presence and hands-on learning in the laboratory. Nonetheless, the study aims at determining the application of innovative Simulation-Based Medical Teaching and Learning in selected KMTC Campuses offering Medical Laboratory Sciences in Kenya. Innovative simulation-based teaching and learning experiences may be effective alternatives when the hands-on approach is too complex for learners in their first year, expensive, or inaccessible due to laboratory constraints in the clinical areas, or the activity is too time-consuming to complete in the laboratory. This innovation can prepare the student for laboratory procedures, promote an enriched and sustainable learning experience.
The current medical laboratory education training system regarding the clinical care of patients in terms of history taking, physical examination, diagnosis, and management in medical schools has been reported to be inadequate by students even after graduation [32]. Not seeing and practicing a number of important diagnoses during training periods could pose a significant knowledge gap which eventually gets carried forward to internship and would eventually affect patient care [33].
Medical laboratory errors emanate from the wide range of mechanical, chemical, biological, and environmental hazards that the laboratory practices involve. These errors affect the delivery of the services in the laboratory as well as the patient management either directly or indirectly. The cause of these errors could be as a result of the training given to the medical laboratory practitioners while in their training institutions [34].
While some of the errors are caused by a lack of or inadequate knowledge and skills among the medical laboratory personnel, others are caused by ineffective equipment used in the laboratories. The levels of training for the medical laboratory technicians/technologists also poses some concern hence, the training as well as clinical and laboratory practice should be adequate enough to enable them handle complex tests in clinical laboratories. These officers need to be equipped enough to reduce the errors to zero or the required levels [35].
Some of the errors as documented include; incorrect patient identification, specimen rejection, proficiency test failure, phlebotomy dissatisfaction. Other errors occur as a result of work overload due to staff shortage caused by unemployment and presence of aged officers working in the laboratories [36]. These medical errors and inadequate confidence, can be observed at the point of care during senior clerkship, internship as well as in employment of nurses, medical laboratory technologists and clinical officers [32], because the traditional hospital-based clinical instruction is observed not to always provide the same type of patients discussed in the classroom [37].
Although simulation-based medical teaching and learning has been integrated in some of the curricula like in Clinical Medicine and nursing among others, its application is unclear, lacking or inadequate in the department of Medical Laboratory Science education or there is lack in its documentation in literature.
There is need to enhance the medical laboratory science course curricular beyond laboratory skills and diagnostic interpretation competency. Incorporating simulation-based teaching and learning in the curricular presents an opportunity to train and produce medical laboratory scientists and technologists with the skill to communicate and work effectively in an inter-professional healthcare team [38].
Traditionally, skill training was “see one, do one” and this was associated with medical errors because of lack of enough exposure even though by then, students were fewer. The scenario seems to be the same to date even after skills laboratory methodology [32], and also to some extent, because improved health care systems and information technology have reduced the length of hospital stay for patients thus preventing students to have sufficient time to understudy a particular disease condition and care with real life patients. The problem has been compounded by the very many students being trained currently versus constrained resources. Effective teaching strategies and innovative approaches are critical in producing a competent all round health care worker in an ever-changing medical field. The use of simulation by computer and internet in skills training is moving in tandem with technology [39].
It has been reported that simulations can increase both learning outcomes and competence levels in the medical laboratory science student. However, the final stage in learning requires real patient and equipment for the student to acquire competence with hands-on experience and expertise [40].
In the medical laboratory, the student examines the specimen for disease or cancer; provides information about the patient’s state of health by testing for diseases and assist the medical practitioner with diagnosis, determination of blood levels of drugs for optimal therapy, tests to determine which antibiotics are the most effective against specific bacteria, tissue sections to determine whether malignancy is present. More than 70% of the information a doctor needs to actually treat the patient comes from the laboratory and any discrepancy in sample analysis errors the whole process. It is rewarding to see a patient’s prognosis get better and hence simulation is advocated for because it is seen as the ideal way to prepare students for the clinical environment and as a means of evaluating clinical deficiencies [6].
Understanding that there is a patient at the end of each specimen and that patients’ lives matter, it is important to develop competent and qualified laboratory professionals, hence there is a definite need for an evidence base for the application of innovative simulation-based teaching and learning in medical laboratory science programs in Kenya in order to provide educators with exemplars of simulated laboratory learning, to give weight to their efforts, to change curricula and to identify directions for further research and educational change.
To examine the challenges affecting the application of innovative simulation-based teaching and learning among teaching staff in selected KMTC Campuses offering Medical Laboratory Sciences in Kenya.
The specific objectives were to;
To examine the challenges affecting the application of innovative simulation-based teaching and learning among teaching staff
To appraise the institutions’ ability to apply simulation laboratory sessions for their teaching and learning
To determine the opportunities for innovative Simulation-Based Medical Teaching and learning among teaching staff
To establish the factors that shape a program’s decision to implement simulation-based teaching and learning and what influences its application among teaching staff
What challenges are encountered while implementing innovative simulation-based teaching and learning?
To what extent are simulations defined, constructed, and implemented in the institutions offering medical laboratory science course?
Are there opportunities for those most directly involved in simulated-based learning in MLS?
What factors shape a program’s decision to implement simulations?
Learning to become a Medical Laboratory Scientist is a highly complex endeavour that could not be explained by any one single theory, but various facets of medical learning have been conceptualized by a number of theorists. The predominant theoretical underpinning which informs medical education includes Kolb’s experiential learning model [41], social cognitive model [42], deliberate practice [43], and situated learning [44]. Although Kolb’s model has been criticized as an oversimplification, it has often been applied as a theoretical underpinning of simulation-based teaching and learning and it is the one that was applied in this study.
Kolb’s experiential learning model identifies the main trigger for learning as being a concrete experience where the learner must engage in a transaction with their environment, which the learner may reflect upon and form abstract conceptualization, this leads to critical reflection and active experimentation. Simulation offers a concrete experience that is sensed through scenario-based experiences. These simulation experiences offer structured opportunities for reflection and formulation of abstract conceptualization which can be symbolic and abstracted, leading to extension and active experimentation and rehearsal of the newly formed concepts [45].
The simulated setting allows the concrete experience to occur in a setting that is safe, both from the point of view of patient safety as well as safe from the learning perspective. The teacher’s role is that of a facilitator who guides the learner through both the experience and the reflection to enable connections and abstraction to be made. The power of using plural analogical examples, rather than dependence on single case examples have been highlighted as important in deep learning and transfer to novel situations [46].
Social cognitive theory [42] brings together both behaviourist and cognitivist approaches to understanding learning. The behaviourist approach emphasizes the external behaviour of people and their reactions to situations. It addresses the concept of a stimulus-response relationship where a given stimulus if rewarded will be repeated whereas unrewarded responses will become reduced. In behaviourist theories, no account is taken of internal processes. In the context of simulation, it is feedback from both consequential clinical happenings as well as faculty or peer feedback that serves to offer the ‘reward’ for desirable behaviours. Skills and drills in resuscitation training are typical examples of this approach. The cognitivist approach also emphasizes the interaction of the learner with their environment as they assimilate new experiences into their existing concepts and understanding in order to build or challenge existing knowledge or application of knowledge. Bandura however emphasizes human agency as a core value. He asserts that the power to originate actions is a key feature of personal agency. Personal agency is extended through intentionality and forethought, self-regulation, and self-reflectiveness about one’s capabilities, quality of functioning, and the meaning and purpose of one’s life pursuits. The personal agency operates within a broad network of socio-structural influences. Bandura [42], argues that self-efficacy (the personal agentic belief of the ability to control future actions) is an essential element in learning. The application of Bandura’s principles in simulation is most often described with reference to self-efficacy: rehearsing a skill or complex procedure or behaviour should both enhance self-efficacy and provide a trigger for reflection.
Deliberate practice is a term introduced by Ericsson, et al. [47] where they identified the development of psychomotor skills in experts in terms of hours of deliberate practice, as a means of explaining variation in individual performances. The theory describes stages of development of skills competence from novice towards mastery and finally to autonomy. Deliberate practice is the intense and focused repetitive performance of an intended cognitive or psychomotor skill in a focused domain, coupled with rigorous skills assessment that provides learners with specific, informative feedback resulting in increasingly better skills performance, in a controlled setting. Although this initial work was carried out in relation to speed typists and musicians the concepts have been applied in the context of medical education and simulation [43].
Much of the literature suggesting the advantages of simulation focuses on the opportunity that simulation offers for repetition and practice. In one reported study [48] medical students who engaged in deliberate practice using simulation acquired improved skills in cardiac auscultation when compared with a comparison group.
Situated learning [44] is one of several theories where participation in a group, in a socio-cultural setting is key to learning. It is a theory that enables understanding of the apprenticeship model of learning, where a whole community contributes to the development of the apprentice, rather than a single expert. The learning which occurs is through collaboration, social interaction, and connectivity with the practice community. This theory suggests that when a new learner enters the community of practice they do so at the periphery. Lave & Wegner [44] called this legitimate peripheral participation. The novice observes, performs less vital tasks, and gradually, with increasing skill and experience moves towards the centre of the community of practice as they learn the knowledge, values, and discourse of the whole group which include experts, peers, and more advanced apprentices. Participation in discourse (or talk) within the community is vital to learning. Situated learning theory encompasses cognitive apprenticeship theory and informal learning theories. It is also closely related to the experiential learning model as it includes learning by doing and participating in the shared experience of the community.
Constructivism Learning Theory: This theory was founded by Jean Piaget in 1976. The theory advances the significance of involving learning in active participation with the aim of constructing knowledge for individual learners. The students are assumed to utilize background knowledge and concept that normally aid them during the acquisition of new information. Dewey, Kolb, and Montessori’s learning theories provide the platform for the use of the constructivist learning theory comprising a myriad of concepts such as active learning, discovery, and knowledge building. Of essence is that all the concepts provide or rather enlighten the students to more flexibility within a given blueprint or system [49].
Constructivism stipulates that the role of the teacher is that of a facilitator tasked with the role of motivating students to discover new tenets and facets of knowledge by themselves. Through such a development, the students are well placed to construct their own knowledge through self-conceptualization. This can be enhanced through the facilitator who instills curiosity and debate among learners, putting into mind their autonomy. Curiosity can be developed by teachers through adding raw and challenging data, new resources and materials in order for students to critically analyze [50].
The constructivist view to learning in the classroom is fashioned in Bruner [51], and Dewey [52] developmental theories. Piaget’s works that gave birth to cognitive construction postulates that, a person’s reaction to experiences is likely to lead or fail to lead to learning. On his part, Vygotsky’s social constructivism stipulates that factors such as language, communication, and social interactions among peers, family, and teachers are significant in the construction of meaning from experiences. According to Vygotsky, meaning is co-constructed and not just constructed [53].
The theory that informs and justifies this study is Experiential Learning. The distinguishing feature of experiential learning based on the work of Steffes [41] is that the experiences of a learner occupy the central place in their teaching and learning [54] and that is exactly what happens during the training of a medical laboratory science learner. Experiential learning shares epistemological tenets with andragogy (the art and science of helping adults learn) but emphasizes engagement and active participation for effective learning. Fanning and Gaba [55], have described this theory as ‘learning by doing, thinking about, and assimilation of lessons learned in everyday behaviours. The experiential learning process is cyclical and encompasses four interrelated aspects [41].
Kolb [56] conceptualized that such learning is a process whereby knowledge is continuously acquired, tested, analysed and reflected upon during and after an event, and so can represent a holistic learning process [54]. This concept of reflection and analysis is the cornerstone of simulation-based education as an experiential learning context. A learner in an inter-professional simulation (a medical laboratory science student) can participate in such an immersive scenario and learn through critical thinking and adaptation rather than strictly content delivery as is often the case in a classroom setting [55,57].
Experiential learning asserts that, adults learn in ways not possible from instruction or information delivery alone, and necessitates interaction between the learner and the environment, moving between ‘opposing modes of reflection and action, feeling and thinking’ [58]. SBME provides an experiential learning context as experiences, either real or simulated, are catalysts for experiential learning [59], and experience is the foundation of, and the stimulus for adult learning. People learn through interactions with people and the environment and hence simulation expands on the traditional classroom and student simulation-laboratory experiences. This includes professions outside of the laboratory with which MLS students interact. MLS programs utilize experiential learning in the student laboratory with case-based specimen analysis; however, it is time to break out of the silo and teach students how to work with inter-professional teams prior to entering the professional healthcare setting.
An additional experiential educational or learning model which fits with SBME and aims to enhance learners’ expertise or mastery is provided by Dreyfus and Dreyfus [60] through their novice to expert. Adult skills acquisition is based on learning skills, rather than a profession. Their argument is that ‘skill in its minimal form is produced by following abstract formal rules, but that only experience with concrete cases can account for higher levels of performance’.
Dreyfus [61] refined the model by Dreyfus and Dreyfus [60] whose five phases were: novice, competent, proficient, expert and master to novice, advanced beginner, competence, proficiency, and expertise. The model was constructed around the four mental functions of component, perspective, decision, and commitment and how these varied at each level of the model.
As learners develop or mature these mental functions, they increase their level of expertise along the five-stage continuum. Individuals progress through the five stages of expertise by drawing on their experiences of solving problems in context in order to reach higher levels of expertise using combinations of the four mental functions. Context and experience in the training of MLS students are fundamental components of the Five-Stage Model of adult skills acquisition.
In the earlier stages, the lecturer reduces complex problems into small pieces which can be solved without knowledge of the entire situation, and in the later stages see learners associating the facts and rules more with context that can be relied upon for future application, and so begin to use analytical processes and rely on past experiences, including drawing on emotional reactions, to decide which elements of the situation are important [61].
At the final stage of expertise an individual, not only sees what needs to be done, but also envisages the solution without having to go through an analytical process to arrive at the solution. At this level the individual is totally immersed in understanding the situation, making decisions on how to proceed, and in the outcome of the situation. The application of Dreyfus and Dreyfus [60] novice to expert model to the educational/experiential aims of SBME can be clearly seen, as this setting provides an experiential medical context for expertise development where the use of mental functions is promoted as the complexity of medical scenarios is enhanced and the level of responsibilities increase.
This model has been applied by several authors [62,63] and now the researcher, who examined the learning of skills and competency development in broader areas of medical education and more so Simulation-Based Teaching and Learning in MLS.
In conclusion, Kolb’s experiential learning model identifies the main trigger for learning as being a concrete experience where the learner must engage in a transaction with their simulation-based, the learner may reflect upon and form abstract conceptualization, which leads to critical reflection and active experimentation. Experience in this context can have the dual meaning as subjective and personal, as well as objective and environmental, these two forms of experience ‘interpenetrate and interact in very complex ways’ [64]. Simulation offers just such a concrete experience which is sensed through scenario-based experiences and most simulation experiences offer structured opportunities for reflection and formulation of abstract conceptualization which can be symbolic, abstracted and lead to extension and active experimentation. The power of using plural analogical examples, rather than dependence on single case examples has been highlighted as important in deep learning and transfer to novel situations [46].
In this model (Figure 1), the goal of medical education is to produce MLS graduates with the necessary knowledge, clinical skills and professional attributes to be successful healthcare professionals. To a certain extent, a medical laboratory scientist level of competence reflects the educational institution they attended and the medical education they received. Therefore, it is vital to appraise the educational environment in which medical lab students learn, including the institutional culture, curriculum, staff competence level and learning climate. Meaningful learning correlates positively with students’ perceptions of their educational environment, as this can influence how, why and what students learn [66].
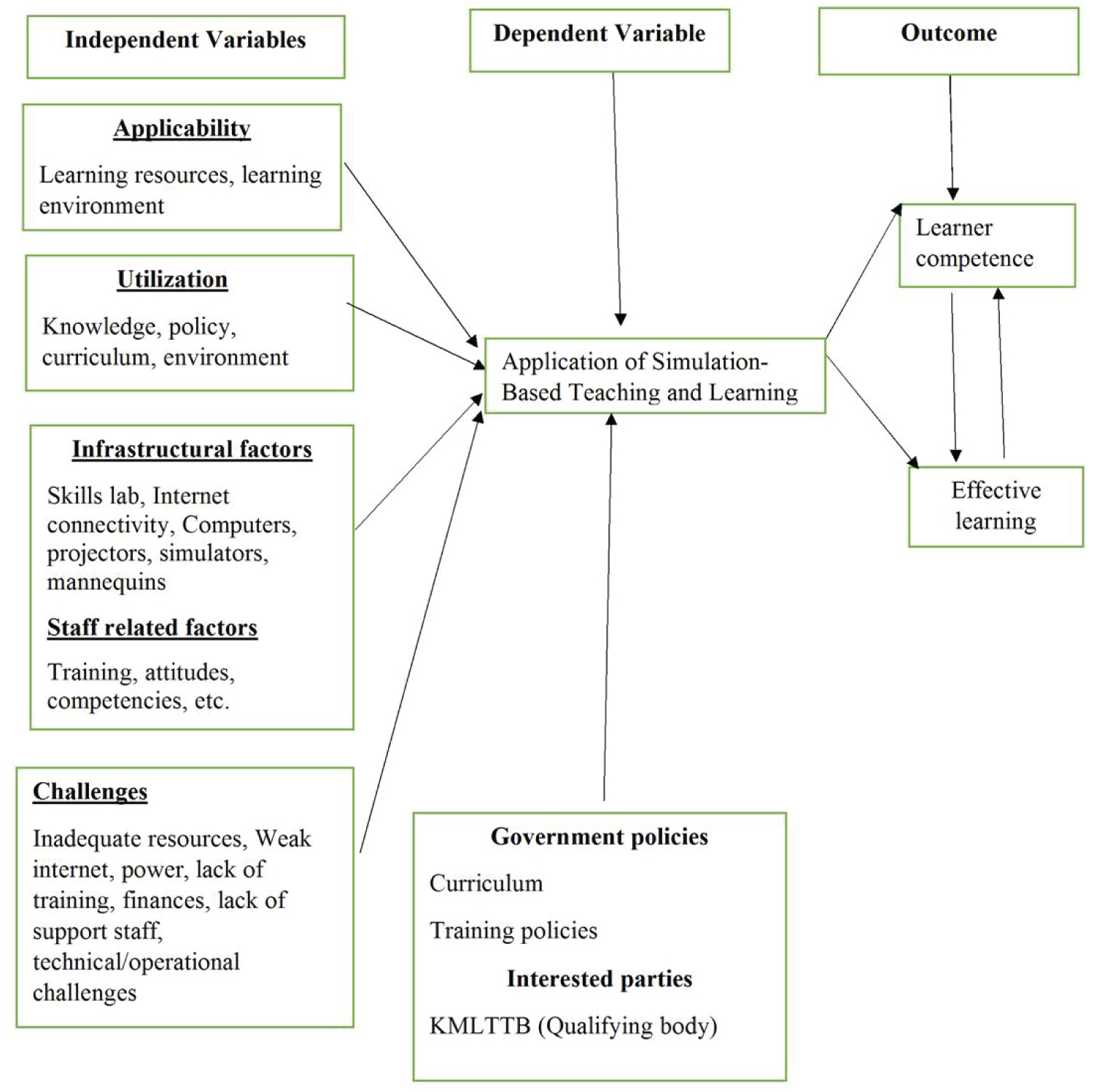 Figure 1: Conceptual framework.
Figure 1: Conceptual framework.
Intervening variables [65].
View Figure 1
The study used mixed-methods cross-sectional research design. This design was best suited for the study since it used information obtained as at particular time. The design was considered appropriate in achieving the study objectives. This study was conducted at the Kenya Medical Training Campuses, offering medical laboratory science program. These campuses are distributed in 12 counties of Kenya. KMTC has more than 74 constituent colleges of the expansive institution offering 50 courses.
The target population comprised of lecturers teaching in the Department of Medical Laboratory Sciences in the various campuses and the principals in these campuses. The researcher chooses campuses offering medical laboratory sciences because of being a professional in the same. Census method was used. The total population was 58 staff. These were 47 lecturers and 11 principals.
The researcher used data collection assistants. The assistants had a minimum of a KCSE certificate. The research assistants underwent three day training on how to identify the respondents, how to approach them, courtesy when engaging the respondents, communication and how to administer the questionnaires. The research assistants administered the first twenty questionnaires with the researcher so as to ensure professional administration of the questionnaires. The research assistants directly delivered the questionnaires to the respondents at the said campuses. The respondents were informed verbally and in writing about the study. Those who consented to fill the questionnaire were provided with questionnaire to fill, and on completing the questionnaire they collected and sealed in an envelope. The questionnaires were collected upon completion daily by the research assistants at designated areas for analysis. Daily review of the questionnaires filed and collected was done by the researcher. Raw data entries were reviewed for data entry errors and corrected prior to analysing data to ensure accuracy and consistency. Data was all coded and entered into a database and quantitative data. Interviews were conducted by the researcher while the checklist was filled by the laboratory in-charges.
Data analysis was conducted using the Statistical Package for Social Science (SPSS) software version 22 for windows. Both descriptive and inferential statistics were used in data analysis. Whereas descriptive statistics included frequencies, percentages, means, and standard deviations, inferential statistics included the chi-test. Quantitative data were presented in tables, graphs, and charts. Responses to qualitative data were thematically analysed.
The study sought at appraising the institutions’ ability to implement and conduct simulation laboratory sessions for their teaching and learning. To achieve this objective, the respondents were first asked how well they understood and defined simulated medical laboratory experiences both actual and anticipated and why they thought so. The scores from their responses were as indicated.
As shown, the respondents 39 (83.0%) of the lecturers indicated that they very well understand and define simulated medical laboratory experiences both actual and anticipated while 8 (17.0%) of the lecturers indicated they somehow understand and define simulated medical laboratory experiences both actual and anticipated. The respondents said they thought so because simulation was well outlined in the teaching curriculum and in all their course outlines. Others reported that they thought so because simulation-based teaching and learning was an important requirement for all Medical Laboratory students before they go to the clinical site and handle the actual patients, while others indicated that simulation-based teaching and learning was a teaching strategy that they used after they had done the theory so that they can reinforce student understanding (Table 1).
Table 1: How well do you understand and define simulated medical laboratory experiences both actual and anticipated. View Table 1
To achieve this objective, the respondents were given the example of challenges suggested to influence simulation-based teaching and learning.
From the results obtained, the respondents agreed that all the challenges suggested also applied in their institutions as far as simulation-based teaching and learning is concerned. Their responses were as follows: issues of professionalism and certain skills 43 (91.5%), simulations are demanding for instructional staff 46 (97.9%), simulations are resource-intensive (funding, equipment, specimens, space and scheduling and administrative support 46 (97.9%), some aspects of laboratory work are difficult or impossible to simulate 44 (93.6%) and the quality of the learning experience may be uneven 43 (91.5%) (Table 2). The respondents were also requested to list any other challenge that they encountered in their institution. Some of the challenges cited were: - “untrained staff on simulation-based teaching in MLS, lack of adequate infrastructure, poor internet strength, lack of enough models for simulation, lack of standard specimens due to complex specimen collection procedures for some specimens as well as instability of analytes when specimens are stored for long and Instability of power (electricity)”.
Table 2: Challenges affecting the application of simulation-based teaching and learning. View Table 2
The respondents were first asked to tick in the relevant box, the perspectives and opportunities brought about by innovative simulation-based medical teaching and learning among teaching staff in medical laboratory sciences.
Almost all the respondents agreed that the suggested opportunities above have been brought about by innovative simulation-based learning. Only very few disagreed on a few of some opportunities as seen from the Table 3. The opportunity for assessment is seen as one of the major advantages for medical simulation. It is also noted in particular that simulation-based learning has the potential for capturing behaviours in contexts similar to actual practice. Other distinct opportunities is in the fact that the setting is reproducible and that simulation allows measurement of skills such as communication and professionalism, which are otherwise difficult to evaluate. Other positive features for simulation-based learning in medical laboratory sciences as reported by the respondents are the fact that it enables them to earn Continuous Professional Development (CPD) points as well as enabling them to use case scenarios in their facilitation.
Table 3: Perspectives and learning opportunities for innovative simulation-based teaching and learning among teaching staff. View Table 3
The narrative on what some respondents said include:
“Provision of an opportunity to practice rare practices like animal dissection, inoculations, a culturing method for viruses”, “preservation of parasites such as trypanosomes”, “use clinical scenarios”, “opportunity for making teaching and learning easier and more efficient”.
Some respondent said that simulation-based learning helps in facilitating ongoing integration of theory and practice, creating opportunities for learning professional language and participating in Inter-professional and teamwork-based activities as well as provision of feedback as alluded by a respondent who said that who mentioned that; “simulation-based teaching and learning makes the whole process of teaching skills and attitude easier”.
From the results obtained, most respondents agreed that the listed factors really shape and influence program’s decision to implement and apply simulation-based teaching and learning indicating that they were part of the considerations they put in place when they thought of implementing simulations in their various institutions with a few having different opinion as seen from the Table 4. Educational validity seems to have been an afterthought in the adoption of simulation-based learning, because 100% of the respondent agreed to it with 37 out of 47 respondents strongly agreeing. The respondents also reported that simulation-based learning effectively helps students learn skills they can apply on real patients or real-life situations, helps increase self-confidence on the students and lecturers as well as making teaching and learning easy.
Table 4: Factors that shape a program’s decision to implement simulation-based teaching and learning. View Table 4
The respondents were also asked about the simulated activities that are directly applicable to MLS and particularly in their institution, the following was a list of simulated activities they voiced out:- “sample collection, analysis of specimen, drug sensitivity testing and culture, media preparation, teaching on internal organs especially anatomy and physiology, dissection, cancer cell and their staging, tissue processing, during practical examination, patient’s response during sample collection, dispatch of results, hands-on practice on any theory given, and simulation of vectors and parasites pathogenic to humans”.
One respondent said “the simulated activities directly applicable in my institution include: - formal ether concentrate method to the slides, getting mosquitoes and demonstrating its parts for the purposes of identification”.
The respondents also reported on the increased use of simulation in MLS education and they alluded that their use was mostly driven by “accreditation of educational programs and standardization of graduate competence” . Other reasons they highlighted included “changes in the medical field, national portability of credentials and economic concerns” .
The study found that there were challenges affecting the application of innovative simulation-based teaching and learning among teaching staff. The study thus concludes that addressing the challenges of simulation in these campuses through training instructional staff and equipping the simulation laboratories will result in its application being improved significantly. The simulations were defined, constructed, and implemented to a greater extent. The study thus concludes that medical laboratory departments have offered some degree of simulations in their programs since they were first brought into the college-based didactic environment from their hospital origins. Further, it was found that simulations are used during their teaching and that it was well incorporated into their teaching curriculum. This is attributed to the fact that it makes learning and teaching both easier and simpler. The study also found out that, there are so many learning opportunities brought about by innovative simulation-based medical teaching and learning among teaching staff. The study, therefore, concludes that innovative simulation-based teaching and learning are key in the training of medical laboratory science students because of these distinct learning opportunities. This could be the reason why there are success stories of the effectiveness of the strategy. The study also found that there were factors considered to influence and shape a program’s decision to implement and apply simulation-based teaching and learning in the department of medical laboratory sciences. Most respondents agreed that the listed factors really shaped and influenced their decision to implement and apply simulation-based teaching and learning indicating that they were part of the considerations they put in place when they thought of implementing simulations. The study concludes that the campuses offering medical laboratory science programs should address the different opinions of the staff concerning the same to ensure uniformity.
Based on the study’s findings, the study makes several recommendations. The management to employ more medical laboratory technologists, and instructors as well as laboratory assistants in order to prevent workload overload and ensure the construction of fully equipped simulation laboratories in the training institutions offering medical laboratory science program. This should be highly prioritized during strategy formulations and budgetary allocation. The study established that KMTCs offering medical laboratory science program were not uniform in the implementation of simulations as a teaching and learning tool. The study therefore recommends that the management to ensure there is standardization and harmonization of training of Medical Laboratory Science program across all KMTCs offering the program in Kenya. The management should also create more opportunities for staff and more infrastructural support to promote implementation and sustainability. Also, The Head of Department, Nairobi campus to prepare schedule for updates especially continuous professional development programs for medical laboratory staff on simulation-based teaching and learning.