Muscle dysmorphia, a form of Body Dysmorphic Disorder, is marked by an intense preoccupation with muscle size and body image, often leading to excessive physical activity, restrictive eating habits, and the misuse of dietary supplements.
We report the case of a 16-year-old boy with muscle dysmorphia who presented to the emergency department with sudden-onset chest pain and was diagnosed with pneumomediastinum. Etiology was attributed to elevated intrathoracic pressure during strenuous weightlifting exercises, combined with dietary restrictions that may have weakened the alveolar walls.
This case is the first to document pneumomediastinum associated with muscle dysmorphia, highlighting the risks posed by excessive exercise and rigid dietary behaviors. By sharing this report, we aim to raise awareness among healthcare providers about the potential for rare medical complications in muscle dysmorphia, emphasizing early recognition and intervention to prevent adverse outcomes.
Muscle dysmorphia, Pneumomediastinum, Eating disorder
BDD: Body Dysmorphic Disorder; CK: Creatine Kinase; CXR: Chest Radiograph; ARFID: Avoidant/Restrictive Food Intake Disorder
Body Dysmorphic Disorder (BDD) is a mental health condition characterized by a persistent preoccupation with one or more perceived flaws or defects in one's physical appearance, which are often minor or not noticeable to others. This preoccupation can lead to significant emotional distress and impair an individual’s daily functioning [1,2]. Muscle dysmorphia, often considered a subtype of BDD , is a disorder characterized by individuals' intense desire to reduce fat mass and an obsessive focus on increasing muscle mass. This condition incorporates environmental factors such as the influence of media, personal insecurities, peer pressure, and dietary behaviors, in addition to personality traits like perfectionism [3].
Individuals with muscle dysmorphia are obsessed with being inadequately muscular and have an intense desire to increase muscle size or achieve a more "ideal" physique. Compulsive behaviors associated with this disorder might involve spending excessive amounts of time exercising in gyms, investing large sums of money in ineffective sports supplements, exhibiting abnormal eating patterns, or even engaging in substance abuse [3]. Some patients become so intensely focused on muscle development that they neglect social engagements, miss school, and continue training despite injuries rather than pausing their fitness routines. They may resort to the use of anabolic steroids and protein supplements, both of which can be associated with significant adverse effects when used over extended periods. An increase in creatine kinase (CK) levels related to high-intensity physical activity can be observed [4].
Pneumomediastinum , refers to the presence of air within the mediastinum, the central compartment of the thoracic cavity housing vital structures such as the heart, major blood vessels, esophagus, trachea, and bronchi [5]. Pneumomediastinum is often precipitated by an injury such as trauma or iatrogenic medical interventions such as endoscopy, tracheal intubation, or mechanical ventilation. Spontaneous pneumomediastinum is rare but can be caused by precipitating factors including activities causing elevated intrathoracic pressure, such as intense coughing, vomiting, Valsalva maneuvers, or strenuous physical exertion [5].
While pneumothorax and pneumomediastinum have been documented in the literature for patients with restrictive eating disorders like anorexia nervosa [6], our comprehensive literature search did not reveal any reported cases of pneumomediastinum in patients with muscle dysmorphia. In this case report, we present a patient with muscle dysmorphia who manifested pneumomediastinum.
We present the case of a 16-year-old boy with muscle dysmorphia who presented to the emergency department with a complaint of chest pain. The patient, aiming to increase muscle mass, engaged in weight training for 1-1.5 hours, six days a week, followed a diet with restricted carbohydrates and fats while increasing protein intake, and used supplementation with L-arginine and glycerol. Over the past three months, he had lost 13 kg through diet and exercise. Based on these clinical findings, he was diagnosed with muscle dysmorphia and had been followed by the Division of Adolescent Medicine and Child Psychiatry Department at Hacettepe University for the previous nine months before presenting to the emergency department.
The patient, who had recently been discharged after a 10-day hospitalization for bradycardia and nutritional management, was advised to avoid physical exercise. However, despite this recommendation, he engaged in heavy weight lifting exercises for 1.5 hours on the day of discharge and the following day. Two days after discharge, the patient presented with chest pain to the hospital.
Since that morning, he had been suffering from severe, sudden-onset chest pain beneath the sternum, which worsened with swallowing. The pain didn’t radiate to the neck or arms, and he didn’t report a history of chest trauma. His daily intake was 4000 kcal, as recommended at the time of hospital discharge.
At presentation, his body mass index was 23.1 kg/m 2 (weight: 75.0 kg; height: 180 cm). His peripheral oxygen saturation was measured at 98%, and his vital signs were within normal limits. Upon physical examination, both hemithoraces participated equally in respiration, with no evidence of tachypnea or retractions; however, a crunching noise synchronous with systole (Hamman sign) was revealed. Pneumomediastinum was detected on his posteroanterior chest radiograph (CXR) (Figure 1) and subsequent computed tomography of the chest confirmed pneumomediastinum (Figure 2). There was no evidence of esophageal perforation, either clinically or radiologically. No pathological findings were observed on the electrocardiogram. His laboratory investigations, which included cardiac enzyme, CK, glucose and electrolyte levels, complete blood count, sedimentation rate, liver and kidney function tests were all within normal ranges.
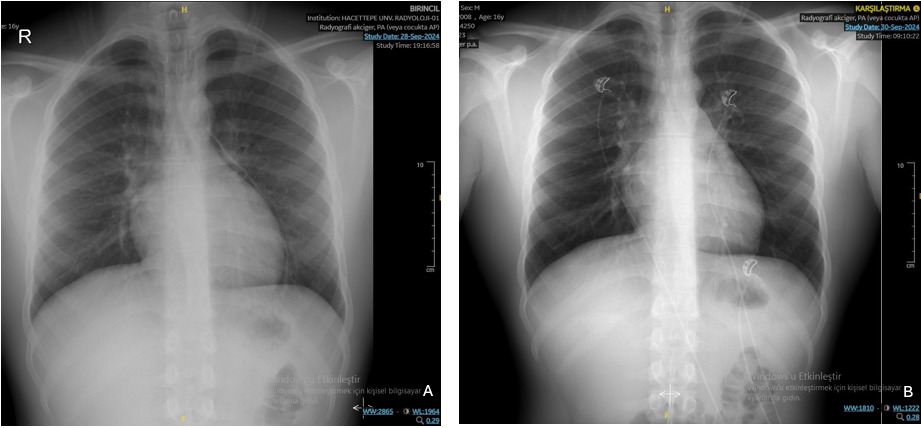 Figure 1: A) Chest X-ray at the time of admission and B) on the second day of hospitalization.
View Figure 1
Figure 1: A) Chest X-ray at the time of admission and B) on the second day of hospitalization.
View Figure 1
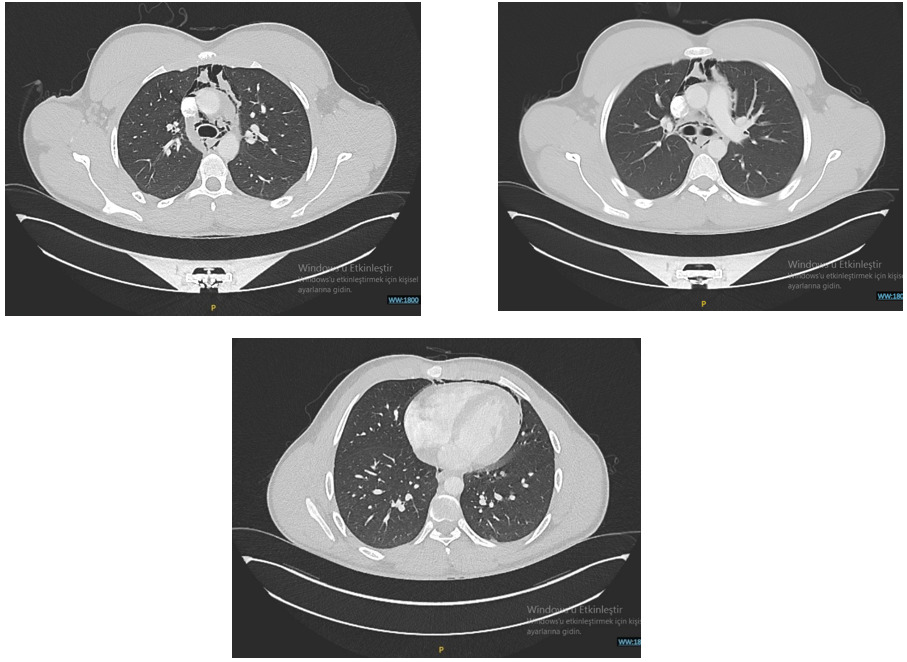 Figure 2: Computed tomographic chest image without contrast, demonstrating pneumomediastinum.
View Figure 2
Figure 2: Computed tomographic chest image without contrast, demonstrating pneumomediastinum.
View Figure 2
The patient’s pneumomediastinum was managed conservatively with supplemental oxygen therapy and bed rest. His chest pain improved, and a CXR performed on the second day confirmed the complete resolution of pneumomediastinum. He was discharged after a five-day hospitalization. The patient is still provided with dietary and exercise counseling, and his regular follow up is carried out in close collaboration with adolescent medicine and child psychiatry.
Consent was obtained from the patient and their parents for the publication of this case.
This case highlights the complex interplay between muscle dysmorphia and its potential medical complications. While muscle dysmorphia is primarily considered a psychiatric condition, the compulsive behaviors associated with it, such as excessive exercise, can lead to significant physical consequences, as demonstrated in this patient who developed spontaneous pneumomediastinum. The absence of esophageal perforation and normal cardiac investigations in this case strongly suggest that the pneumomediastinum was induced by the increased intrathoracic pressure generated during intense weight lifting exercises. Pneumomediastinum has been previously documented in weight lifters, with its etiology often attributed to both alterations in intrathoracic pressure and direct trauma, such as when the barbell impacts the chest [7-9]. In this case, the absence of any reported chest trauma suggests that the pneumomediastinum was primarily induced by significant intrathoracic pressure changes associated with strenuous weight lifting.
Although muscle dysmorphia is not classified as an eating disorder, it shares several overlapping characteristics, such as significant focus on body image, restrictive behaviors, and rigid, intense exercise routines, all of which can lead to severe medical complications. The occurrence of pneumomediastinum in anorexia nervosa (restricting and binge/purge subtypes), and avoidant/restrictive food intake disorder (ARFID) has been previously reported in the literature [10,11]. Dieatary restriction in these patients is thought to lead to weakened alveolar walls and thinning of the connective tissue, resulting in alveolar wall rupture even with a minimal increase in intra-alveolar pressure [6,12]. Additionally, self-induced vomiting increases intra thorasic pressure and might lead to esophageal lacerations [10]. Considering these factors, patients with eating disorders may be at an increased risk of spontaneous pneumomediastinum [6]. Our patient was also known to follow a diet restricted in carbohydrates and lipids and recently had a history of hospitalization due to bradycardia, he may have additionally developed alveolar wall weakness as a result of an energy deficit.
To the best of our knowledge, the occurrence of pneumomediastinum in a patient with muscle dysmorphia has not been previously documented in the literature. Given our familiarity with the patient, we were aware of his preoccupation with weight lifting. However, had he presented to another clinic, the diagnosis might have posed a significant challenge, particularly if he had not disclosed the extent of his weight lifting activities. In patients with a well-developed physique, acute onset dyspnea, cough, neck pain or dysphagia pneumomediastinum should be included among the differential diagnoses.
This rare complication underscores the importance of recognizing muscle dysmorphia not only as a mental health condition but also as a driver of potentially life-threatening somatic complications,emphasizing the need for a multidisciplinary approach in managing this condition. Beyond addressing the psychological aspects of the disorder, healthcare providers must remain vigilant for physical complications resulting from excessive exercise, supplement misuse, and dietary practices. Early recognition and education about the risk sassociated with muscle dysmorphia are critical to preventing adverse outcomes such as pneumomediastinum. This case also highlights the importance of tailored care plans, particularly in adolescent patients, to ensure adherence to medical recommendations and to mitigate the risks associated with high-intensity physical activities. Further research is warranted to explore the prevalence and mechanisms of rare complications like pneumomediastinum in this population.
No funding was received for this case report.
All authors contributed equally to this case report.
The authors declare that they have no conflict of interest.