The improving survival rates and life expectancy of patients with pediatric-onset chronic diseases led to a rise in the number of individuals requiring transition to adult care. A successful Health Care Transition (HCT) is vital in ensuring therapy adherence, continuity of care, and positive health outcomes. Both pediatricians and internists are key stakeholders in the transition process and have equally valuable input in improving HCT policies and programs.
Pediatricians and internists in active practice at a private tertiary hospital (Manila Doctors Hospital) were selected randomly to participate in a 2-staged survey. The first stage asked for demographics, HCT experiences, and respondents concerns about the Pediatric-to-Adult healthcare transition process. Three reviewers independently analyzed the answers from stage 1 for themes to create a stage 2 Likert survey. The participants subsequently answered the stage 2 survey.
A total of 59 physicians (25 pediatricians, 34 internists) participated in the study, with 85% (50/59) being able to proceed to the stage 2 survey. Forty-eight percent (48%) of the pediatricians and 50% of internists had prior experience in HCT. The most frequently used method in transferring patients is through the use of a referral letter. Among pediatricians, 33% initiated the patient's HCT at age 18 while internists started accepting at 18-20 years-old. Among those who never had HCT experience, 38% of the pediatricians and 71% of the internists were utterly unaware of the concept. The notable concerns in the HCT process were physician trust, attachment to the pediatrician, and patient anxiety. The identified gaps include the lack of education and training among health care providers, late initiation of HCT, poor endorsement system, and lack or absence of structured HCT program. Both pediatricians and internists agree that HCT training among staff alongside uniform hospital protocols and guidelines are necessary.
HCT remains not a standard of care, as shown by the low percentage of respondents with past HCT experience. Moreover, HCT seemed to be an unpopular concept among the participants. Gender, age, and individual physician role may have influenced the respondents' views on certain HCT aspects.
Health care transition, Pediatric chronic diseases, Adolescent healthcare
With the advances in medical research and improvement in the management of chronic diseases, pediatric patients who have long-term conditions that once typically result in childhood mortality now live into adulthood. Thus there is a significant increase in the number of pediatric patients needing HCT [1].
In 2011, the American Academy of Pediatrics addressed this concern and released a report to highlight transitioning of patients who have chronic physical conditions to adult health care as one of its leading priorities [2].
In an executive summary published by the Association of Maternal & Child Health Programs (AMCH) and the National Academy for State Health Policy (NASHP) in 2017, a transition policy is recommended with consent information at age18 and age of transfer. This policy must be developed with consumer input and accorded to the patient and family starting at ages 12-14 and must be regularly evaluated as a component of ongoing care [3].
In an article by Mubanga, et al. [4], which explores the present status of health care transition, it was noted that HCT planning is not being currently practiced as a standard of care. Moreover, AAP deduced that 'transition planning when present at all, can be inexplicit, incomplete, or late' [2].
On literature review, current researches deal primarily with a single specialty (internist or pediatrician) or with a specific subspecialty group care [5-9]. This study aims to cumulate and collate both physician perspectives about HCT to ultimately ascertain the gaps in care and establish recommendations to reinforce this transition.
To determine the experiences and perspectives of pediatricians and internists of a private tertiary hospital (Manila Doctors Hospital) toward health care transition of pediatric patients with chronic disease.
1. To present demographic data of respondents.
2. To determine prior transition experience of respondents in terms of the following (previous HCT participation, manner of becoming part of transition team, means of transfer, age of patient on start of HCT, self-assessment on knowledge regarding HCT, satisfaction on previous HCT experiences). If with no previous experience, to determine awareness and willingness for HCT.
3. To determine transition perspectives of respondents in the ff aspects: patient and family involvement, clinical/medical, health care provider, institutional coordination process, psychosocial perspectives.
4. To use the obtained data from stage I survey to come up with stage II survey questionnaire using the Delphi method.
5. To compare the degree of agreement between pediatricians and internists on the generated statements about HCT.
6. To compare Likert ratings of health care providers in accordance with the following parameters: gender, age, type of practice (generalist vs. subspecialist), years in practice, and physician role.
Qualitative-Quantitative (Delphi Method) Study Design (Descriptive-Analytic).
October 2020 to March 2021.
Manila Doctors Hospital (MDH), a private tertiary hospital located in Manila, Philippines, was chosen for the study. A list of physicians from Pediatrics and Internal Medicine (IM) department from all subspecialties was obtained from the webpage hospital directory and the hospital's Information and Telephone System (IATS). Simple random stratification sampling was done using an online randomizer application with every second provider selected within a subspecialty area to acquire a workable sample of physicians from multiple disciplines. If there is only one consultant available per subspecialty area, he/she was automatically chosen. The allotment of the number of participants per subspecialty was based on proportion (number of physicians per subspecialty).
Inclusion criteria: Licensed and practicing physician at MDH (pediatrician or internist) and reads and understands the English language.
Exclusion criteria: Physicians who have retired or whose contact information cannot be obtained.
At 95% confidence level and 0.10 margin of error, the minimum sample size computed was 59. This was based on the total population of 65 pediatricians and 89 internists at Manila Doctors Hospital. This was distributed proportionately to the size of IM and pediatrics hence the result of 34 internists and 25 pediatricians. The study used 0.10 margin of error.
Below is the Sample Size Formula:
Population:
Internists = 89, Pediatricians = 65, Total Number = 154
Minimum sample size = 59 (By proportion: 34 internists, 25 pediatricians)
This study entailed the use of survey questionnaire which was distributed through print or online copy (Google forms). Informed consent was obtained from all the participants before entering the study. The survey was divided into two stages.
The stage 1 survey had three parts. The first part asked for demographic characteristics of the participant including age, gender, field of practice, subspecialty if any, years in practice, type of practice. The second part asked for participant's transition/transfer experience. The third part had an open-ended question that asked the participants to list concerns about health care transition in the following aspects: Patient and family involvement, clinical, health care provider, coordination process/institutional, and psychosocial.
As patterned from the study of Peter, et al. [4], the responses from part 3 of the stage 1 survey were evaluated to generate a stage 2 survey (25 items 5-point Likert survey). In the stage 2 survey, the participants were asked to rate each of the items on a scale of 1 to 5 (1 strongly disagree) (5 strongly agree).
A 2-stage Delphi method was utilized to obtain opinions of physicians pertaining to the transition from pediatric care to adult care. The first stage questionnaire was developed based on existing literature. A pilot test was done involving 5 participants (3 pediatricians, 2 internists). The questionnaire was further improved after obtaining feedback.
A total of 59 participants were recruited for the study proper, which comprised of 25 pediatricians and 34 internists.
Three (3) independent reviewers (physicians not belonging to the field of Pediatrics or Internal Medicine) evaluated the responses from part 3 of the stage 1 survey. The selected reviewers had varying physician roles: 1) Epidemiologist, medical research professor and clinician; 2) Family medicine physician; 3) Chief hospital administrator and clinician.
The responses from part 3 of the stage 1 survey were sent to the reviewers through email. The responses were anonymized whether they came from a pediatrician or internist. The reviewers were asked to independently evaluate the responses and identify the top 5 most common themes cited by the participants per category (1) Patient and family involvement; 2) Clinical; 3) Health care provider; 4) Institutional/coordination process; 5) Psychosocial). After the independent review, an online group discussion was done by the principal investigator (PI) together with the three reviewers. The most common themes identified by each of the reviewers were tabulated by the PI and aligned statements with a similar concept. During the discussion, the associated themes identified were used to generate a unifying statement. A total of 25 statements were generated (5 per category) to create a stage 2 5-point Likert survey.
All of the participants were invited for the 2nd stage survey. 50 out of the 59 participants (85%) (24/25 pediatricians, 26/34 internists) responded to proceed. At least three reminders were sent to the non-responders during the period of stage 2 survey data collection.
This research study adheres to the ethical principles stated in the Declaration of Helsinki by the World Medical Association (WMA). Confidentiality was upheld at all times. Informed consent was obtained from all participants. The study acquired an approval from the Institutional Review Board of MDH prior to its execution.
Descriptive Statistics such as mean and standard deviation were used to present continuous data while frequency and percentage for categorical variables. Median served as the middle response, measuring the central tendency. It was also used to present responses for Likert-type questions. Mann Whitney U test was utilized to compare results of two groups, while Kruskal Wallis in comparing more than 2 groups. To study the pediatricians 'and the internists 'specific perspectives Mann-Whitney U test was employed.
Likert scale response was presented using median and percentage for each statement. On comparing the different groups, there was a need to provide a single score measuring the perspective. This was obtained by adding the score of all the statements. The Kruskal-Wallis test explored differences in Likert ratings according to demographic characteristics. The level of significance is at 5%. MedCalc Statistical software version 19.4.1 was used to carry out statistical calculations.
Figure 1 summarizes the methodology for this study.
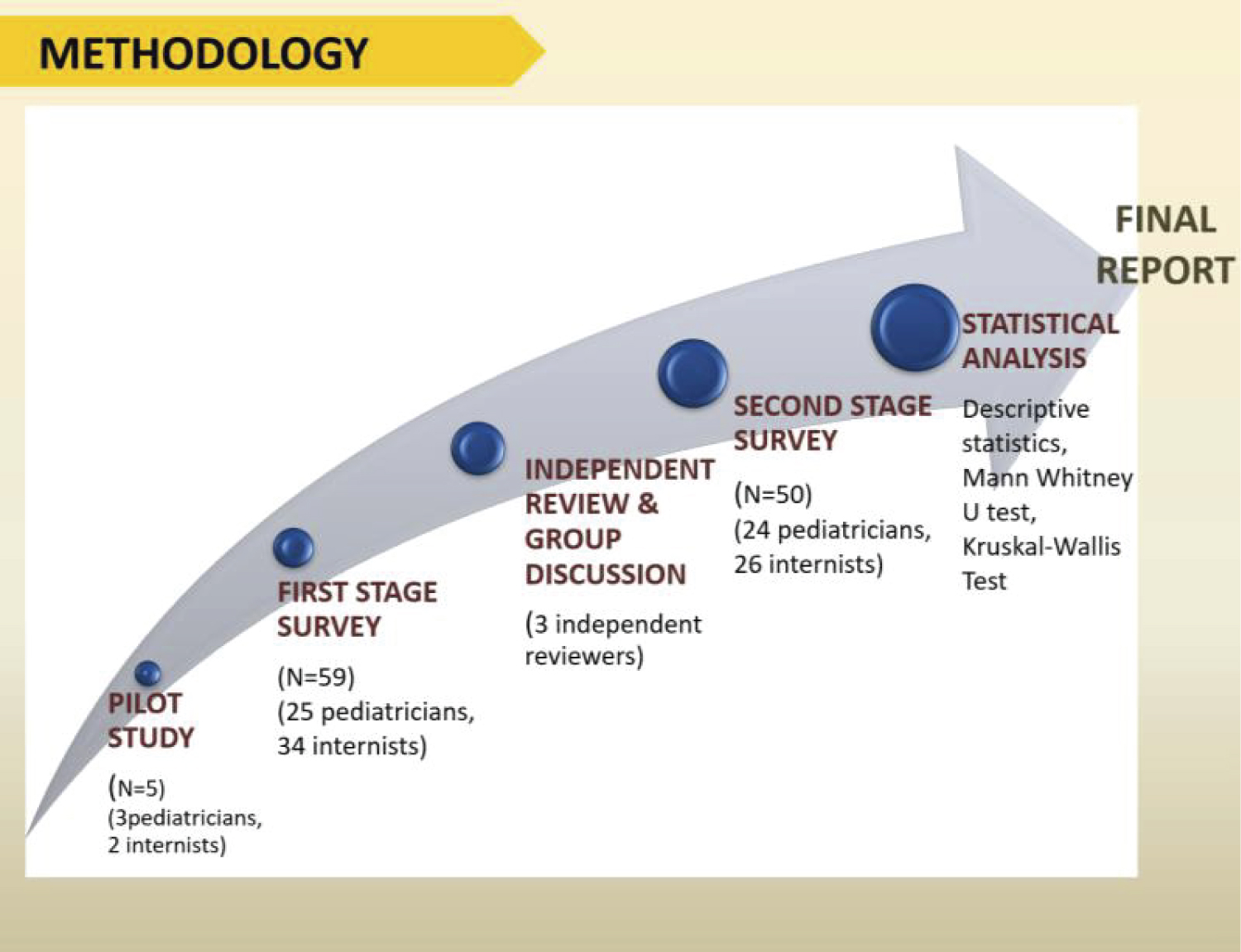 Figure 1: Study methodology.
View Figure 1
Figure 1: Study methodology.
View Figure 1
As shown in Figure 2, a total of 59 physicians (25 pediatricians, 34 internists) from MDH consented and participated in the study. Out of the 59, 50 participants (85%) proceeded to stage 2 survey (24 pediatricians, 26 internists).
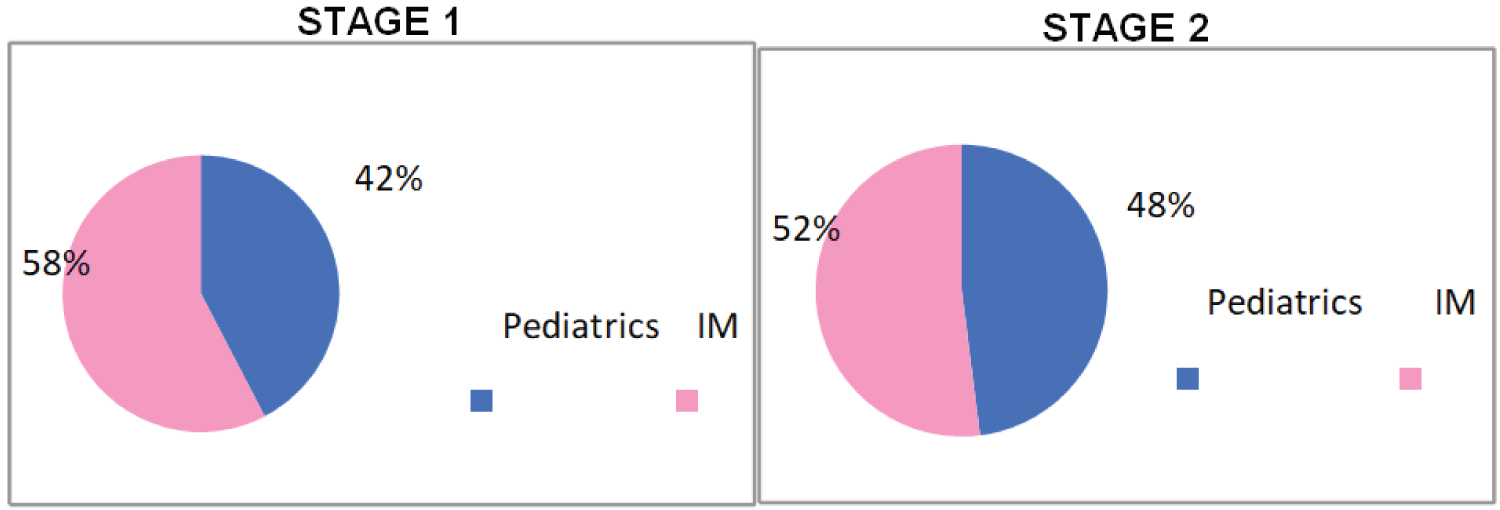 Figure 2: Comparison of stage 1 and stage 2 participants.
View Figure 2
Figure 2: Comparison of stage 1 and stage 2 participants.
View Figure 2
The participants had an age range of 39 to 65-years-old and a mean age of 49-years-old. As illustrated in Figure 3, the largest proportion of participants in both fields belongs to the 41-50 years age range for both stages.
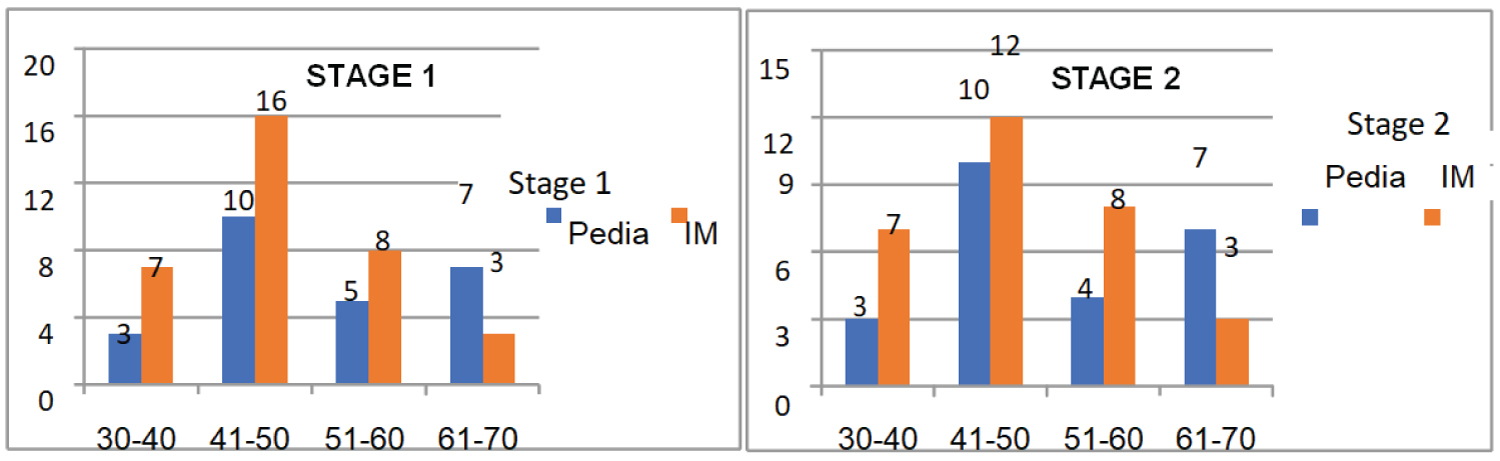 Figure 3: Comparison of stage 1 and stage 2 participants according to age.
View Figure 3
Figure 3: Comparison of stage 1 and stage 2 participants according to age.
View Figure 3
In stage 1, there were more females (88%) in the pediatric group while there were more males (53%) in the internist group. In stage 2, the majority in pediatric group still belongs to the female gender while in the IM group, from a male dominant group (53%) in the initial stage, it became evenly distributed in stage 2 (Figure 4).
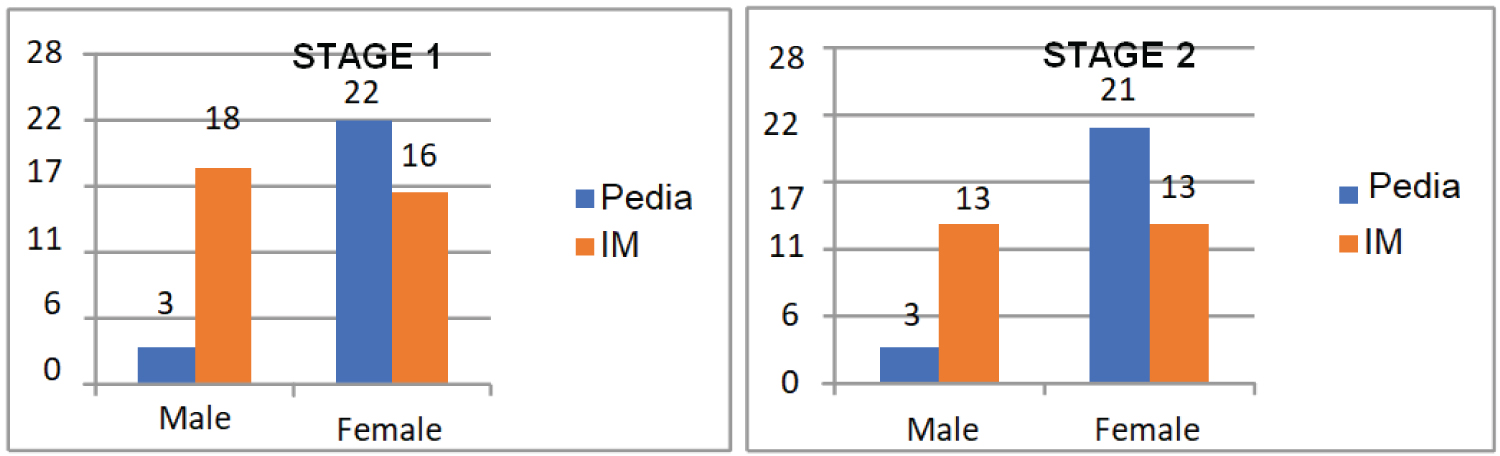 Figure 4: Comparison of stage 1 and stage 2 participants according to gender.
View Figure 4
Figure 4: Comparison of stage 1 and stage 2 participants according to gender.
View Figure 4
In stage 1, most of the pediatricians (32%) have been in the practice for 1-10 years. For the internists, 41% have been in practice for 1-10 years and another 41% for 11-20 years. In stage 2, the majority falls in the 1-10 years duration of service category for both IM and pediatrics (Figure 5).
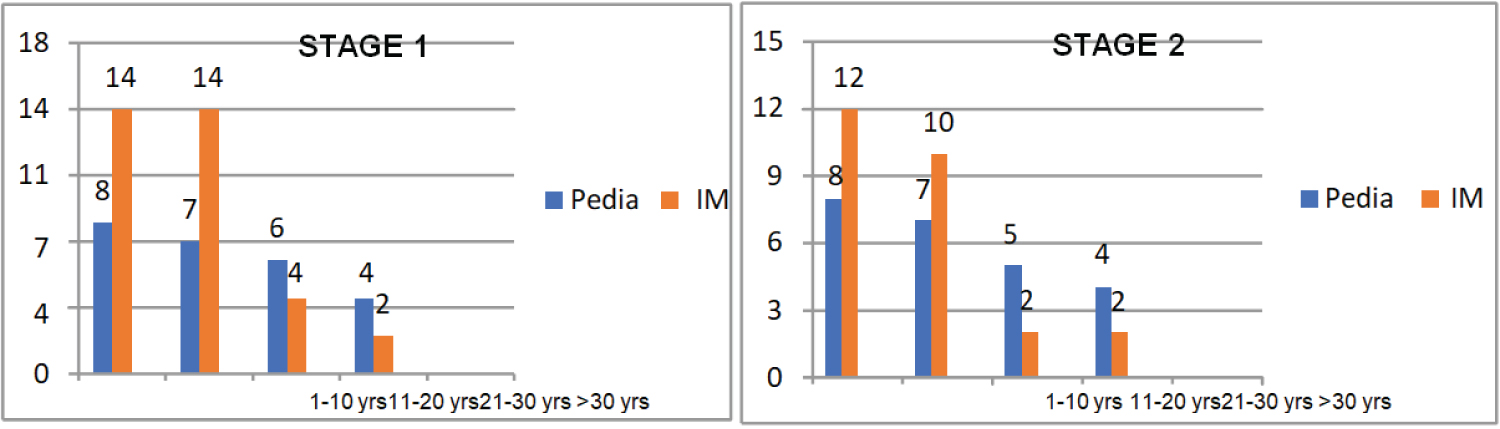 Figure 5: Comparison of participants in stage 1 and 2 according to duration of practice.
View Figure 5
Figure 5: Comparison of participants in stage 1 and 2 according to duration of practice.
View Figure 5
As shown in Figure 6, private practice followed by government practice is the most common physician role. Twenty percent of the pediatricians have an administrative job and another 20% are into academe. On the other hand, 18% of the internists belong to the faculty, 9% engages in administrative job and 3% into research. The ranking of physician roles remains unchanged in stage 2.
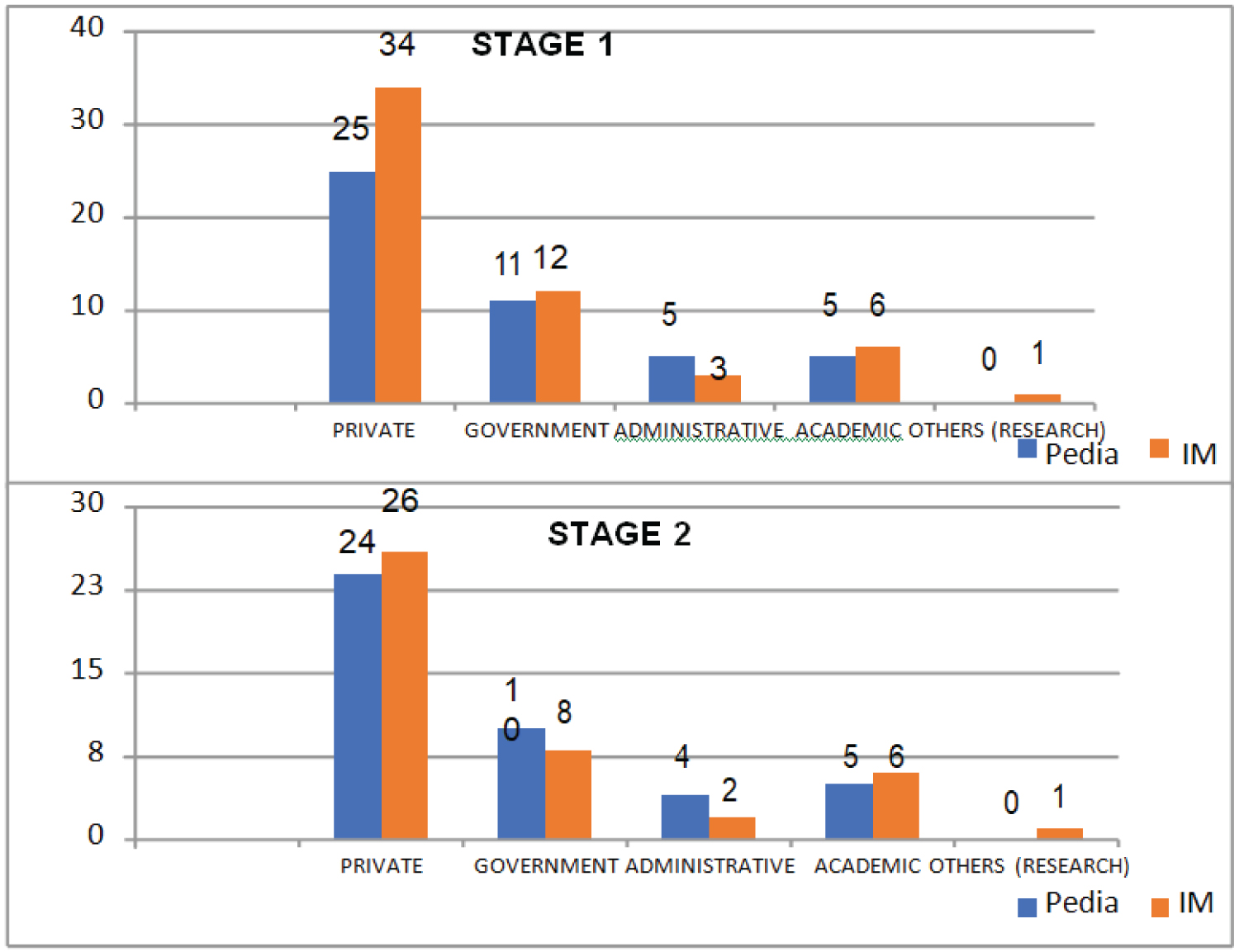 Figure 6: Comparison of stage 1 and stage 2 participants according to physician role.
View Figure 6
Figure 6: Comparison of stage 1 and stage 2 participants according to physician role.
View Figure 6
Majority of the participants in both fields are subspecialists (pediatricians 80%, internists 97%). For the internists group, only 1 available generalist is listed at the hospital webpage. In stage 2, all the nonresponders are subspecialists (Figure 7).
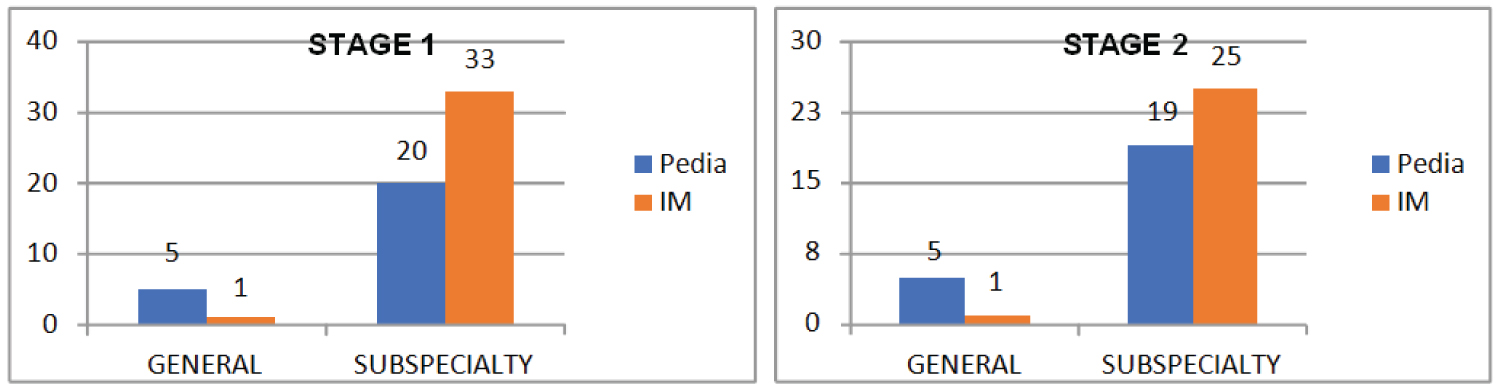 Figure 7: Comparison of stage 1 and 2 participants according to practice type.
View Figure 7
Figure 7: Comparison of stage 1 and 2 participants according to practice type.
View Figure 7
As allotted based on proportion or number of available physicians per subspecialty, the top specializations for pediatrics and IM are illustrated in Figure 8. The top ranking specialties remained unchanged for stage 2.
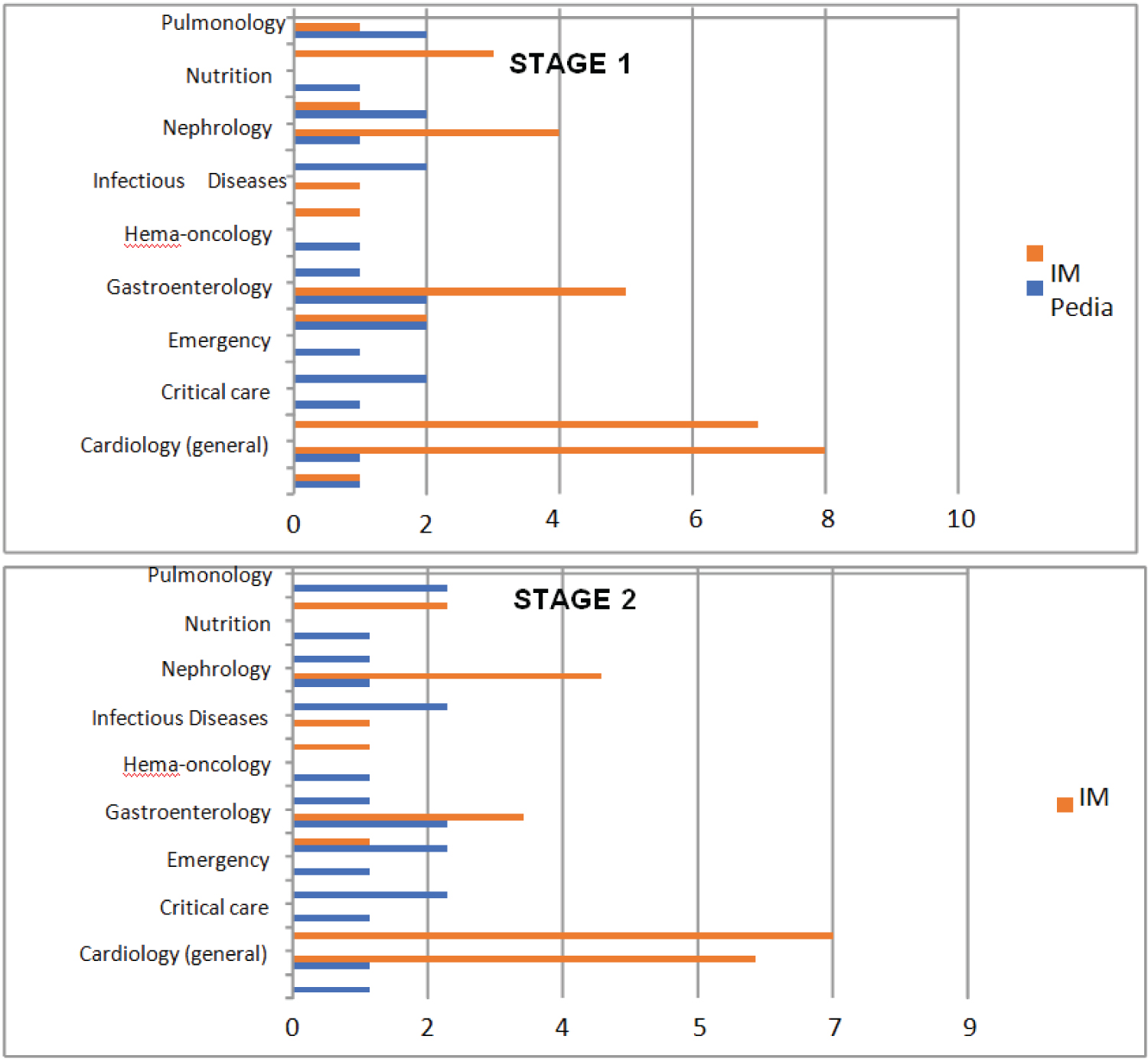 Figure 8: Comparison of stage 1 and stage 2 participants according to specialization.
View Figure 8
Figure 8: Comparison of stage 1 and stage 2 participants according to specialization.
View Figure 8
Forty eight percent of the pediatricians have previous participation in HCT process while half of the internists (50%) have previous experience and the remaining half never had experienced HCT (Supplementary File).
Among respondents with previous HCT participation, referral from colleagues is the most common manner of becoming part of HCT for internists. It is also the top answer for pediatricians but is tied to 'being a member of a specialty program'.
The most frequently used means in transferring patients for both pediatrician and internist groups is a referral letter. Among pediatricians, this was followed by transition clinic then phone call. On the contrary, internists ranked phone call as 2nd and transition clinics ranked 3rd. None of the participants have utilized electronic mail to transition patients.
Among the 12 pediatricians who have previous HCT participation, the majority (33%) started HCT at the age of 18. Among the 17 internists with previous HCT participation, 41% begin accepting patients for transition at age 18, while another 41% start at 19-20 years-old.
Out of the 13 pediatricians who had no previous HCT experience, 8 (62%) were aware of the concept. This contrasts with the internists, wherein out of 17, only 5 (29%) were aware of HCT.
Table 1 reveals that pediatricians have significantly higher mean rating on their self-assessment on knowledge about HCT of patients with chronic condition (p = 0.0044). Specifically, the mean of pediatricians of 3.8 is higher than 2.74. On the other hand, the two groups have no significant difference on their satisfaction on past HCT experience (3.91 Pediatrician vs. 3.65 Internist) as well as on their willingness to be part of HCT for pediatric patients with chronic condition (4.64 Pediatrician vs. 4.56 Internist).
Table 1: Participants 'satisfaction on past HCT experience, willingness towards future HCT participation and self-assessment on HCT knowledge. View Table 1
For part 3 of stage 1 survey, a total of 303 responses (122 from pediatrics, 181 from IM) were received with the most number of concerns belonging to the patient and family involvement category (82 responses: pediatrics 37, IM 45).
During the discussion with the independent reviewers, the most common themes identified under the patient and family involvement category are physician trust, patient willingness and attachment to pediatrician. Under the clinical/medical category, the top concerns are medication adjustment, record archiving, and differences in management guidelines between the two fields. Regarding to health care provider, the majority mentioned about endorsement and coordination between pediatrician and internist. Others cited continuity of communication post-transfer and competency of the counterpart physician. As for the institutional coordination process, top concerns are the lack of hospital protocol and guidelines on HCT. Others cited accessibility of records, personnel training and endorsement procedures. For the psychosocial perspectives, the top issues raised include patient anxiety, financial capabilities and psychological impact of HCT.
The generated 25 statements for stage 2 survey are shown in Table 2. The perspectives of the respondents on these statements (designated as statements 1, 2..) are further analyzed according to the their demographic characteristics and are shown in the succeeding tables.
Table 2: Comparison of stage 2 responses between pediatricians vs. internists. View Table 2
As shown in Table 2, all responses referring to patient and family involvement were not significantly different except for statement 1: patients undergoing transition often having difficulty trusting the new physician (p = 0.0178). Specifically pediatricians significantly agree more on this statement (3.79) as compared to internist.
All statements pertaining to both clinical/medical and healthcare provider themes turned out to have no significant difference between the responses of the two groups.
On institutional coordination process, results reveal that pediatricians significantly agree more (4.71) that residents, fellows, and consultants should be trained on proper referral system and transition process as compared to internist response (4.23). For the remaining statements, there was no significant difference between the two groups.
With regards to statements pertaining to psychosocial themes, results revealed a significantly higher agreement response by pediatricians as compared to internist on the following statements: patient anxiety and readiness should be addressed by both health care providers for a smooth transition (4.67 vs. 4.31), financial capability of the family is a primary concern during transition (4.08 vs. 3.46) and transition process should be able to address the psychological and emotional impact on patient (4.5 vs. 4.04).
Table 3 shows that female physicians as compared to males respondents significantly agree more that patients undergoing transition often have difficulty trusting the new physician (3.00 vs. 3.68), as well as on this statement: patients awareness and communication with the family regarding the transition process are both necessary (4.56 vs. 4.85). Similarly, female physicians have significantly higher mean (higher agreement) than male that there should be hospital protocol and uniformed guidelines in health care transition (3.75 vs. 4.32), as well as on patients anxiety and readiness should be addressed by both health care providers for a smooth transition (4.25 vs. 4.59). On the other hand, whether the physician is generalist or specialist, there is same mean agreement in all statements.
Table 3: Comparison of stage 2 responses of physicians according to gender and type of field and age. View Table 3
Comparing the response of the physicians according to age, all statements turned out to have the same response across all ages except on this statement: transition clinic must be conducive in establishing patient rapport and confidence to the new doctor (p = 0.0327). Specifically, younger doctors (30-40 years-old) significantly less agree (3.80) on this statement as compared to 41 to 50-years-old (4.46) and 61 to 70-years-old (4.60). In addition, Table 4 shows that the physicians' responses, when grouped according to the years of their service, are not significantly different for all statements.
Table 4: Comparison of stage 2 responses of physicians according to age and years in service. View Table 4
Table 5 shows that physicians who are in sole private practice significantly less agree on statements about institutional coordination process in particular to these statements: 1) There should be a hospital protocol and uniform guidelines in health care transition; 2) There should be inter-hospital coordination and referral system guideline for the transfer of care of patients; 3) Complete electronic records should be made available to the transition team and 4. Transition clinic/program should be established in all hospitals. The few transition clinics in the Philippines mostly are in public hospitals thus physicians engaged in private practice might have less exposure and experience. In addition, physicians who are in private practice less agree that the financial capability of the family is a primary concern during transition.
Table 5: Comparison of stage 2 responses of physicians according to physician role. View Table 5
On the other hand, physicians who practice at a government facility aside from MDH which is a private hospital have significantly higher mean agreement (4.39 vs. 4.00) that there should be a uniform guidelines in HCT (p = 0.04810). These physicians also have significantly higher mean agreement (4.39 vs. 3.84) on these 2 statements: 1) complete electronic records should be made available to the transition team; 2) Financial capability of the family is a primary concern during transition (4.28 vs. 3.47).
Physicians engaged into administrative work have significantly higher mean agreement on 5 statements: 1) transitioning of patients from pediatrics to adult care should start at early and must be gradual (4.67 vs. 3.84); 2) Communication and coordination between the pediatrician and internist should be continuous during transition process (4.83 vs. 4.25). They also have significantly higher agreement or mean; 3) There should be inter-hospital coordination and referral system guideline for the transfer of care of patients (4.83 vs. 4.14) (p = 0.0194); 4) A transition clinic or program should be established in all hospitals (4.67 vs. 3.86); 5) A patient for transition should undergo psychological evaluation (4.33 vs. 3.16). On the other hand, physicians belonging to the academe have significantly mean higher agreement of 4.40 vs. 3.85 that a transition clinic or program should be established in all hospitals (p = 0.0413).
This study aimed to determine the experiences and perspectives of pediatricians and internists of the selected private tertiary hospital toward HCT of pediatric patients with chronic disease. The demographic data of respondents showed that the study was able to acquire a population of multiple subspecialties with varying demographic characteristics with the goal of obtaining insights from a representative sample. The demographic characteristics of respondents were compared for both stages to verify representativeness, albeit only 85% of the participants proceeded to stage 2. Data showed minimal deviation from the first stage.
HCT experiences by the participants were identified. It showed that a significant percentage of participants in both pediatrics (48%) and IM (50%) have no previous HCT experience. This adds up to the previous inference that HCT is not currently being practiced as a standard of care. Results in this study showed that the most common manner of becoming part of a transition team is through a referral from/to a colleague, while the most common means in transitioning patients is through a referral letter. The use of referral letters alone could be troublesome for chronic and complex cases that need extensive details, especially when the family cannot accurately recall diagnostics and management done in the past.
Majority of pediatricians in this study initiate transition at the age of 18-years-old while internists start accepting pediatric patients by age 18-20 years-old. While earlier studies note varying ages of transition readiness, the suggested age of HCT initiation by expert consensus is at early adolescence or 10-13 years of age [2]. The role of pediatricians as the initiator of the process is crucial as starting HCT at early adolescence contributes to a smoother transfer of care. In this study, results showed that pediatricians significantly rated their HCT knowledge higher than internists. For those who previously participated in a HCT, the majority were satisfied with their experience. On the other hand, for those with no previous HCT experience, many physicians from both fields were unaware of the transition concept, with the internists being less aware (pediatrics 38%, internists 71%). This is a noteworthy finding as it suggests the lack of education and training about HCT among physicians, mostly with the internists. This is a similar finding in earlier research whereby a key challenge noted in transition is the absence of an identified adult health care provider to whom care can be transitioned [2].
This study endeavored to determine the HCT perspectives of respondents in varying aspects. As such, the stage 1 survey was able to receive a total of 303 responses which were summarized into themes to generate the stage 2 survey. In previous studies, barriers identified were logistic, bureaucratic, health information, and communication gaps [3]. In this study, HCT hurdles cited by the majority of respondents fall on the aforementioned categories. In particular, top concerns were poor endorsement, record archiving of long-standing cases, differences in management guidelines between pediatrics and internal medicine, personnel education and training, and the lack of standard hospital protocol on HCT.
The degree of agreement between the pediatricians and internists to the stage 2 survey statements was compared. The pediatricians in this study significantly have a greater agreement than internists that patients undergoing transition often have difficulty trusting the new physician. They also agree that the strong attachment and familiarity with them could be a hindrance to a smooth transition. This is the same finding identified by Gray, et al. [10] wherein "relationships" domain such as difficulty letting go of long-term bond with the pediatrician was regarded as a frequent transition impediment. Both pediatricians and internists disagree that medication dose adjustment can be difficult for the new physician. On the other hand, both physician groups agree that there must be a clinical pathway to reconcile the differences in guidelines between the two fields.
The Likert ratings for the stage 2 surveys were also compared in accordance to gender, age, type of practice (generalist vs. specialist), years in practice, and physician role. While there were certain statements to which female physicians significantly agree more than males, it showed that whether the physician is a generalist or specialist or when responses were grouped according to the years of service, there is the same mean agreement in all statements in all categories. Younger physicians significantly agree less than older physicians that transition clinics must be conducive in establishing patient rapport and confidence to the new doctor (p = 0.0327). Furthermore, when responses were examined according to physician role, physicians in private practice less agree significantly that the family's financial capability is a primary concern during HCT while those with practice at government facility believes otherwise. Physicians who have administrative roles significantly agree that a patient for transition should undergo a psychological evaluation.
HCT remains not to be a standard of care, as shown by the low percentage of respondents with past HCT experience. Moreover, HCT seemed to be unpopular given the poor awareness of the participants regarding the concept. The concerns cited on different HCT aspects were ground-level information involving transition key stakeholders (pediatricians and internists) whose insights are relevant to assess the current practices on HCT. Gender, age, and individual physician role may have influenced the respondents' views in certain aspects. Most of the statements generated in the stage 2 survey were agreed upon by both pediatricians and internists, therefore, creating a consensus as aimed by the Delphi technique. The identified gaps in HCT help point out the areas where improvements are necessary that may aid in drafting future HCT policies and programs. A timely, well-designed and well-executed transition from pediatric to adult care will help pediatric patients with chronic diseases reach their maximum health potential.
While this study reached the minimum sample size required, 15% of the participants did not respond for stage 2, which could have affected the stage 2 results. It is hereby recommended in future studies to increase sample size in case participants opt to drop out.
To develop a more effective HCT model, other stakeholders in the process such as the patient, family, and health institutions can also be engaged in future studies for a more holistic approach to the HCT process.
Special thanks to the independent reviewers who gave valuable insights in analyzing the survey responses: 1) Jose Ronilo Juangco, MD, MPH, FPSVI; 2) Jenifer Samson Lee MD, DPAFP; 3) Nimfa Santiago-Zarate MD, MPH.
Our deepest gratitude to all the physicians who, despite their busy schedule in the midst of a global pandemic, took time in participating for this research study.