Melanoma is a highly aggressive cancer that can be cutaneous (most common) or mucosal, affecting the skin or mucous membranes at any organ in the body. It can also be found in the eye (uveal). Breast melanoma is rare, and it can manifest in one of three forms: 1) Metastatic secondary to primary melanoma at another site, 2) Primary cutaneous melanoma arising at the breast skin, or 3) Primary non-cutaneous melanoma arising in the breast parenchyma itself. The latter is exceedingly rare and till date, almost only twenty-two cases have been reported in literature, including the case in the current study. Due to the rarity of this type of melanoma, it should be diagnosed in a stepwise approach after exclusion of any potential differential diagnosis. Immunohistochemistry (IHC) is a cornerstone. Management should be simply by breast and axillary surgery according to guidelines for breast cancer, and then to be followed, if proven indicated by multidisciplinary team, by adjuvant therapy according to guidelines for melanoma. The use of radiotherapy is still under debate. Based on the rarity of this type of disease, prognosis is generally poor with overall survival less than 50%. We hereby present a case of 43-y-o lady with a final diagnosis of Primary Melanoma of Breast Parenchyma (PMBP), without skin involvement and without another-site primary, in our practice at Kuwait Cancer Control Centre (KCCC), State of Kuwait, Arabian Gulf area. Management was by surgery followed by immunotherapy. The patient approved for publishing via an informed consent.
Breast, Melanoma, Primary, Parenchyma, Rare, Kuwait
PMMB: Primary Malignant Melanoma of the Breast; PMBP: Primary Melanoma of Breast Parenchyma; IHC: Immunohistochemistry; SLNB: Sentinel Lymph Node Biopsy; ALND: Axillary Lymph node Dissection; KCCC: Kuwait Cancer Control Center; LIQ: Lower Inner Quadrant (Breast); MDT: Multi-Disciplinary Team
Malignant melanoma usually affects skin, mucous membranes and the choroid of the eye [1]. Breast melanoma can occur as a secondary lesion (metastatic melanoma from another primary site) or as a primary lesion arising originally in the breast. Of note, melanoma is the most common cause of metastasis to the breast from extramammary solid neoplasms [2].
Primary Malignant Melanoma of the Breast (PMMB) is particularly rare (3-5% of all melanomas and < 0.5% of all malignant breast tumors). It can present as either (1) Cutaneous melanoma involving the skin overlying the breast, or (2) Parenchymal melanoma with no skin involvement. The latter is also known in literature as Primary Melanoma of Breast Parenchyma (PMBP). The necessary tools for diagnosis include triple assessment: clinical; radiological and pathological, added to Immunohistochemistry (IHC) staining and tissue origin workup. The standard of care entails surgical removal, either by mastectomy or wide local excision, plus axillary Sentinel Lymph Node Biopsy (SLNB) +/- Axillary Lymph Node Dissection (ALND) if needed. Adjuvant therapy, if indicated, should follow the guidelines of melanoma management. The current study is to present a 43-y-o lady with a final diagnosis of PMBP, with no skin involvement or identified other-site melanoma, in our practice at Kuwait Cancer Control Centre (KCCC), State of Kuwait, Arabian Gulf area. The patient approved for publishing via an informed consent.
A 43-y-o female patient presented to surgical OPD in KCCC with a suspicious large left breast mass, no previous history of surgery or chronic medical illness. She has a positive family history of breast cancer related to her grandmother on the paternal side. Initial evaluation revealed a left breast mass, lower inner quadrant, with a size of 6 * 8 cm on clinical examination. Initial core biopsy result was “poorly differentiated malignant tumour: Metaplastic carcinoma vs. sarcoma vs. malignant phyllodes tumour”. Staging workup (CT scan, PET Naf and PET/CT scan) was free of metastasis. Surgical intervention was planned, and she underwent left mastectomy plus Sentinel Lymph Node Biopsy (SLNB), which came negative by frozen examination, on 30/1/2023. Final postoperative histopathology revealed (1) High grade malignant neoplasm compatible with malignant melanoma, (2) Tumour size of 6 * 6 * 5.5 cm, (3) Free margins; (4) Normal overlying skin (5) No evidence of Ductal Carcinoma in Situ (DCIS) or lymphovascular invasion and all immunohistochemistry (IHC) stains were negative. The case was discussed in KCCC Breast MDT meeting, and the consensus was “for referral to Melanoma Unit for further management and immunotherapy”. The patient is currently following the prescribed treatment protocol (Figure 1, Figure 2 and Figure 3).
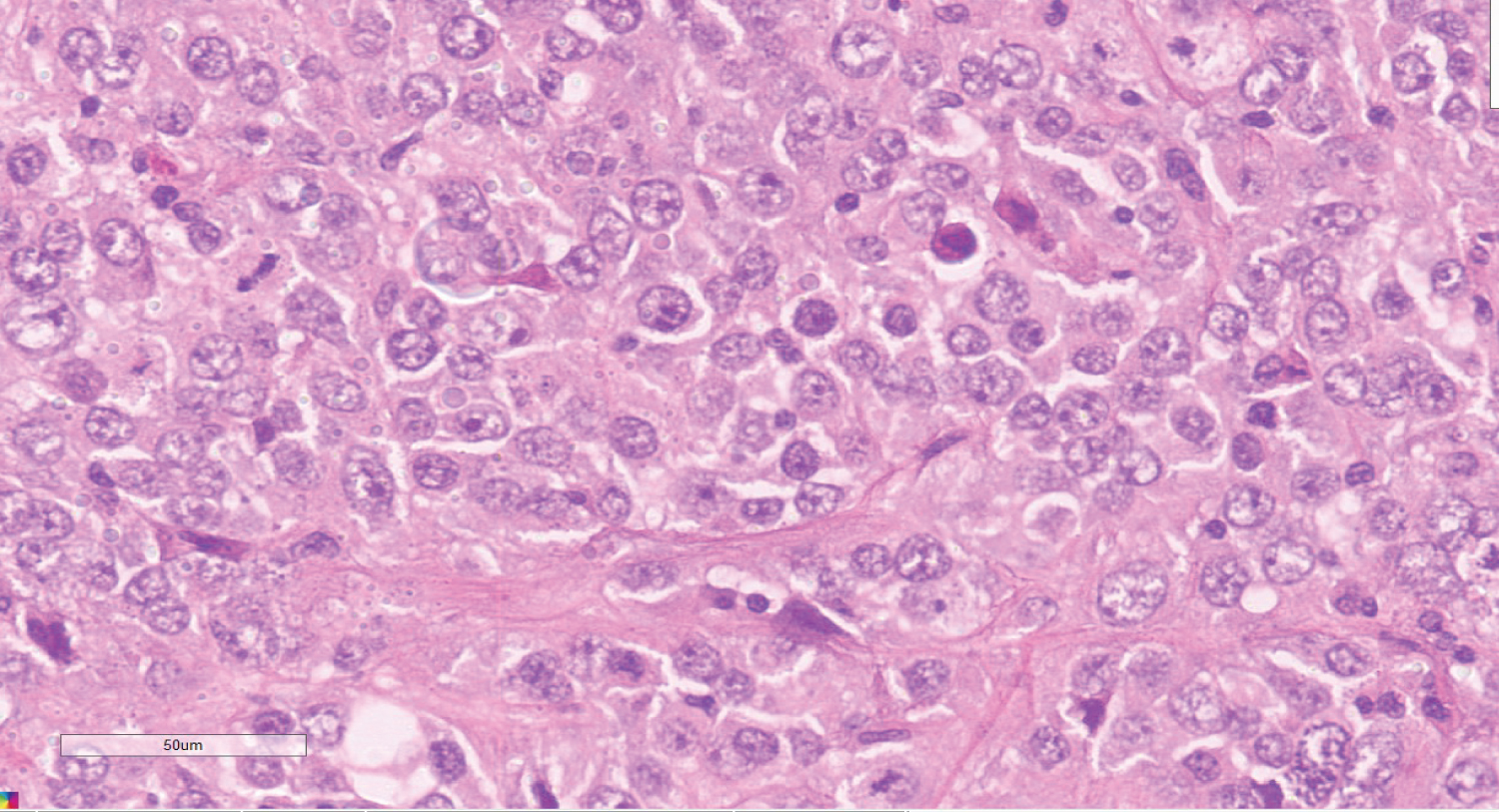 Figure 1: Hematoxylin and Eosin section shows large tumor cells with pleomorphic vesicular nuclei and prominent nucleoli.
View Figure 1
Figure 1: Hematoxylin and Eosin section shows large tumor cells with pleomorphic vesicular nuclei and prominent nucleoli.
View Figure 1
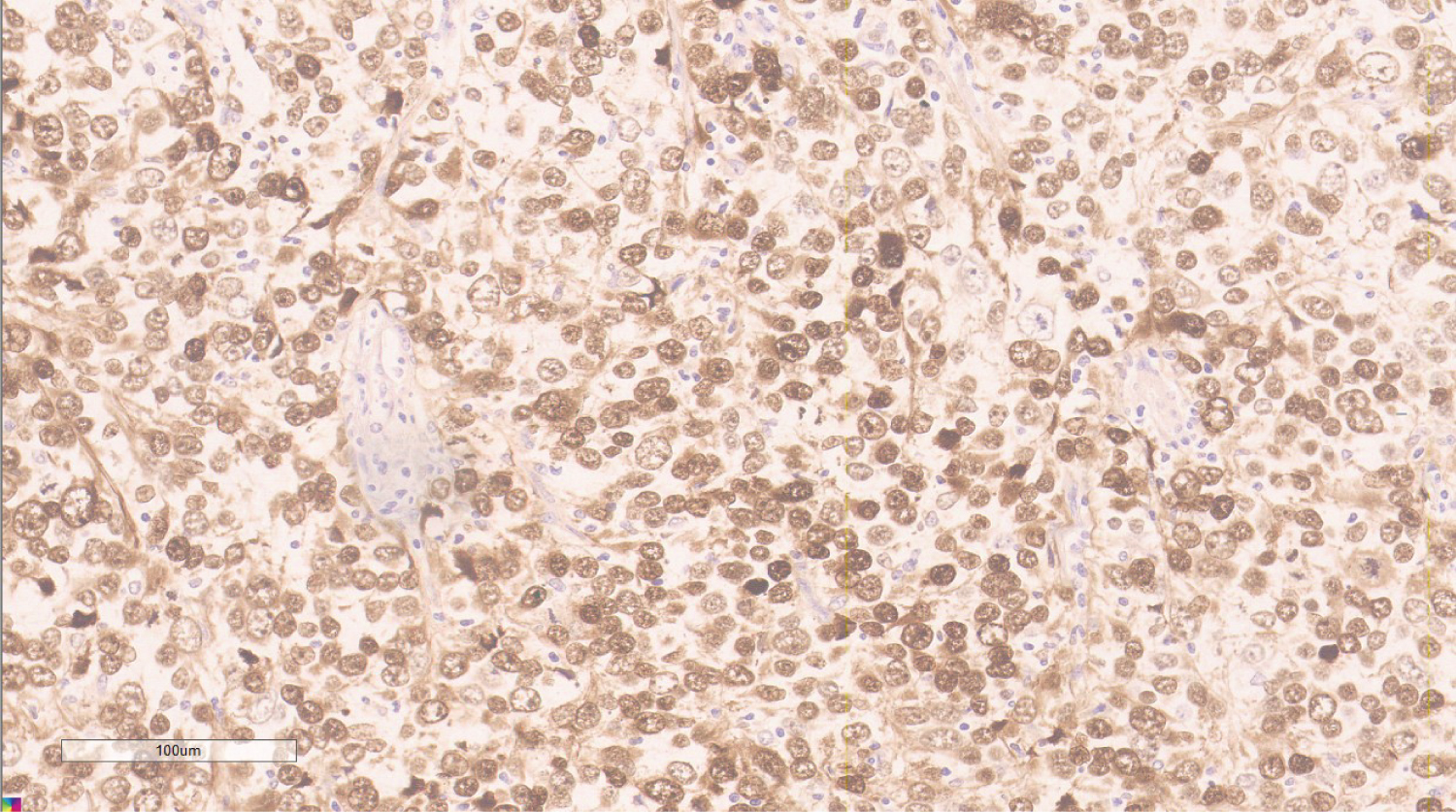 Figure 2: S-100, showing nuclear expression in tumor cells.
View Figure 2
Figure 2: S-100, showing nuclear expression in tumor cells.
View Figure 2
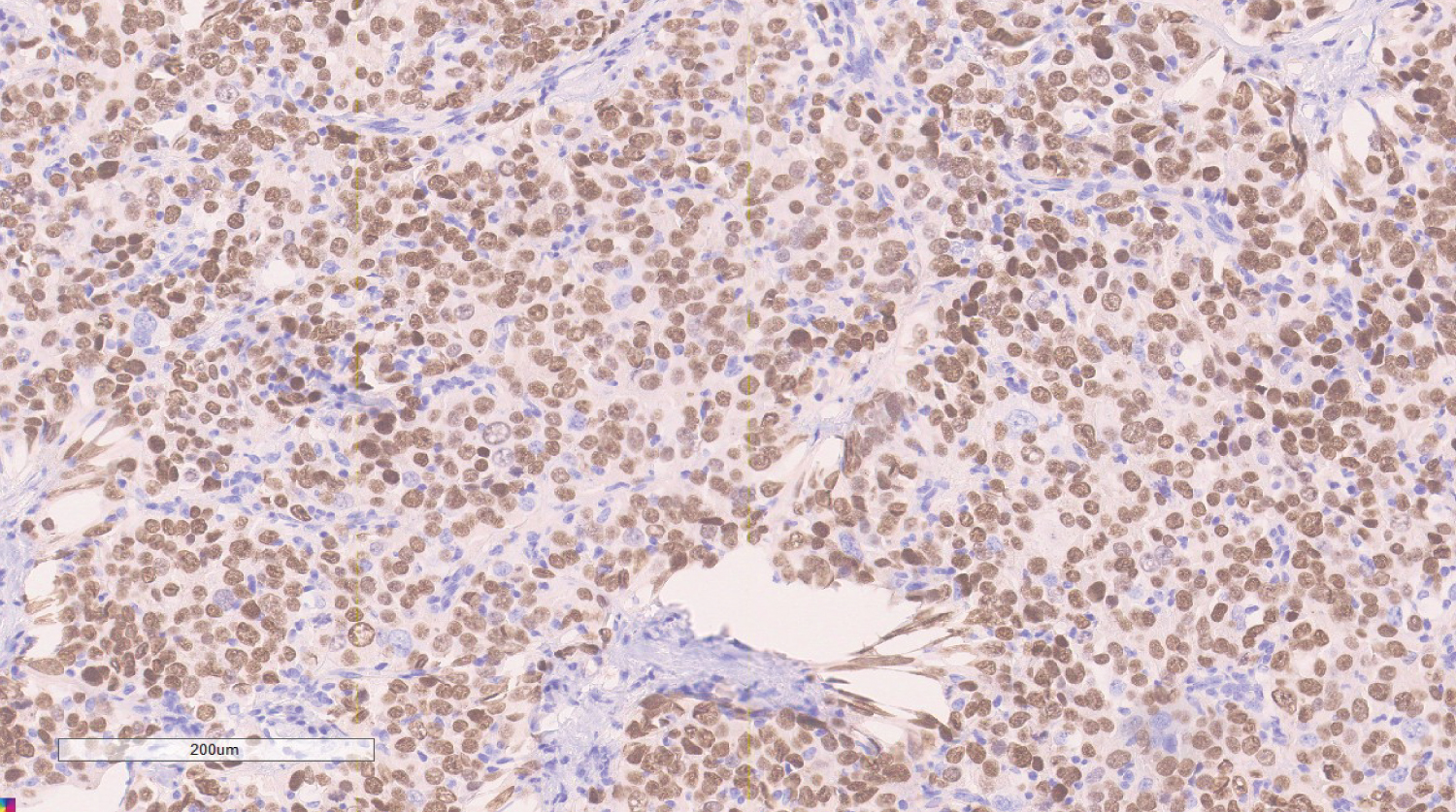 Figure 3: SOX-10, showing nuclear positivity in tumor cells.
View Figure 3
Figure 3: SOX-10, showing nuclear positivity in tumor cells.
View Figure 3
Melanoma is a highly aggressive neoplasm of atypical melanocytes, with unpredictable biological behavior. Typically, melanoma arises from the skin, and about 4-5% of primary lesions are extracutaneous [3]. It can be found in paranasal sinuses, anus and other mucosal linings (mucosal melanoma) as well as in the eye (uveal melanomas of the choroid, iris and ciliary body). The breast can be a site of both primary malignant melanoma, arising from outside (the overlying skin) or the inside (breast parenchyma), and metastatic lesions from other primary skin locations [4]. “Breast melanoma” is a term that can include three main clinical presentations: melanoma of the skin overlying the breast (most common), metastatic breast melanoma lesion, and primary melanoma of breast parenchyma [5].
PMBP is extremely rare, and most literature about breast melanomas is focused on those either arising on the breast skin or metastasizing from other primary sites [6]. The first case of non-cutaneous PMBP, presenting as a breast mass, was described by Gatch in 1956, and since then till 2020, only 14 non-cutaneous cases have been reported in the literature according to Mastoraki, et al. [3]. In addition, the authors in the current study found only four more cases of PMBP and another two cases of primary melanoma of the breast nipple [5,7-10].
In a study of non-cutaneous melanomas, 6,691 melanoma cases were reported, of which 4,885 were ocular and 1,806 mucosal, with no cases of noncutaneous PMMB [11].
While the characterization of PMBP has been limited to a few literature reports, Rassouli and colleagues explained that it might arise from ectopic melanocytes incorporated in the breast epithelium, or as the result of metaplastic changes in breast duct cells. In their literature review, only two of the evaluated cases had axillary lymph node metastases, which could be interpreted as a distinctive metastatic pattern of PMMB.
Given the rarity of PMMB, and more particularly PMBP, the definitive clinicopathological characteristics are not established yet and so it is usually difficult to diagnose. The most common clinical presentation is a palpable breast lump. A previous study from Italy included 39 cases of PMMB and noted a pattern of distribution different from the usual for breast cancer with a predominance of the upper inner quadrant [12]. In a recent case report from Korea, the patient presented with a recurrent breast abscess [6]. Our case presented with a palpable lump in the lower inner quadrant (LIQ) of left breast (Figure 4, Figure 5 and Table 1).
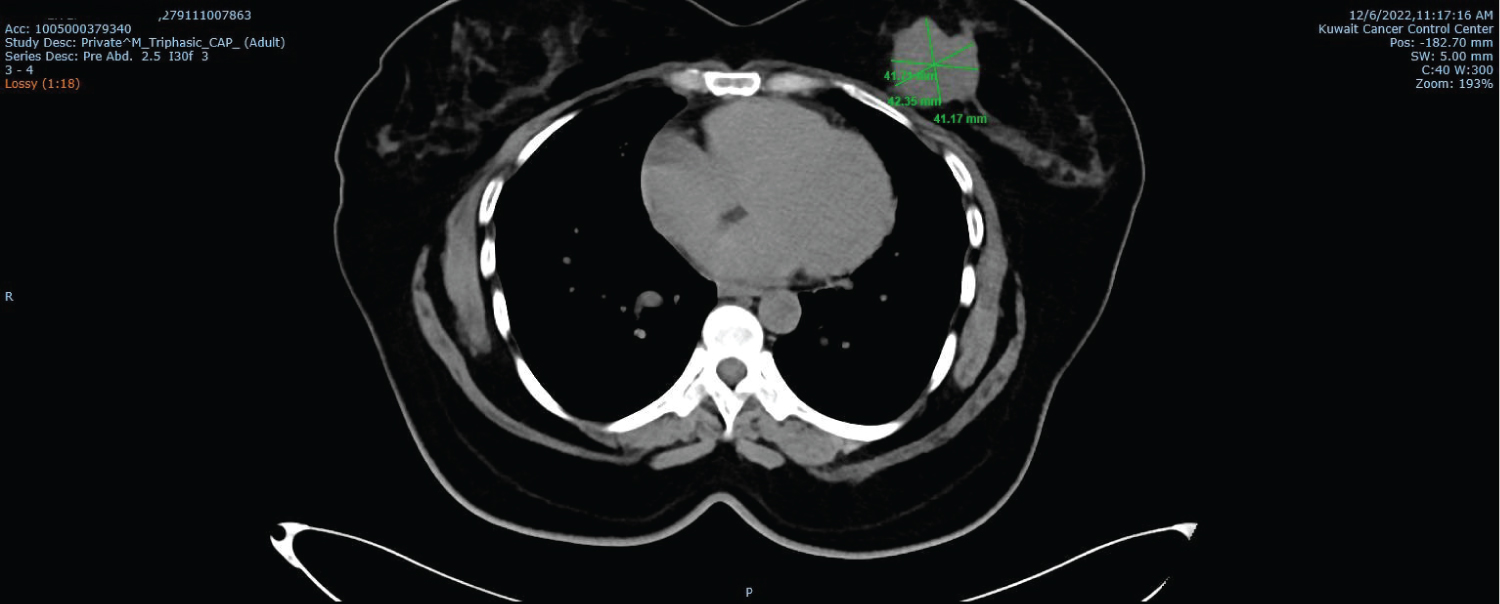 Figure 4: Triphasic CT scan (for metastatic workup) showing the mass in LIQ of left breast.
View Figure 4
Figure 4: Triphasic CT scan (for metastatic workup) showing the mass in LIQ of left breast.
View Figure 4
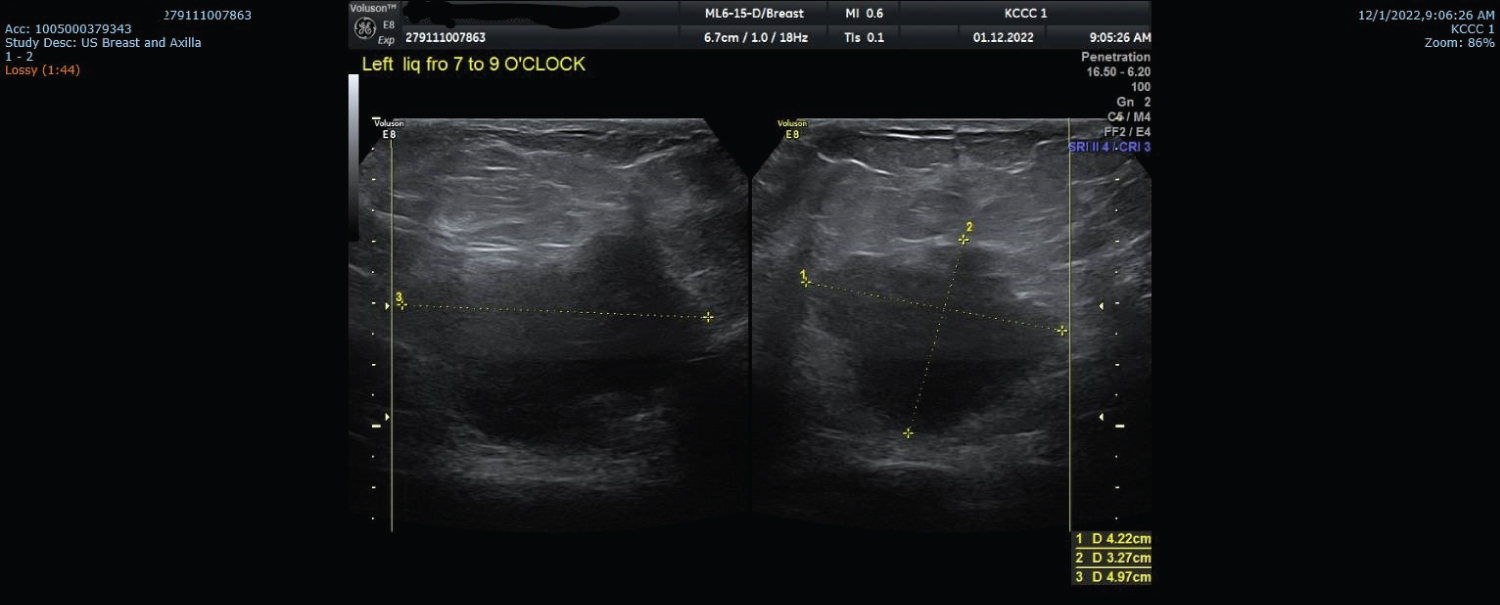 Figure 5: Ultrasound examination showing the mass in LIQ of left breast; 7-9 o'clock position.
View Figure 5
Figure 5: Ultrasound examination showing the mass in LIQ of left breast; 7-9 o'clock position.
View Figure 5
Table 1: A simple guide of workup to reach final diagnosis of different types of breast melanoma (from Mastoraki, et al. [3]). View Table 1
The first step is to rule out poorly differentiated invasive breast carcinoma. Another important step is to differentiate metastatic melanoma to the breast from other primaries in skin. A thorough complete skin examination should be performed to exclude the presence of a primary [13]. Paget’s disease of the breast (nipple and areola complex) may look like cutaneous melanoma and needs to be differentiated from it as treatment approaches are not the same. Dermal infiltration of an underlying ductal breast carcinoma in the area of the areola without pagetoid epidermal invasion may resemble malignant melanoma clinically. Usually diagnosis is made by history, clinical examination, histology and IHC. Differential diagnosis also includes metaplastic carcinoma of the breast with melanocytic differentiation and epithelioid angiosarcoma of the breast [9]. Sarcomatoid carcinoma and sarcoma with epithelioid features, like clear cell sarcoma and histiocytic sarcoma, can also be added to the differential diagnosis. Clear cell sarcoma is well known for its characteristic histological features, almost identical to melanoma, and some studies have suggested that the presence of BRAF mutation, which favours the diagnosis of melanoma, is a key-point to distinguish between both entities [14].
On histological examination, melanoma cells have a diverse appearance ranging from epitheloid-like to spindle-shaped cells and include different cytoplasmatic features, such as signet ring shapes and clear cells. In addition, their growth patterns result in a large architectural variation with trabeculae, papillary figures, glands and rosettes.
Due to this variability, IHC is required to distinguish melanomas from epithelial, hematological, mesenchymal and neural tumors and from metastases of extramammarian malignancies, such as melanomas and carcinomas of the lung, ovary, prostate, kidney and stomach. S100 is the most sensitive marker for melanoma with a sensitivity of 97-100% [2]. Other established sensitive and specific markers for melanoma are melan-A, tyrosinase and HMB-45. Usually, an additional panel of epithelial, mesenchymal, lymphoma- and sarcoma-specific markers is assessed to exclude metastatic disease. Finally, Ki-67 or Mib-1 staining may be used to distinguish between benign and malignant tumors [9]. In our case, the tumor was found negative for all IHC stains for epithelial, lymphoid; histiocytic, vascular or muscle origin. It showed positive immunoreactivity for S-100, SOX-10 and vimentin but negative for HMB45 and Melan A. Carcinoma was ruled out (due to negative epithelial stains) and so clear cell sarcoma (due to presence of significant pleomorphism).
Molecular testing (for BRAF mutation) and FISH (for EWSR1 gene rearrangement) were done, and both came negative.
The standard of management is surgery. Radical resection with negative margins and axillary SLNB is the key-principle, even in those patients with clinically negative axilla. If SLNB is found positive by frozen examination, Axillary Lymph Node Dissection (ALND) is to be performed. Further treatment must be based on the general principles of management of melanoma as the supreme rarity of the disease outweighs any specific considerations [4]. Interferon alpha is considered as the standard immunotherapy for high-risk patients. Other choices for primary advanced and recurrent PMMB include ipilimumab and vemurafenib and systemic chemotherapy with dacarbazine, temozolomide, cisplatin and paclitaxel. Radiotherapy does not improve overall survival, therefore, remains debatable.
The available data in the literature suggest that PMMB has a poor prognosis with survival rates of < 50% [2].
PMMB is extremely rare with only < 200 cases reported in the history of English literature and most of them were involving the breast skin. To date, total number of recorded cases of PMBP without skin involvement is 22 including our presented case of a 43-y-o lady who presented with a sizeable left breast lump and treated by surgery (left mastectomy+ SLNB) followed by immunotherapy. Accurate diagnosis is a challenge to both the surgeon and the clinicopathologist and also cannot be achieved without proper stepwise approach and IHC. Breast and axillary surgery are the mainstay of treatment and adjuvant therapy follows the guidelines applicable to melanoma. Prognosis is generally poor with < 50% overall survival.
Informed consent obtained from the patient about treatment plan and publication. The involved team of care approved and participated in the study.
The authors declare they have no conflict of interests.
None.
None.
Conceptualization: Amal Yousif Saleh Abdullah, Mohamed Moneer Abulfotooh Alsayed; Investigation: Rana Abdulghani, Sana Tabish, Ghaidaa Naser Abdul Razak; Resources: Ashraf Ahmed Abdeltawab Ibrahim, Ghaidaa Naser AbdulRazak, Mohamed Moneer Abulfotooh Alsayed; Supervision: Amal Yousif Saleh Abdullah; Writing; primary draft: Mohamed Moneer Abulfotooh Alsayed; Writing, review and editing: Mohamed Moneer Abulfotooh Alsayed, Ashraf Ahmed Abdeltawab Ibrahim, Amal Yousif Saleh Abdullah.