Background: Long COVID has recently been recognized by the World Health Organization as a syndrome occurring two months after infection with Covid-19 with various physical, neurocognitive, and psychiatric symptoms that cannot be explained by another diagnosis. It is estimated that between six and twenty million patients in the United States alone are affected by this condition.
Unfortunately, despite its prevalence, there is no established treatment regimen. The most widely prescribed therapies include respiratory care and physical therapy, cognitive therapy, and emotional support. Previous reports from the U.K. and Israel showed improvement in fatigue and brain fog following a regimen of Hyperbaric Oxygen Therapy (HBOT). The aim of this pilot study is to attempt to replicate the reported symptomatic improvement in long COVID patients with a short course of HBOT.
Methods: Twelve patients were recruited via social media outlet to participate in a study investigating long COVID at a private outpatient hyperbaric facility. All patients had documented PCR COVID infection, had been diagnosed with long COVID by their primary care medical doctors and screened for contraindications to HBOT. Patients underwent ten 80-minute sessions of hyperbaric oxygen delivered via facemask at 100% oxygen at 2.0 ATM in a monoplace hyperbaric chamber. Patients were required to complete the 11-point Chalder Fatigue Scale as well as the Post Covid Functional Scale at baseline, five-session mark, and ten-session mark. The ten sessions had to be completed over a 2-week period.
Results: Patients showed statistically significant improvement in both the Chalder Fatigue Scale as well as the Post Covid Functional Scale at the five and ten session marks post-treatment. There were no complications from treatment and all patients reported improvements in energy as well as cognition.
Conclusions: This study confirms previous reports of the efficacy of HBOT as a treatment modality for patients suffering from long COVID. With estimates of 15% of all previously infected adults in the US having long COVID symptoms, this report emphasizes the efficacy of HBOT as a first line therapy for long COVID as well as highlights the need for large scale studies utilizing this modality.
COVID-19, HBOT, Long COVID, Hyperbaric oxygen and SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has resulted in more than 679 million cases of COVID-19 with 679,021,063 deaths as of February 2023 (CDC). While most of those infected recover, a significant number of patients maintain a range of persistent symptoms that can have devastating effects on their quality of life. This has been commonly termed "long COVID" [1]. The World Health Organization has defined the presence of various symptoms, even weeks or months after acquiring SARS-CoV-2 infection irrespective of the viral status as "long COVID". This condition is confirmed three months from the onset of infection with having physical, neurocognitive and psychiatric symptoms that persist for more than two months and cannot be explained by an alternative diagnosis. The most common physical symptoms include fatigue, dyspnea, ageusia, anosmia, insomnia, headaches and systemic widespread pain [2]. "Long COVID," also known as post-COVID, was formally recognized as a condition that could result in a long term disability under the Americans with Disabilities Act (ADA). Post SARS-CoV-2 infection is a recognized as a public health emergency with multiple clinical challenges in terms of establishing a diagnosis and best treatment [2-4].
Despite recognition from WHO and CDC, this condition remains the pandemics least understood clinical syndrome as there exists no blood test or biochemical marker to confirm the diagnosis. Researchers still cannot even completely agree on its prevalence or the features that define it. What is clear is that we now have a new chronic illness that could potentially affect millions of people and prevent their ability to work or participate in normal daily activities. Fatigue is one of the most commonly reported symptoms with estimates of up to 65% of patients which is often accompanied by cognitive and affective deficits [5-8]. The fatigue experienced can be particularly severe often preventing patients from performing their usual work and activities and this is particularly troublesome as the age group most affected tends to be economically active adults [9]. The patho-physiology of post-COVID-19 condition is not yet been clearly elucidated and possible etiologies include direct brain invasion of the viral particles, dysregulated immune response, thrombotic disease, mitochondrial dysfunction and vascular compromise with secondary tissue hypoxia [9].
The most commonly reported treatment options include physical and occupational therapy, anti-inflammatory molecules targeted toward the virus, dietary regimens, and psychological therapy but none have emerged as the clear best option [5,7,10]. Both Paxlovid and metformin were studied as a treatment for acute COVID and both showed some evidence in reduction of the incidence in the development post COVID symptoms but have not been studied as a treatment for long COVID [11,12].
Because of the severe lung involvement in acute SARS-CoV-2, hyperbaric oxygen was studied for patients in severe respiratory distress from acute, severe infection. A systematic review was performed by Oliaei who reviewed eight studies worldwide and concluded that, HBOT allowed most patients to recover after treatment with blood oxygen saturation increased after several sessions of HBOT [13]. Overall, HBOT seems to be a safe and effective method to improve oxygenation with COVID-19 but none of the studies were well controlled.
A recent case series of ten post-COVID-19 condition patients undergoing ten HBOT treatment sessions in a large multiple chamber at 2.4ATM in the U.K showed improvement in fatigue and global cognition [6]. More recently, Zilberman-Itskovitch, et al. in Israel provided strong evidence in a double blinded study that hyperbaric oxygen improves neurocognition symptoms in a large, randomized, clinical trial with patients undergoing 40 daily sessions at 2.0 ATM over a two month period and showed significant improvements in global cognition and energy domain [14].
This study was designed to evaluate the short-term effects of HBOT on patients suffering from post SARS Covid-19 t infection in a small pilot trial in New York City, the epicenter of the pandemic in the USA. Our goal was to attempt to replicate the results of Robbins, et al. and determine whether a protocol of 10 sessions at 2.0 ATM in would provide clinical benefit for patients suffering from sequelae of SARS COVID-19 infection. We chose the validated 11point Chalder fatigue scale as well as the Post Covid Functional Scale our outcome measurements to capture both the fatigue and neurocognition components [15,16].
We recruited 15 patients from social media websites who were suffering from long COVID symptoms a to participate in a free trial of ten sessions of hyperbaric oxygen over a two-week period (weekend off). The following inclusion were utilized: above 18 years of age, confirmed PCR positive diagnosis of COVID-19 illness at least three months prior to treatment, being willing and able to participate in hyperbaric oxygen treatment, complete the outcome scores during the treatment period, and finally suffering from symptoms of long COVID as confirmed by their medical doctor. Exclusion criteria were a history of any non-COVID brain pathology, active malignancy, substance use at baseline, any significant physical disorders or major cognitive deficits, chest pathology incompatible with pressure changes, history of chronic fatigue syndrome, epilepsy, ear, sinus pathology, and claustrophobia. All patients signed an informed consent prior to the initiation of treatment.
Of the 15 enrolled patients, three patients dropped out of the study for two for inability to complete the ten sessions within the two-week period and one developed an unrelated illness. The study group thus consisted of seven male and five female subjects with an average age of 49 (range 27-73). Demographic data on patients is presented in Table 1 below.
Table 1: Demographics of COVID patients undergoing hyperbaric oxygen treatment. View Table 1
Hyperbaric oxygen was delivered utilizing the Forteus 420 hyperbaric chamber (Oxyhealth, Sante Fe, New Mexico) with 100% oxygen delivered via face mask. The chamber can be pressurized up to 2.2 ATM but for the study we pressurized the chamber to 2.0 ATM for the treatment which lasted 80 minutes (10 minutes to get to 2.0 ATM, 60-minute session, 10 minutes depressurize) All patients received 10 HBOT sessions (with a 2-day break in the middle for the weekend) and all subjects completed the treatment.
Patients completed the Chalder fatigue scale and Post Covid Functional Scale pre-treatment, after five sessions, and after ten sessions. Chalder, et al. developed a brief self-rated 14-item for chronic fatigue but the modified 11pt scale has been validated for the general population [15]. The fatigue scale is self-administered and attempts to measure the extent and severity of fatigue both within the clinical and non-clinical, epidemiological populations. It is a relatively short questionnaire in simple English with a straightforward answering system and provides a brief tool to measure both physical and psychological tiredness (Figure 1).
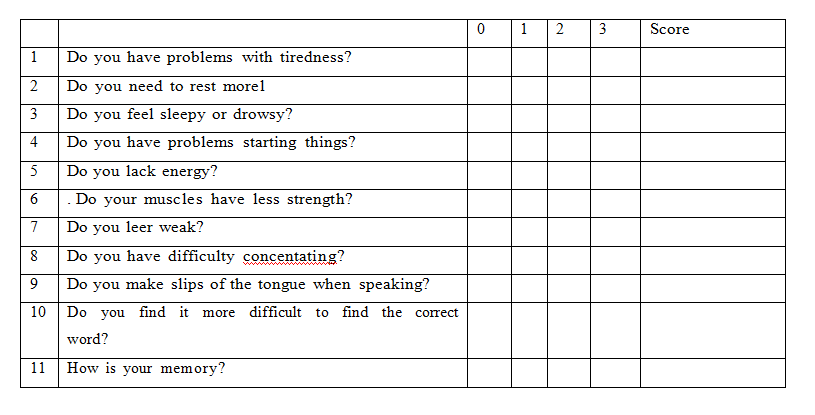 Figure 1: Chalder Fatigue Scale.
View Figure 1
Figure 1: Chalder Fatigue Scale.
View Figure 1
The Post Covid Functional Scale (PCFS) measures patients functional status post COVID over time [15]. The scale is a self-reported functional scale which attempts to cover the an entire range of functional limitations, including changes in lifestyle, sports and social activities (Figure 2).
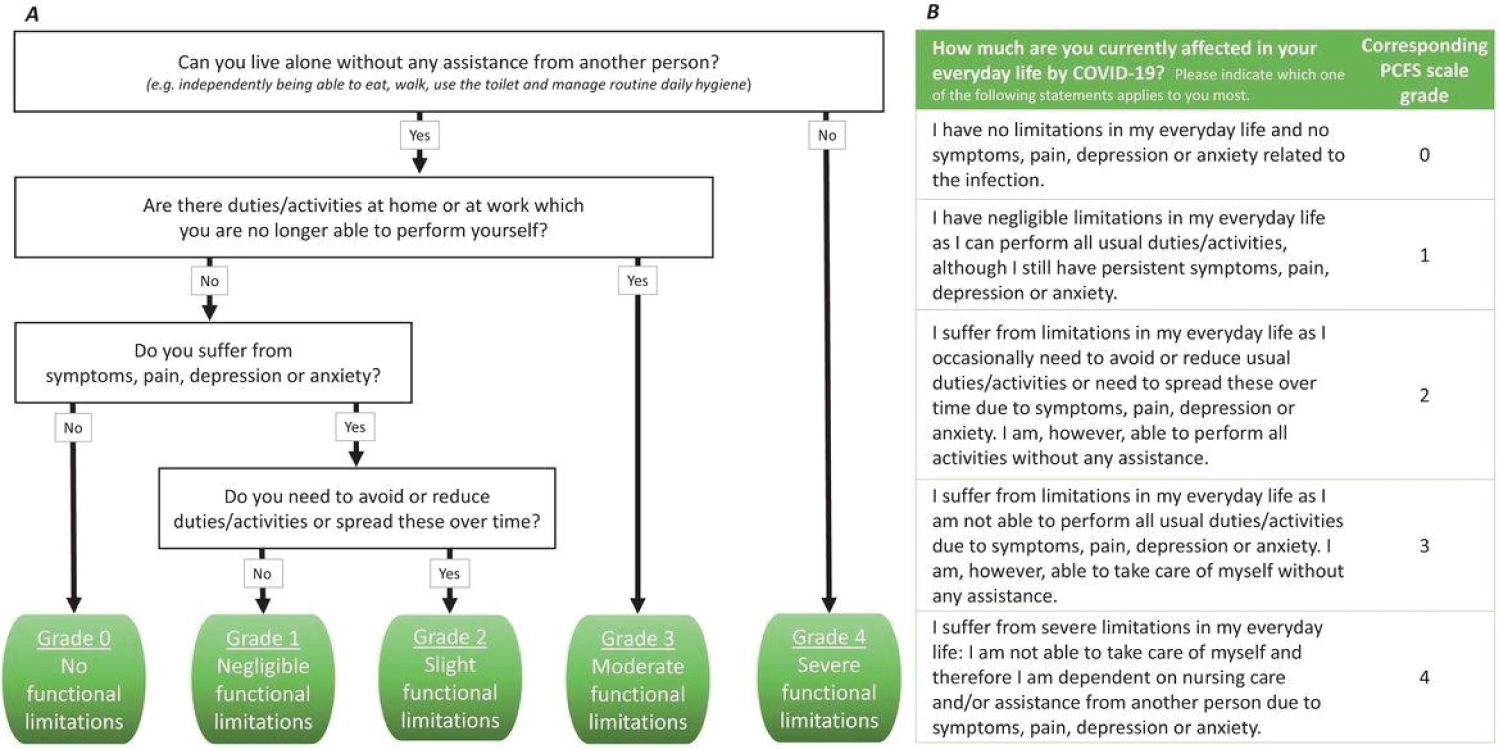 Figure 2: The Post Covid Functional Scale (PCFS).
View Figure 2
Figure 2: The Post Covid Functional Scale (PCFS).
View Figure 2
The results were analyzed using a paired t-test. For descriptive statistics continuous variables are presented as a mean and standard deviation or 95 percent confidence interval while categorical variables are presented as frequency and percentage. To determine significant changes pre and post treatment with Chalder and PCFS scores, paired t-tests were utilized with an alpha of 0.05. Analysis was performed on R: A Language and Environment for Statistical Computing (R Core Team 2022, Vienna Austria).
All patients showed significant impairment on both the Chalder fatigue scale [15] as well as the Post Covid Functional scale [16] at the initiation of the treatment. The mean Chalder fatigue scale showed significant improvement both at the five-day mark (p = 0.002) as well as the ten-day mark (p < 0.001) Prior to the initiation of treatment, patients showed significant impairments with a mean Chalder score of 22.5 and a mean PCFS of 2.3. After completing 5 treatments, all patients experienced significant improvement in the Chalder score (22.5 to 14.3, p = 0.002) but not significant improvement in the PCFS score (p = 0.8). At the completion of 10 treatments relative to the baseline timepoint, all patients had significant improvement in both Chalder score (22.5 to 11.4, p < 0.001) as well as the PCFS (2.3 to 1.5, p = 0.005). The mean Chalder scores as well as the improvement are displayed in Table 2 and Table 3 while the mean PCFS and improvements are shown in Table 4 and Table 5.
Table 2: Mean Chalder scores of Covid patients undergoing hyperbaric oxygen treatment. View Table 2
Table 3: Mean improvement in Chalder scores of COVID patients undergoing hyperbaric oxygen treatment. View Table 3
Table 4: Mean PCFS of COVID patients undergoing hyperbaric oxygen treatment. View Table 4
Table 5: Mean improvement in PCFS of COVID patients undergoing hyperbaric oxygen treatment. View Table 5
No adverse events were reported in any of these patients receiving HBOT during this treatment or in the immediate post-treatment period.
The results our pilot study confirms Robbins study in that a short course of hyperbaric oxygen (10 sessions) can have a significant effect on patients suffering from long COVID. We demonstrated statically significant improvement in both fatigue (Chalder scale) [15] and neurocognitive functions (Post Covid Functional Scale) [16] and this reaffirms the use of hyperbaric oxygen as an effective treatment for those patients suffering lingering symptoms due to remote SARS-CoV-2. The improvement in fatigue was more immediate at the 5 day mark while the improvement in PCFS was only significant at the 10 day mark which we believe is due to the neuroplasticity effects of hyperbaric oxygen which may take longer for patients have a clinical effect. Many researchers believe post Covid fatigue has clinical overlaps with chronic fatigue syndrome (CFS) and previous studies have demonstrated that HBOT can be beneficial in reducing symptom severity and increasing quality of life in this group of patients [17,18]. Our patients were suffering significant symptoms of fatigue pretreatment with an average Chalder score of 22.5/33 indicating significant lack of energy. A drop to 14.3 after just five sessions and then to 11.4 showed the profound effect of breathing 100% oxygen at high pressure has on the fatigue symptoms. Zilberman-Itskovich in their randomized, double blinded study of 40 sessions with brain PET scans showed that HBOT induced changes in the frontal lobe and this area has been implicated with fatigue in COVID-19 patients [14]. Many clinical studies have also shown that HBOT can improve pain and quality of life of fibromyalgia patients and these patient group has very similar symptoms to long COVID [8,9,19-22]. Previous studies have shown that fibromyalgia is associated with decreased brain perfusion in the insula, hippocampus, putamen, prefrontal and cingulate cortex [23-25]. Zilberman-Itskovich's study showed increased perfusion in these regions after HBOT and possibly this increased brain perfusion is responsible for the patients improvement in energy and neurocognition [14].
Dysregulation of the immune-brain axis, the coagulation process, and auto- inflammation have all been postulated to cause severe fatigue in Covid patients [26]. While it has not been proven what is the exact pathogen for post infection symptoms, hyperbaric oxygen has been shown to have strong appositive effect on the all of those areas of dysregulation. Many clinical studies have demonstrated several neuroplasticity effects such as anti-inflammatory, mitochondrial function restoration, angiogenesis and induction of proliferation and migration of stem cells all which are potentially beneficial [8,9,27-29].
Our results also showed significant improvement in patients Post Covid Functional Scale with an improvement from with improvement from 2.3 to 1.2. The PCFS is a simple tool to monitor symptoms and the impact of symptoms on patients functional status, i.e. a scale that can measure the consequence of the disease beyond outcomes such as mortality. Becker, et al. show that the main neurocognitive impairment in post-COVID-19 condition is dysexecutive, or brain fog, which has significant implications for occupational, psychological, and functional outcomes [30]. While the magnitude and immediacy of the improvement in the PCFS was not as great as the Chalder fatigue scale we believe it takes longer for the neuroplasticy effects of hyperbaric to become evident as well as the patients pre -treatment PCFS were not severe. For the patients to participate in this outpatient treatment protocol they had to be functional enough to be able to attend ten 80 minute sessions in 2 weeks at a remote site and fill out the corresponding outcome data. Patients with severe score on the PCFS (3 or above) were unable to perform all their activities of life and thus would have been too disabled to participate in this study.
We felt that measuring both outcome measurements would give us the best tool to determine the effects of this short course of hyperbaric oxygen treatment. These protocols utilize the so called "hyperoxic-hypoxic paradox", by which alternating fluctuation in both pressure and oxygen saturation may induce gene expression and metabolic pathways that are essential for regeneration without the hazards of prolonged hypoxia. Many of pathways can modulate can promote angiogenesis and restore mitochondrial function and induce neurogenesis in injured brain tissue [8,9,19,27,31-34].
Our patients clearly improved after ten sessions, and this is important information for patients as a 40-session hyperbaric program is very difficult to accomplish for patients because this treatment is considered off label in the United States and is not covered by government or commercial health insurance. We are cognizant of the limitations of this pilot study but feels it provides useful confirmatory data for those patients seeking treatment because as of this writing there is no accepted treatment protocols. There are currently limited treatment options for post SARS-CoV-2 infection, with even fewer treatment options available for those suffering from fatigue and thus this study reaffirms the need to study hyperbaric on a larger scale. Both Paxlovid and Metformin when given for acute infection showed a reduction in the development of post COVID symptoms and certainly prevention of disease is a desired outcome however neither have been studied for those who already developed long COVID [11,12].
There are some clear limitations of this pilot study. First, there was no control group and the placebo effect of ten hours of treatment for subjective symptoms cannot minimized. Second, the follow up was only two weeks and thus we have no data on any permanent improvement in symptomatology. We originally planned follow patients at six months but unfortunately at the six month five of the 12 were re-infected with Covid-19 (Omicron) making any data on the remaining seven patients problematic. However, all 12 patients felt the hyperbaric treatment helped their symptoms and would like to continue with this treatment.
Long COVID is now firmly established as a diagnosis that can cause significant long term disability and its management is challenging for the both the patient and health care provider. Successful treatment options are limited and we believe this additional report on the efficacy of short-term hyperbaric oxygen is an important contribution to raise the awareness of HBOT as an effective treatment modality.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None.
This manuscript has not been presented at any academic conference or meeting.