Psoriasis and psoriatic arthritis (PsA) can affect the skin and musculoskeletal structures of the feet, raising the consideration of whether footwear has a role in clinical management. We summarized available evidence on how footwear (shoes, orthotics, insoles, and socks) can be utilized to supplement control of clinical symptoms in patients with psoriasis and PsA.
Four electronic databases were searched for articles reporting on patients with psoriasis or PsA and outcomes pertaining to the impact of footwear interventions on clinical symptoms. Two independent reviewers assessed titles and abstracts according to eligibility criteria, and evaluated relevant full texts for inclusion. Study design, participants, intervention(s), and outcomes were extracted for qualitative analysis.
We identified 177 articles, of which seven met eligibility criteria for inclusion in our review. Two studies were randomized controlled trials of synthetic material socks for plantar psoriasis, two articles were case reports on orthotic interventions for patients with PsA, and three articles were narrative reviews. We identified limited scientific evidence to support or refute the use of footwear interventions as therapeutic adjuncts in psoriasis or PsA. However, several authors hypothesize that minimizing shear forces in footwear, improving breathability, depth of footwear, and cushioning of insoles may reduce foot pain, disability, and functional limitations in patients with psoriasis and PsA.
Footwear interventions present a unique biomechanical opportunity in the management of psoriasis and PsA; however, to date, limited evidence exists to support or refute their efficacy suggesting a need for further research in this area.
Psoriasis, Psoriatic Arthritis, Shoes, Orthotic Devices, Foot Orthoses, Podiatry, Orthopedic Footwear
DMARDs: Disease-modifying anti-rheumatic drugs; MTP: Metatarsophalangeal; NSAIDs: Non-steroidal anti-inflammatory drugs; OCEBM: Oxford centre for evidence-based medicine; PsA: Psoriatic arthritis; PTFE: Polytetrafluoroethylene
Psoriasis is a chronic inflammatory skin disease with a worldwide prevalence of approximately 1-3% [1,2]. While generalized plaque psoriasis is most common, psoriasis can specifically affect the feet, such as palmoplantar psoriasis and pustular psoriasis, causing pruritus, pain during ambulation, and physical dysfunction. Approximately 25% of psoriasis patients also develop psoriatic arthritis (PsA), a chronic systemic inflammatory arthropathy which has a tendency to affect the foot and ankle with irreversible joint damage, achilles enthesitis, plantar fasciitis, and dactylitis [3,4].
It is well established that mechanical strain of the skin contributes to development of psoriatic skin lesions, potentially through a mechano-inflammatory mechanism - a process termed the Koebner Phenomenon [5,6]. Recently, it has been shown that psoriasis patients with a history of biomechanical trauma are also at greater risk of developing PsA, a process described as the deep-Koebner Phenomenon [7]. These observations raise the question of whether targeted interventions such as footwear, which biomechanically unload the skin, soft tissues, and musculoskeletal structures of the lower extremity, have any role in management of psoriatic disease involving the foot and ankle [8].
We sought to conduct a systematic review to summarize available evidence on how footwear (shoes, orthotics, insoles, and socks) can be utilized for control of clinical symptoms in patients with psoriasis and PsA. Given that footwear has not classically been discussed as a component of management in psoriasis and PsA, it is hoped that this study serves as a resource for physicians, podiatrists, and physiotherapists on the potential utility of footwear interventions in this patient population and can identify knowledge gaps for further research.
Our PICO-style question to guide this systematic review was "Can footwear interventions be utilized for symptom or disease control in patients with psoriasis or psoriatic arthritis?". MEDLINE, EMBASE, CINAHL, and Cochrane Central were searched on April 8, 2020 according to the search strategy shown in the Appendix. In brief, we considered MeSH and keyword terms relating to psoriatic disease and any footwear intervention including shoes, insoles, orthotics or socks. The reference lists for the identified articles were used to perform a secondary search. No limitations were placed on the date of study publication.
Articles were included in this review if they (a) reported on patients with psoriasis or PsA, (b) if they studied the effects of shoes, orthotics, socks or other forms of footwear interventions, and (c) if they reported clinical outcomes. No limitations were placed on study type or study date. Only studies published in English were considered.
Two independent reviewers (H.L., M.S.W-C.) first assessed titles and abstracts according to eligibility criteria, and articles were either excluded or progressed to full-text review. If insufficient information was available at the title/abstract review stage, full texts were evaluated. The two reviewers subsequently performed full-text reviews of all studies and identified articles meeting eligibility criteria (H.L., M.S.W-C.). Reviewers discussed all cases where discrepancies arose, and additional reviewers were available (L.C.C., R.T.L.) to assess articles for which discussion did not yield a unanimous decision.
A data extraction form was developed and utilized to document all relevant features from each eligible article, which included: first author, publication year, study design, participants, intervention(s), and outcomes.
The Oxford Centre for Evidence Based Medicine (OCEBM) Levels of Evidence, Treatment Benefits framework was used to establish a level of evidence for all individual articles, and an overall grade of recommendation for the data presented in this review [9].
The primary outcomes considered in this study were clinical symptoms relating to psoriasis or PsA. Given a high degree of heterogeneity in interventions used and outcomes assessed across a variety of study designs, data were synthesized qualitatively. This study was conducted and prepared in accordance with PRISMA guidelines [10].
The PRISMA flowchart details the study selection process and highlights reasons for study exclusion at each stage. In total, 137 records were screened initially, with seven articles deemed to meet eligibility criteria and inclusion in this review (Figure 1).
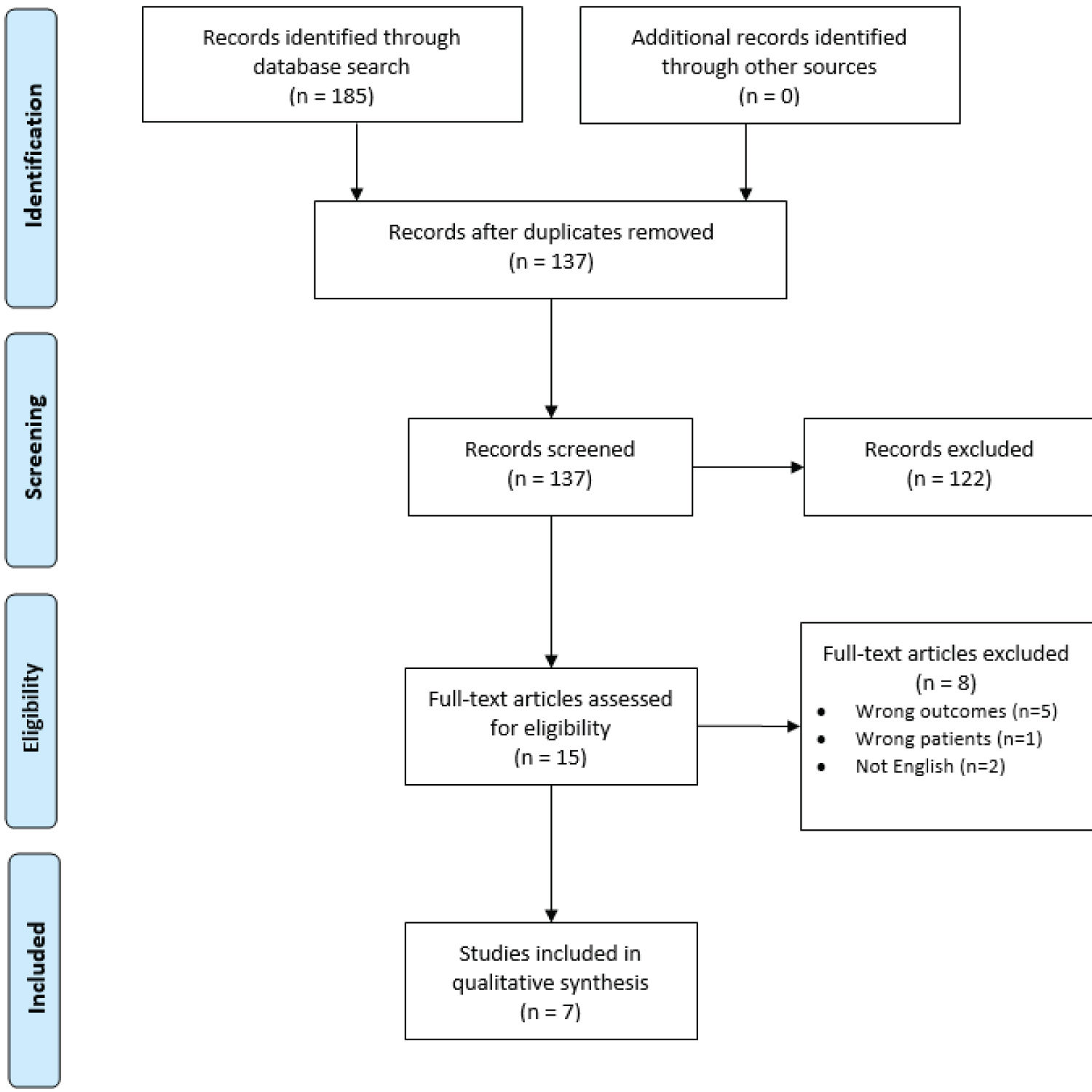 Figure 1: PRISMA flowchart for this study. View Figure 1
Figure 1: PRISMA flowchart for this study. View Figure 1
Data pertaining to the study participants, intervention(s), and outcomes were extracted from each of the seven included articles and are shown in Table 1. In total, four articles assessed patients with psoriasis, while three articles assessed patients with PsA. While foot orthoses were assessed most commonly (n = 3 articles), other interventions included fluorine-synthetic fiber socks, and specific characteristics of footwear including tightness of fit, use of moisture-reducing textiles, roughness of fabrics and material weight, sizing to accommodate pedal edema, and elimination of irritating hard toe-caps and stitching. Participants in the randomized controlled trials (n = 2 articles) and the case studies (n = 2 articles) included 26 females and 13 males, with an age range of 23 to 65 years. Clinical outcomes assessed by these studies included reduction in size and number of psoriatic lesions, pain reduction, functional improvement, and patient satisfaction. Three articles were narrative reviews with author perspectives and proposed hypotheses for the utility of footwear for psoriasis or PsA. Their evidence was largely based on using the clinical manifestations of psoriasis and PsA, such as skin inflammation, edema, pain, and deformity, to recommend the utilization of footwear which is accommodating and supportive.
Table 1: Summary of study features. View Table 1
The majority of the articles considered in this systematic review were narrative review with author perspectives (n = 3), while two were randomized controlled trials (open-label) and two were single-case reports. Based on this, the overall quality of evidence was graded as "C" using the Oxford Centre for Evidence Based Medicine criteria, representing an overall low level of evidence. A summary of individual study grading is provided in Table 2 [9].
Table 2: Study quality and overall quality of evidence. Quality level was based on the OCEBM Levels of Evidence Scale from 1-5, wherein level 1 represents the highest quality evidence and level 5 represents the lowest quality evidence. Overall grade of recommendation utilized a scale from "a" to "d" wherein "a" reflects consistent level 1 studies and "d" reflects consistent level 5 studies or troublingly inconsistent or inconclusive studies of any level. View Table 2
The two randomized controlled trials compared the effectiveness of fluorine-synthetic fiber socks and standard cotton socks on psoriatic lesional area reduction over a four-week period. The authors reasoned that a smooth-surface fabric such as this would improve psoriatic lesional area through friction reduction during walking and other daily activities. Among patients with plantar pustulosis, the median lesion reduction after four weeks was 42.6% in the fluorine-synthetic arm, and 2.7% in the cotton arm (p = 0.148) [11]. Among patients with plantar psoriasis, the median lesion reduction after four weeks was 11.95% in the fluorine-synthetic arm, and 11.89% in the cotton arm (p = 0.776) [12]. Among patients with plantar pustulosis, the overall change in lesion area over time was significantly in favour of the fluorine-synthetic arm (p = 0.045), as was the overall change in pathological condition perception over time (p = 0.025, assessed using an anchored horizontal 100-mm visual analog scale) [3]. Patient satisfaction score, assessed using a modified visual analog scale (patients marked according to the extremity which they believed had the best outcome), was found to be statistically significant for preference toward the fluorine-synthetic fiber socks among patients with plantar psoriasis (p = 0.011) [11,12].
One case report described the treatment course of a 47-year-old male diagnosed with polyarticular PsA, who experienced bilateral pain in the ankles, bilateral pain and stiffness in the first metatarsophalangeal (MTP) joints, achilles tendon pain, and heel pain [16]. This report analyzed the impact of several treatment modalities, including foot orthotics [16]. This patient’s orthotic intervention, which included a heel lift, medial arch support, metatarsal bar and soft poron top layer, specifically addressed force reduction through the Achilles tendon, stability of the subtalar joint, and protection of the first MTP joint. These interventions served to improve the patient’s symptoms in combination with other therapeutic modalities including non-steroid anti-inflammatory drugs (NSAIDs), disease-modifying anti-rheumatic drugs (DMARDs), exercise, and stretching [16].
The second case report described the experience of a 46-year-old female with psoriasis who developed psoriatic lesions consistent with a weightbearing (Koebner-based) distribution on the plantar aspects of the feet after beginning to play tennis [14]. Her exercise-based symptom exacerbation was then resolved through use of an orthotic which minimized vertical and shear forces during ambulation [14].
One narrative review described footwear intervention options for various arthritides, recommending that for people with PsA, footwear should be lightweight, sufficiently sized to accommodate swelling, and exclude hard toe-caps and stitching which can cause friction and result in Koebner-induced exacerbation [13]. Another report described multi-disciplinary management strategies for several rheumatic diseases, including PsA [15]. The authors suggested that early intervention with simple and functional foot orthoses can prevent deformity and reduce pain and disability among patients with rheumatologic conditions [15]. The final narrative review recommended features of orthotic and footwear interventions for patients with palmoplantar psoriasis, which included a tight fit to minimize friction, and breathability to minimize hidrosis and resultant irritation [17].
Observations of the Koebner and deep-Koebner Phenomenon raise the question of whether targeted interventions such as footwear, have any role in management of psoriatic disease involving the foot and ankle [8]. Therefore, the objective of this systematic review was to summarize available evidence on how footwear (shoes, orthotics, insoles, socks) and its role in biomechanically unloading the skin, soft tissues and musculoskeletal structures of the foot and ankle, can be utilized for management of clinical symptoms in patients with psoriasis and PsA.
Psoriasis and PsA impact foot-related pain and disability in different ways. The classic psoriatic rash, which involves erythematous and well-demarcated scaling plaques, is commonly found on the plantar surface of the foot [11,12,14,17]. This may in part relate to the Koebner phenomenon, in which psoriatic lesions are worse in areas subjected to pressure or friction [11,12]. These findings are usually bilateral, and are most common in the heel region, the lateral borders of the feet, and the metatarsals [14]. The Koebner phenomenon underscores the importance of appropriate footwear and textiles in the approach to psoriasis management [11,12]. Psoriatic arthritis, a condition seen in approximately 25% of psoriasis cases, commonly leads to foot pain, and if left untreated, deformity [4]. Individuals with PsA commonly suffer from swelling, inflammation, and pain in the distal digits and MTP joints [13]. Other common symptoms include ankle and foot pain, morning joint stiffness, and flattening of the medial and metatarsal arches [16].
In this systematic review, we have identified a lack of strong evidence to support or refute the role of footwear interventions in psoriasis and PsA. The current treatment arsenal for management of psoriasis and PsA includes analgesics and NSAIDs (for PsA), DMARDs (for psoriasis and PsA), topical corticosteroids (for psoriasis), ultraviolet light (for psoriasis), oral retinoids (for psoriasis), and biologic medications targeting inflammatory cytokines related to psoriasis and PsA [16,17]. Some of these treatments have remarkable efficacy in preventing and clearing skin lesions, or preventing further joint damage. However, occasionally patients with plantar or foot and ankle involvement will still experience residual skin lesions or have residual pain from prior joint or entheseal damage, rendering footwear intervention as an appealing, non-invasive and conservative adjunct for both the prevention and management of psoriatic symptoms. Indeed, in the rheumatoid arthritis literature it is more established that there is importance in addressing both inflammation and biomechanics in rheumatic disease [16] and it seems evident that further research is required in this area for psoriasis and PsA. This is especially true given the known association with the Koebner phenomenon, where tissue biomechanics may precipitate disease. Additionally, little interest has been paid to the relationship between skin health in psoriasis and textile materials [11,12].
It is well established that irritants can further exacerbate the manifestations of psoriasis in the foot and ankle [11,12] Further, trauma induced by normal forces or friction can contribute to the persistence of pustular lesions in keeping with the Koebner phenomenon [11,12,14]. The effects of skin trauma may therefore be further exacerbated in individuals who participate in athletic activity and thus subject the skin of the foot and ankle to more frequent, higher magnitude mechanical loading [14]. Similarly, higher loads at the foot and ankle could provoke injury, and potentially PsA onset or exacerbation [7,14]. Finally, it is known that patients with PsA can develop permanent joint or entheseal damage, and can have altered gait biomechanics [3,18]. For all of these reasons, footwear intervention as an adjunct to routine management in psoriasis and PsA patients seems intriguing and our systematic review highlights a few noteworthy considerations on this topic.
The use of fluorine synthetic fiber socks (Tepso GmbH, Lenzing, Austria), which are fabricated with strands of high-quality polytetrafluoroethylene (PTFE), has been proposed as a means by which to improve patient comfort [11,12]. PTFE is characterized by low surface friction against skin (coefficient of friction against skin is 2.5 times lower than cotton against skin under dry conditions, and 3 times lower under wet conditions, according to the manufacturer). PTFE is also chemically inert, biocompatible, and has non-stick and hydro-repellent properties, which collectively may prevent mechanical and chemical irritation of psoriatic lesions [11,12]. While the randomized controlled trials assessed in our systematic review did not show statistically significant differences in lesion reduction, these were both small studies with further investigation warranted. Interestingly, these studies did show that patient satisfaction was in favor of the fluorine-synthetic fiber socks and that disease perception had improved following four weeks in the fluorine-synthetic fiber sock. This should be considered against the notion that synthetic materials may contribute to excess sweating. A daily routine of washing, drying, and powdering the feet may reduce sweat-induced irritation; however, ultimately a breathable non-irritating material may need to be considered [17].
Specific footwear and orthotic interventions were also analyzed by articles included in this review. It was found that the use of a simple orthotic designed to minimize the vertical and shear forces during ambulation led to successful resolution of psoriatic foot lesions [14]. Specific features of orthoses that should be considered include a heel lift to address achilles tendinopathy/enthesopathy (a common feature of PsA), a strong medial arch support to stabilize the subtalar joint, a cushioned top layer, and a metatarsal bar to offer protection to the first MTP joint, and to minimize PsA-related pain [13,16]. While patients with psoriatic disease may develop a variety of tendinopathies/enthesopathies of the foot and ankle, evidence is currently limited on specific interventions for each [19]. Additionally, it has been suggested that pedal edema, joint swelling, and toe involvement such as dactylitis, which are common to inflammatory conditions such as psoriasis and PsA, must be accommodated with sufficient shoe size [13]. However, this should be considered on balance with the notion that excess space in the shoe may subject the patient to the effects of excess friction, if plantar psoriasis is also of concern [17]. Proposed solutions include construction of a soft toe cap and carefully-placed stitching to minimize the effects of friction, according to some authors [13]. With early implementation of foot orthoses, it is thought that patients display improved outcomes such as reduced foot pain, and prevention of deformity, disability, and functional limitation [15].
The body of evidence examining the impact of footwear on psoriasis and PsA remains small, and generally of low study quality, representing an inherent limitation of our systematic review. Furthermore, because the available studies vary greatly in design, intervention and outcome, qualitative analysis and interpretation was necessary. Still, much remains speculative regarding the potential role of footwear in psoriasis and PsA.
This systematic review found a lack of strong evidence to support or refute the use of footwear as an adjunct in management of psoriasis and PsA. Based on qualitative synthesis and theory proposed from the articles included in this review, it seems reasonable that footwear intervention design for psoriasis and PsA should consider causes of discomfort in psoriasis and PsA. These include friction and associated Koebner phenomenon-mediated injury reduction, force redistribution to prevent deformity, appropriate accommodation for pedal edema, minimizing skin irritation, and concurrent management of associated pathologies. Given that footwear has not classically been discussed as a component of psoriasis and PsA management, it is hoped that this systematic review serves as an initial clinical resource for those involved in the care of patients with psoriasis or PsA. While many unknowns remain, it is hoped that the knowledge gaps identified in this review serve as a platform for further research in this area.
The authors have no disclosures. No funding was received for this study.