Background: The COVID-19 pandemic saw government-imposed health mandates that contributed to profound work, exercise, and lifestyle changes. There was an observed increase in weight gain and sedentary behavior during the pandemic in United States, as well as increased outdoor exercise and running in the United States. While road race times have consistently slowed over the last few decades, it is unknown how running performance changed during the pandemic.
Methods: This was a retrospective analysis of finishers of the world's largest 10 km road race in 2019 (pre-pandemic) and 2021 (pandemic). Times were gathered using implicit JavaScript Object Notation API and novel web-scraping and post-processing. Participants' resident state and pace were correlated with open sourced publicly available durations of shelter-in-place, mask mandates, and gym closures in addition to COVID-19 hospitalization incidence and per capita mortality from March 2020 through March 2021. Runners' pace and participation differences were correlated with per state mitigation stipulations and per-capita COVID-19 hospitalizations and mortality from March 2020 to March 2021, controlling for age and sex. All data was open access.
Results: There were 60,525 pre-pandemic and 24,265 pandemic runners. The pace average was 1.4 min / mile faster (95% confidence interval [C] 1.34 to 1.45, p < 0.001) during the pandemic (12 versus 13.4 min / mile). Finishing times decreased during the pandemic in both women (12.9 vs. 14.3 min / mile, 95% CI 1.31 to 1.47, p < 0.001) and men (11.3 vs. 12.5 min / mile, 95% CI 1.2 to 1.3, p < 0.001). These performance trends were consistent in the 10,475 repeat runners (p < 0.001). These performance trends were consistent in the 10,475 repeat runners (p < 0.001) in both women (-0.4 min / mile, 95% CI -0.4 to -0.3, p < 0.01) and men (-0.3 min / mile, 95% CI -0.4 to -0.3, p < 0.01), with greatest improvement in those younger than 20 years old (-1 min / mile, 95% CI -1.2 to -0.7, p < 0.01). Mitigation had negligible impact on performance when weighted by resident state and duration of mask mandates (r = 0.17, 95% CI -0.1 to 0.5), shelter-in-place (r = 0.24, 95% CI -0.1 to 0.5), and gym closures (r = 0.14, 95% CI -0.2 to 0.4). There was no correlation between performance and COVID-19 hospitalization incidence (r = < 0.01, 95% CI -0.4 to 0.4) or per capita mortality (r < 0.01, 95% CI -0.3 to 0.3).
Conclusion: Pandemic-era 10 km runners saw improved performance over pre-pandemic times, consistent across age groups and sex, with the biggest benefit in the youngest people. COVID-19 mitigation restrictions and disease severity did not affect performance, suggesting unmeasured lifestyle changes may have contributed to improved fitness.
Running, Performance, COVID-19, Lifestyle, Infectivity, Mitigation
COVID-19: Coronavirus disease 2019; United States: U.S.; District of Columbia: D.C.; Minute: min; Miles per hour: M.P.H.
The corona virus disease 2019 (COVID-19) pandemic in the first year resulted in more than 98 million cases worldwide, and more than over 24 million cases in the United States (U.S.) [1]. In early 2020, 43 out of 50 states and District of Columbia (D.C.) imposed shelter-in-places orders, with travel restrictions and work from home mandates aimed to slow disease transmission and manage health care resources [2]. These resultant lifestyle restrictions contributed to overall decreased physical activity [3,4], with increased sedentary and unhealthy eating behavior [3,5]. During the first year of the pandemic 28 - 61% of adults in the U.S. reported unintended weight gain, with an average gain of 28 - 44 lbs gained [4,6]. Exercise behavior and fitness saw varied changes during the pandemic [7-9], and while no definitive relationship between COVID-19 and running performance has been established [7,10], small numbers limit insight.
Running popularity has steadily increased over recent decades [11], and early parts of theCOVID-19 pandemic saw an increase in weekly outdoor running by 55 - 117% [12]. While marathon participation decreased 11-fold during the pandemic, average finishing times were approximately 20 minutes faster than pre-pandemic times [13]. This runs counter to the last 20 years of consistently slower performance trends observed in over 28,000 U.S. races of varying distances [14]. Improved pandemic running performance in marathons may have been a reflection of the greater exercise and training opportunities due to pandemic-mandated work from home schedule flexibility [15], although insight is limited as the average age of pandemic runners was substantially younger which would have impacted outcomes [13].
A retrospective analysis of finishers at the world's largest 10 km road race was conducted and controlled for age and regional mitigation efforts and infectivity rates for insight into the influence of the COVID-19 pandemic on running performance.
This retrospective analysis of finishers from the Peachtree 10 km Road Race 2019 (pre-pandemic) and 2021 (pandemic) editions were obtained from publicly available results accessed on chronotrack.com using an automated data aggregation and post-processing routine.
All participants with finishing times from the pre-pandemic and pandemic 10 km races were included for analysis. Available data fields included participant name, age, sex, bib number, chip time, home town, state, division, and rank (overall and within division). Participants who competed in both races were matched by the name, hometown and consistent age. Ethical approval was obtained from Stanford University institutional review board.
Pandemic variables were analyzed between March 1, 2020 and March 1, 2021. March was chosen as an initial starting point as COVID-19 was officially declared a pandemic on March 11, 2020 by the World Health Organization and the first shelter-in-place order issued by California on March 19, 2020 [16]. Mitigation restrictions analyzed included number of months with a shelter-in-place order, mask mandates, and gym closures. For data analysis, the duration of the restrictions were approximated categorically: 0 - 4 weeks was considered one month, 4.1 - 8 weeks as two months, etc. As not all mandate timing was contiguous, the total number of weeks were aggregated prior to month approximation. This data was obtained from per-state publicly available sources. (Appendix)
Hospitalizations and deaths from COVID-19 per state were utilized as a measure of disease severity. The total incidence and mortality per 1000 people per state in the 12 months preceding the 2021 race were calculated utilizing data from the University of Minnesota COVID-19 tracking project [17].
Pace differences between study years were tested for differences in means using the Welch two-sample t-test and Wilcoxon Rank Sum test. Paired versions of these same tests were used to assess differences in race pace for individuals who competed in both years. To assess the impact of state COVID mitigation precautions on performance, these same tests were utilized for participants grouped by state with the Holm method applied to adjust the p values for the 50 multiple comparisons. To assess the relationship between stay-at-home, mask mandates, and performance, we applied Pearson's correlation test. A multi-variate regression was used to analyze per-state infectivity rates and per capita infectivity with running groups (e.g., pace and time, controlling for age, sex, and division). All analysis was performed using the R environment for statistical computing version 4.1.1.
There were 84,790 runners analyzed, with 60,525 finishers pre-pandemic and 24,265 during the pandemic. There were 182 runners in 2019 whose hometown was not a U.S. state or D.C. and 44 in 2021. Pandemic runners were 1.4 min / mile faster on average than those pre-pandemic (12 versus 13.4 min / mile, 95% Confidence Intervals [CI] 1.34 to 1.45, p < 0.001). Finishing times decreased during the pandemic in both women (12.9 versus 14.3 min / mile, 95% CI 1.31 to 1.47, p < 0.001,) and men (11.3 versus. 12.5 min / mile, 95% CI 1.2 to 1.3, p < 0.001) (Figure 1). This improved performance trend was consistent across all age groups and sexes (Figure 2).
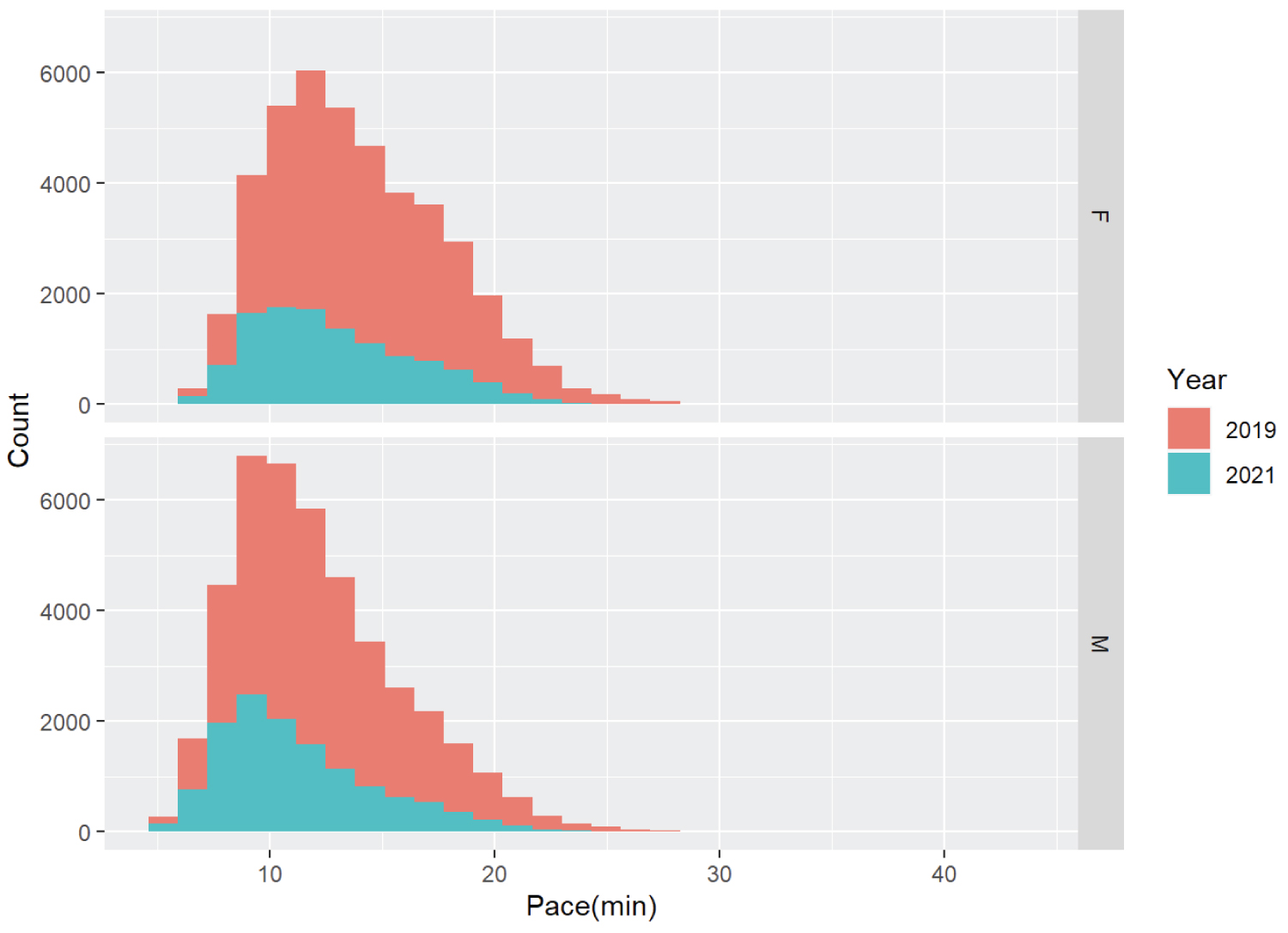 Figure 1: Race participants per year and average pace.
Figure 1: Race participants per year and average pace.
min = minutes / mile, F = female, M = male
View Figure 1
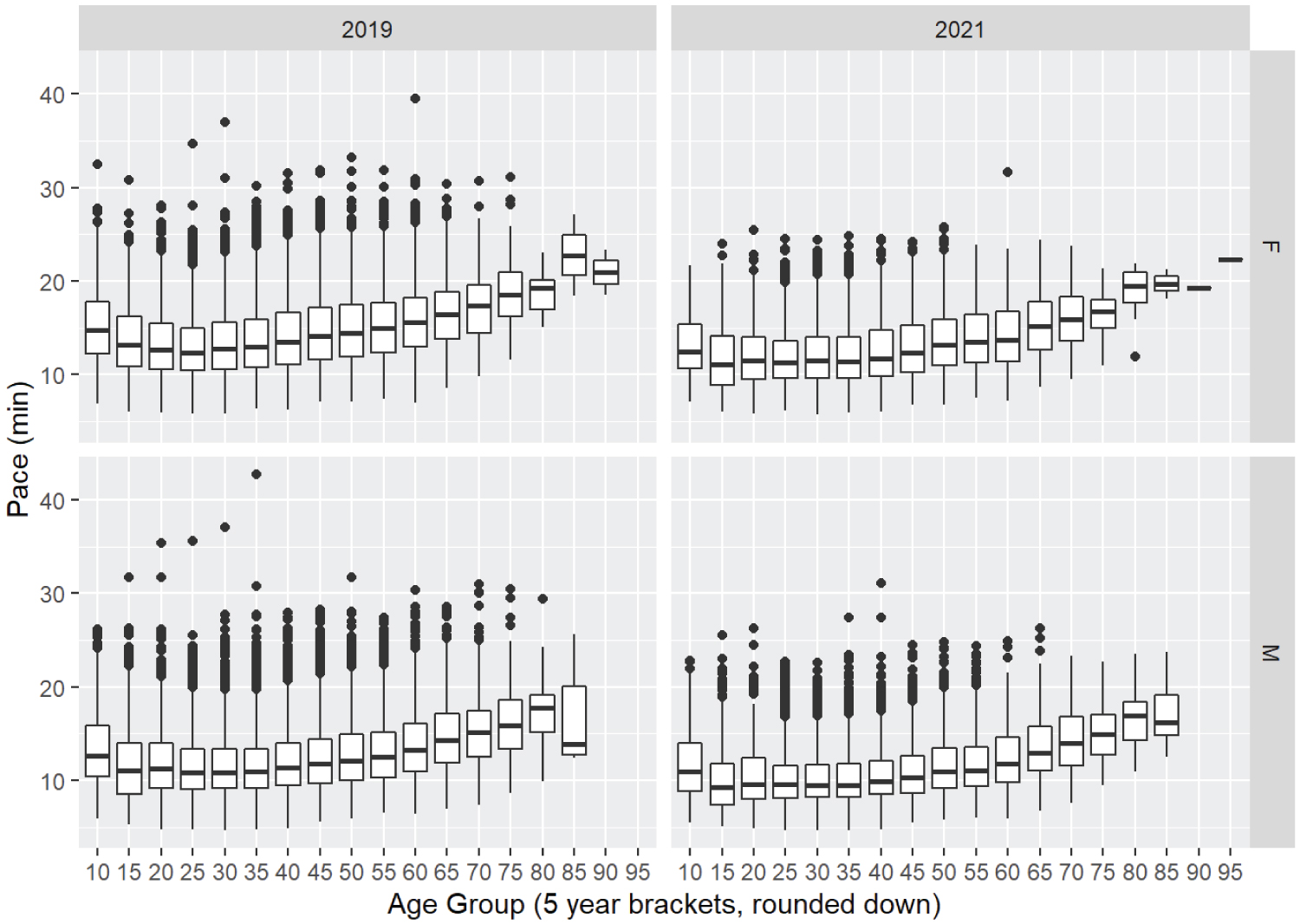 Figure 2: Age of race participants and average pace.
Figure 2: Age of race participants and average pace.
min = minutes / mile, F = female, M = male
View Figure 2
Of the 10,475 racers who participated in both races, pandemic times saw a 0.33 min / mile improvement (95% CI 0.29 to 0.37, p < 0.001). With improved performance in both women (0.35 min / mile, 95% CI 0.29 to 0.42, p < 0.001) and men (0.31 min / mile, 95% CI 0.25 to 0.37, p < 0.001).The greatest performance improvement was seen in those younger than 20 years of age (0.95 min / mile, 95% CI 0.74 to 1.16, p < 0.001) (Figure 3).
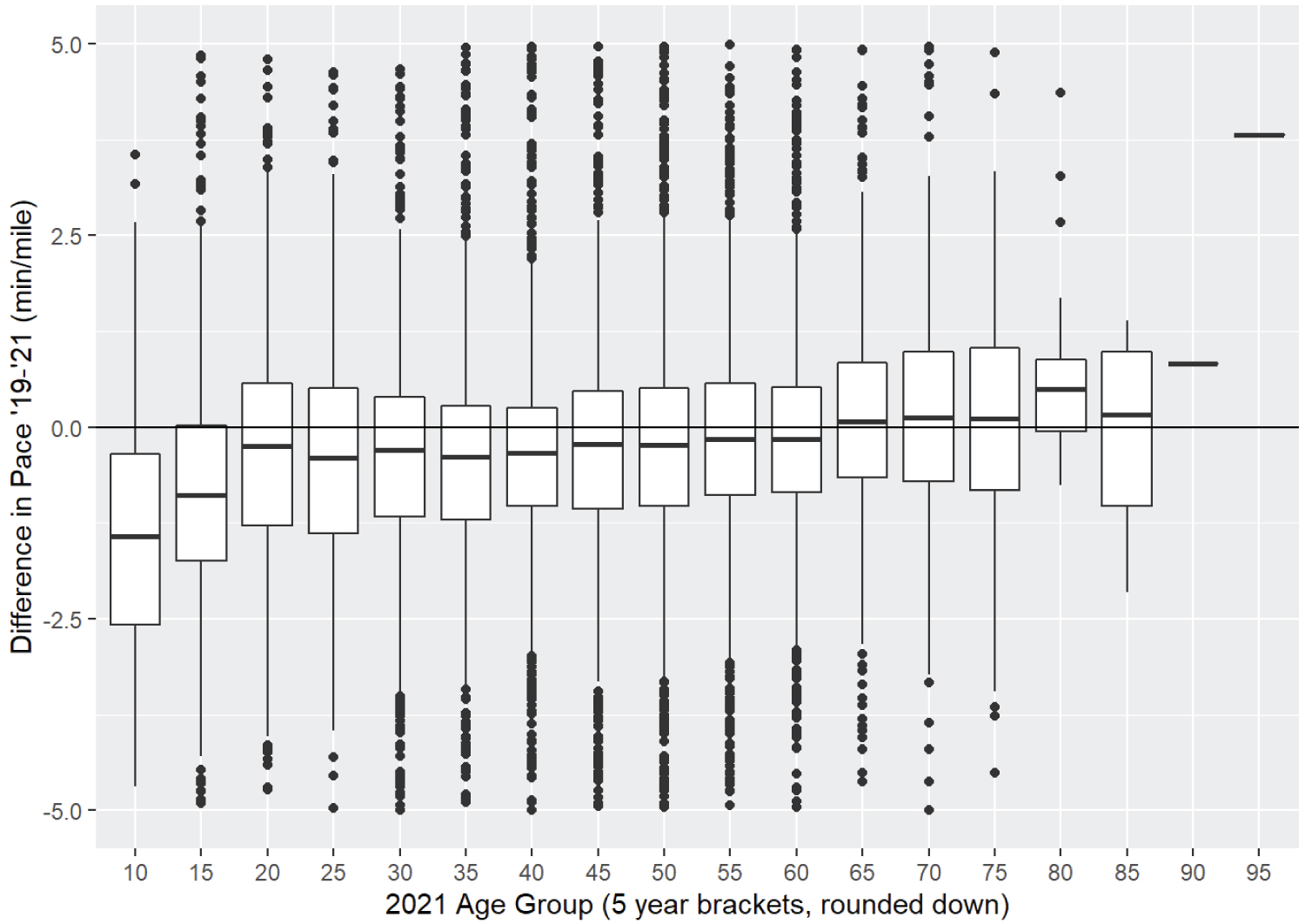 Figure 3: Age of race participants and differences in pace.
Figure 3: Age of race participants and differences in pace.
min = minutes
View Figure 3
Summarizing COVID-19 mitigation requirements averaged across the 50 states and D.C., 78% had mask mandates in effect for 6.8 months, 86% with shelter-in-place orders for 2 months, and 94%gym closures for 3.1 months. Weighted by state of residence among 2021 runners, the average mask mandate was 0.45 months, shelter in place for 1.1 month, and gym closure for 1.2 months.
Comparing runners' performance per state in 2019 and 2021, five states (Georgia, North Carolina, Ohio, Florida and Texas) had statistically significant improvements in pandemic pace (data not shown). Taking the mean change in pace between the years weighed for each state, there were no significant correlations with duration of mask mandates (r = 0.168, 95% CI = -0.14 to 0.45, p = 0.17), shelter-in-place (r = 0.237, 95% CI = -0.07 to 0.5, p = 0.16), or gym closures (r = 0.141, 95% CI = -0.17 to 0.42, p = 0.37). When grouping the runners by states without mask mandates (n = 79,988), pandemic finishers' time averaged 1.4 min / mile faster (13.5 to 12.1 min / mile, 95% CI 1.36 to 1.47, p < 0.001) compared to 1.2 min / mile faster in those states with mask requirements (n = 4,802) (12.7 to 11.5 min / mile, 95% CI = 0.95 to 1.42, p < 0.001). Too few individuals were from a state that did not impose shelter-in-place or gym closures to perform a similar analysis.
Among the 10, 475 runners who finished both races, per state pace differences and duration of COVID-19 mitigation requirements showed no significant correlation with mask mandates (r = -0.244 95% CI -0.55 to 0.11, p = 0.18), shelter-in-place (r = -0.243 95% CI -0.55 to 0.12, p = 0.18), or gym closures (r = -0.193 95% CI -0.51 to 0.17, p = 0.29). Analysis of repeat runners from states without mask requirements (n = 10,109) showed a greater pace decrease (0.33 min / mile, 95% CI 0.28 to 0.37) compared to those states with mask mandates (n = 366, 0.32 min / mile, 95% CI 0.12 to 0.56). Too few repeat runners lived in a state that did not impose shelter-in-place or gym closures to analyze.
There was a strong association between hospitalization incidence and mortality from COVID-19 during this time (r = 0.588 95% CI 0.32 to 0.77, p < 0.001). Runners' performance changes were poorly correlated with COVID-19 severity in the 12 months preceding the race by both per state hospitalizations (r = < 0.001 95% CI = -0.37 to 0.37, p = 0.99) and mortality (r = 0.009 95% CI = -0.29 to 0.31, p = 0.95). These results were similar with the repeated race participants' state hospitalizations (r = 0.144 95% CI = -0.32 to 0.55, p = 0.54) and mortality (r = 0.103 95% CI = -0.25 to 0.44, p = 0.57). When a shorter time frame of 3 months preceding was analyzed as a potentially more accurate temporal reflection of population health in the runners' state, slower pace was significantly correlated with per capita mortality rates per state (r = 0.418, 95% CI = 0.13 to 0.64, p < 0.01), but not hospitalizations (r = 0.054, 95% CI = -0.33 to 0.42, p = 0.78). In the repeat runners' performance, slower pace was not correlated with mortality (r = -0.154, 95% CI = -0.48 to 0.21, p = 0.4) or hospitalizations (r = 0.316, 95% CI = -0.15 to 0.67, p = 0.17). States with a high disease burden still had a large increased proportion of participants (Figure 4).
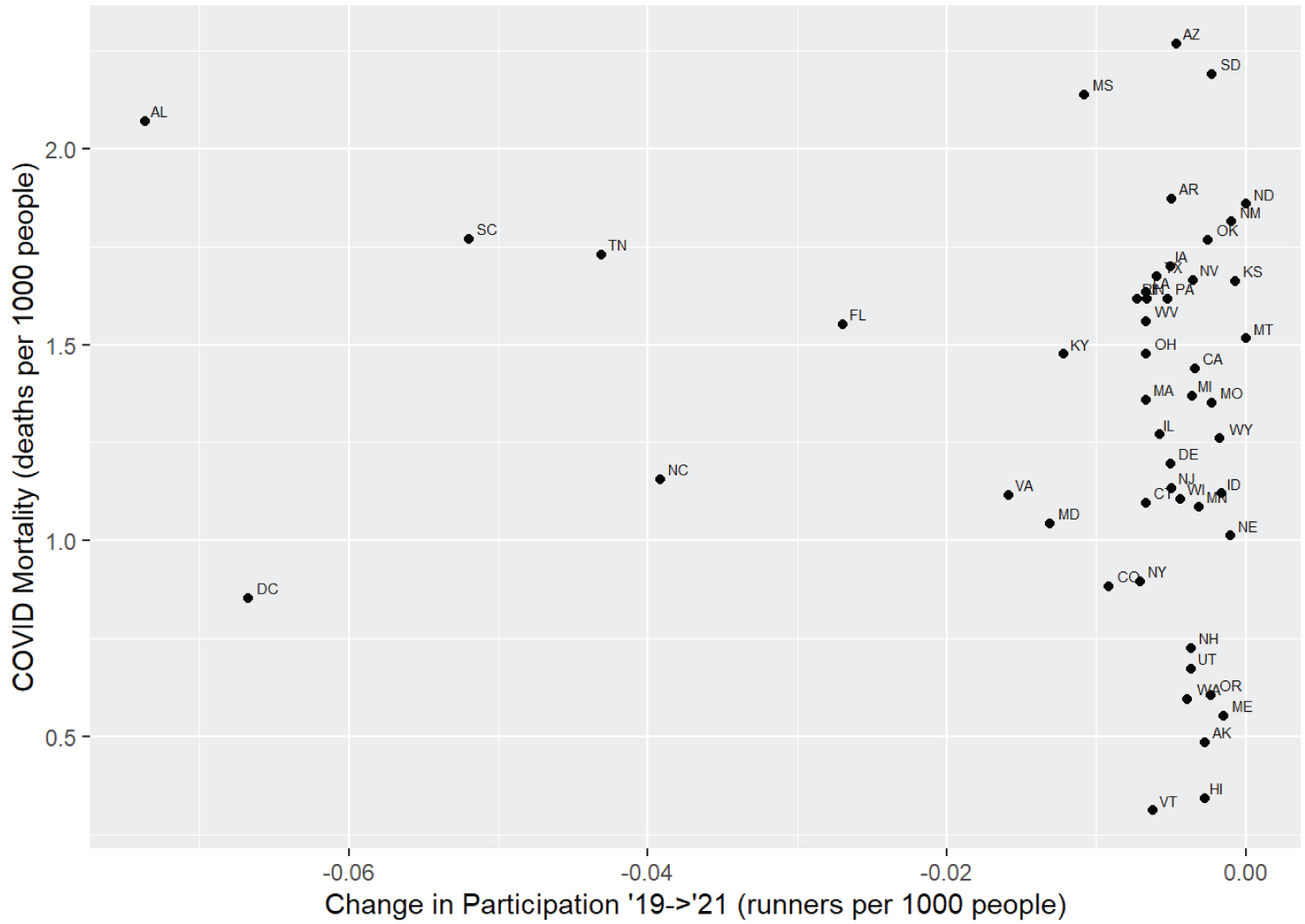 Figure 4: Change in participation per year and COVID-19 mortality.
View Figure 4
Figure 4: Change in participation per year and COVID-19 mortality.
View Figure 4
In this analysis of the 84,790 runners at the Peachtree 10km Road Race in 2019 and 2021, finishers in the pandemic era averaged 1.4 min / mile faster pace than pre-pandemic and 0.33 min / mile faster in the 10,475 racers who participated in both races. This improved performance was unlikely due to more elite runners participating in the pandemic edition, or older participants staying home [13], as consistent performance improvements were observed across all ages in addition to the repeat runners (faster although 2 years older in the pandemic edition). The COVID-19 pandemic caused more than one third of households in the U.S. workforce to transition to tele work, with an increased amount of time working from home [18]. Tele work improves flexibility in the working schedule, and U.S. adults averaged 32 minutes more per day on physical activity than prior to the pandemic [19]. Physical activity has been shown to be an important determinant of health during pandemics [20], and 27% of households with a tele worker reported their health status as excellent, compared to 80% with no tele workers who reported their health as poor [18]. Forty-three percent of tele workers in the U.S. used the time saved while working from home on exercise, and applying 11% of the time typically spent on commuting to exercise [21,22]. Europeans during shelter-in-place increased their activity by 36 - 58% compared to pre-pandemic levels [23], and wearable GPS technology reported a 5% increase in recorded activities during work day times over the first 7 months of the pandemic [24]. It is reasonable that these pandemic-dictated lifestyle changes contributed to increased exercise and fitness as reflected in the observed improvements in running performance, similar to the increased pace in over 80,000 marathon runners reported over the same time [13].
Pandemic mitigation efforts led to widespread gym and exercise facility closures, which likely led people to turn to the outdoors for exercise. A study of popular outdoor exercise applications found a 28 - 68% increased amount of running miles from early to middle of 2020, compared with to the year prior [24]. Fifty-nine percent of surveyed adults chose outdoor exercise (including running) to reach their fitness goals in 2021, compared to 15% the year earlier [25]. We hypothesized that runners from states with greater mitigation requirements may have seen improved performance, as outdoor running could be preferable to inaccessible or inconvenient indoor exercises. However, there was no substantial evidence that participants from states without a mask mandate performed better or worse. These results are consistent whether analyzing all participants' performance as a group or using a paired analysis comparing only those participants who attended and competed in both races. When runners were grouped by states without mask mandates, pandemic runners were 0.6 min / mile slower than those from states with mask requirements, but had a statistically significant improvement in performance. Similar results were seen in the repeat runners. As 94% of the pandemic runners and 97% of the repeat race participants were from states without mask mandates, we are cautious about drawing conclusions regarding the association of mask mandates with running performance.
Unsurprisingly, there was a strong correlation between the incidences of COVID-19 hospitalizations and per capita mortality rates. We analyzed incidence of state-wide COVID-19 severe enough to require hospitalization in the 12 months and 3 months preceding the race as a surrogate for general population-level health, but there was not convincing evidence that increased severity of COVID-19 in the racers' locale was associated with poorer running performance. There was concern that runners from states with a higher disease burden may have been less likely to participate in the pandemic race, which would have limited insight into the relationship of COVID-19 regional infectivity and performance. While there may have been a weak correlation among those states with the smallest changes in participation, this association was not seen in states with extremely high disease burdens, which had nearly the same proportion of runners participating in both races.
Gathering accurate data for the duration of per-state pandemic mitigation stipulations required sourcing multiple local news agencies, which resulted in substantial unavoidable source variability. While some gym closure data fell under the category of"indoor businesses" and under the jurisdiction of state regulations, some larger states had per-county variability so it was necessary to apply the date of the first gym opening to the entire state, although this was not necessarily representative. Implementation of some emergency mitigation orders may have lagged several days after the recorded date of announcement, which would have introduced some temporal inaccuracies. Shelter-in-place orders had various terminology throughout the U.S., including"shelter at home,""stay at home," and"safer at home," with regulation strictness that varied from $100,000 fines and threats of incarceration, to a general encouragement to stay at home when able. As such, the influence of each states' policies would have a disparate impact on peoples' behavior. There were 16 states that did not report public hospitalization data during the study period, and while this represented only 2.5% of the studied population, it introduced inaccuracy to this infectivity metric. Additionally, although the race was held on the same date both years, the pandemic edition was 9°F cooler with 9% lower humidity [26], factors that have been associated with faster endurance running [27], and may have contributed to faster performance. The pandemic race's wind speed was 0.9 MPH faster than pre-pandemic, which may have contributed to slower times if it was a directional headwind. Due to the relatively short length of the race, these weather differences are unlikely to explain the performance results found for all demographics of runners. Filters applied to identify repeat racers excluded any participants who moved between races, but more importantly limited potential for ambiguous matches. The majority of race participants and repeat racers were from 5 states, and these were less impacted by COVID-19 precautions than the average U.S. citizen. As such, care should be taken when generalizing mitigation impacts to states where data is more limited. Finally, generalization of pandemic lifestyle changes could not be assessed in our analyzed population, so quantifying the influence of these factors is limited.
Pandemic-era 10 km runners improved running performance over pre-pandemic times, consistent with marathon runners and in contrast to decades of road racing trends. There was no significant association of running performance with per-state COVID-19 mitigation restrictions or infectivity, which was reinforced by analyzing the runners who repeated the race both years. By controlling for measurable pandemic variables that may have impacted the performance outcomes, unmeasurable societal lifestyle changes such as working from home may have improved running performance.
There was no external funding or support for this project. The authors report no conflicts of interest.