Radiation exposure to the thyroid gland is unavoidable in breast cancer (BC) radiotherapy (RT). This study was conducted to evaluate the impact of using different supraclavicular (SCV) field angles on the percentage volume of the dose absorbed by the thyroid relative to the maximum dose absorbed by the spinal cord.
A total of 50 consecutive BC patients undergoing planning computed tomography (CT) were evaluated. The thyroid gland, spinal cord, and SCV nodal volumes were contoured on the planning CT of patients who received 50 Gy of radiation in 2 Gy daily fractions to either the breast or chest wall, and to the SCV or full ipsilateral regional nodes. Dosimetric comparisons of three different angles (0º, 10º, and 15º) of the anterior SCV field with a corner spinal cord shield was performed on three-dimensional conformal radiation therapy (3DCRT). We compared the percentage volumes of absorption by the thyroid at low (V15), intermediate (V30), and high (V50) doses (15 Gy, 30 Gy, and 50 Gy), respectively; it was also compared with the maximum dose absorbed by the spinal cord.
The mean thyroid volume of our population was 8.3 cc (1.8-20 cc). The mean percentage volumes of radiation absorbed by the thyroid were as follows: low dose (V15) = 26%, intermediate dose (V30) = 16.3%, and high dose (V50) = 2.8%. We found that smaller field angles were associated with lower mean percentages of volume absorption for radiation doses of all dose levels (low, intermediate, and high doses; this finding was statistically significant (P < 0.05). The mean maximum dose to the spinal cord is lower at larger angles (15º, 10º, and 0º; 9.6 Gy, 17.3 Gy, and 33.6 Gy, respectively), which was also statistically significant (P < 0.05); a maximum dose was observed at 0º for 47.9 Gy. We found that the mean contoured thyroid volume only influences the percentage volume absorbed by the thyroid at a high dose and smaller angle (≤ 10º); this finding was statistically significant (P < 0.05).
Use of a larger anterior SCV field angle to spare the spinal cord led to a significant increase in the percentage volume of radiation absorbed in the thyroid at all dose levels; this has the potential to increase the thyroid post-radiation toxicity.
We propose routine utilization of field angle (≤ 10º) and a medial spinal cord shield as an optimal strategy to minimize the doses absorbed by both the thyroid gland and spinal cord.
Thyroid, Breast radiation, Absorbed dose
Supraclavicular (SCV) nodal irradiation is recommended in the majority of node-positive breast cancer (BC) patients as part of adjuvant radiation therapy (RT) to the chest wall or breast. Radiation exposure to a part of the thyroid is unavoidable in BC patients receiving adjuvant radiotherapy that includes ipsilateral SCV nodal irradiation. Practices such as delineating the thyroid, spinal cord and utilizing three-dimensional conformal (3DC) RT planning in BC nodal irradiation are being increasingly performed, while practices such as utilizing conventional SCV or full-nodal irradiation fields are decreasing. Even though some dosimetric data on 3DCRT planning of SCV irradiation showed better target coverage, they also indicated that increased radiation doses were being absorbed by the thyroid [1].
Hypothyroidism was reported as the most common thyroid disease following RT to the neck in patients with Hodgkin's lymphoma and in those with head and neck tumors. In those patients, hypothyroidism can develop several months to years after RT. These studies revealed that about 30%-50% of all patients developed either clinical or subclinical hypothyroidism during the follow-up period [2-11]. Thyroid function was primarily assessed by measuring thyroid-stimulating hormone (TSH) levels. Some researchers found that female gender was associated with relatively higher rates of hypothyroidism following neck irradiation.
Several reports examined post-treatment hypothyroidism in BC [12-17]. For instance, Joensuu, et al. demonstrated that an immunoassay of 80 patients (21%) treated with post-mastectomy radiation showed evidence of hypothyroidism [12]. Further, in their retrospective study of 200 BC patients, Bruning, et al. found that the prevalence of hypothyroidism was significantly greater in patients who had received regional nodal irradiation compared to those who received radiation to the chest wall or breast alone [13]. The data indicated that patients who underwent 3DCRT exhibited a tendency toward increased post-treatment hypothyroidism, as compared with those treated with conventional radiation planning; moreover, hypothyroidism was significantly increased in female BC patients following combined modality treatments of chemotherapy and radiation [14].
The tolerance level of thyroid tissues to radiation is poorly defined but, theoretically, the development of radiation-induced hypothyroidism is primarily related to vascular damage and less viable tissue that is not able to produce thyroid hormone post radiation [15]. This largely depends on the volume of the thyroid gland receiving high radiation doses.
The risk of developing post-radiation hypothyroidism is not remarkably high (15%-18%) [14,18]. In the past two decades, BC patients showed dramatic improvements in their long-term survival; thus, it is of interest to explore the effect of radiation exposure on the thyroid glands of BC patients, and further studies are needed to evaluate the dose-effect relationship between RT and long-term thyroid toxicity following regional nodal irradiation.
The aim of our study was to evaluate the impact of different angles of SCV fields on the percentage volume of the radiation dose absorbed by the thyroid gland. Another aim was to document the maximum dose absorbed by the spinal cord to assess whether the use of different beam angulations would predict lower dose volumes of thyroid gland absorption, and to examine how that would affect the maximum dose absorbed by the spinal cord.
After we obtained ethical approval from the institutional review board at King Abdulla Medical City, we conducted this dosimetric study in the Radiation Oncology Department on a total of 50 consecutive BC patients treated with radiation during the year 2015. Patients received radiation doses of 50 Gy in 2 Gy daily fractions to either the breast or chest wall and regional nodes.
1. Adult female patients with pathologically proven invasive BC.
2. Patients treated surgically either by modified radical mastectomy (MRM) or breast conservation surgery (BCS).
3. Patients treated with adjuvant radiation with three fields of RT, but only when the target volume included the breast after BCS or the chest wall after MRM, as well as the ipsilateral regional lymph nodes.
1. Any patients with abnormal thyroid glands or abnormal thyroid nodules were excluded from this study.
2. Any patients where the RT plan required supplementary axillary RT Field were also excluded.
CT simulation was conducted while the patient was in the supine position, with both arms extended above the head and immobilized using a breast board. The CT scan was obtained using a wide bore CT scanner with the patient in the treatment position. A free-breathing planning scan was obtained covering the region from the lower cervical vertebra body to 2 cm below the diaphragm in 5 mm slide thicknesses.
1. The scan images were exported to the treatment planning system for target delineation and computer dosimetric planning.
2. The following volumes were included and routinely delineated on CT slides: The breast, chest wall, SCV, axilla, lungs, heart, and spinal cord. We contoured the thyroid gland for purpose of this study.
3. The total radiation dose delivered to the chest wall or breast was 50 Gy in 25 fractions (2 Gy/fraction) followed by ± additional tumor bed boost of 10 Gy/5 fractions using photons or 6-12 MeV electrons. The total prescribed radiation dose to the ipsilateral SCV was 50 Gy.
Treatment planning and dose calculation were performed using the Eclipse planning system (Version 10) applying the AAA algorithm. We compared the dosimetric impact on the thyroid gland by employing three different field angles using (3DCRT) planning to encompass the CT-contoured SCV nodal volume.
Data collection was performed for the following parameters based on each patient's Dose Volume Histogram (DVH):
1. The percentage and absolute volumes of the thyroid gland (cc) absorbing 15 Gy, 30 Gy, and 50 Gy (V15, V30, and V50), respectively; these were estimated at different beam angulations of 0º, 10º, and 15º.
2. The total and mean thyroid dose (cc).
3. Dosimetric comparisons between the three different angles (0º, 10º, and 15º) of the anterior SCV field with a corner spinal cord shield were performed on 3DCRT (Figure 1). We compared the percentage volumes of the thyroid absorbing low (V15), intermediate (V30), and high (V50) doses (15 Gy, 30 Gy, and 50 Gy), respectively, as well as the maximum dose absorbed by the spinal cord.
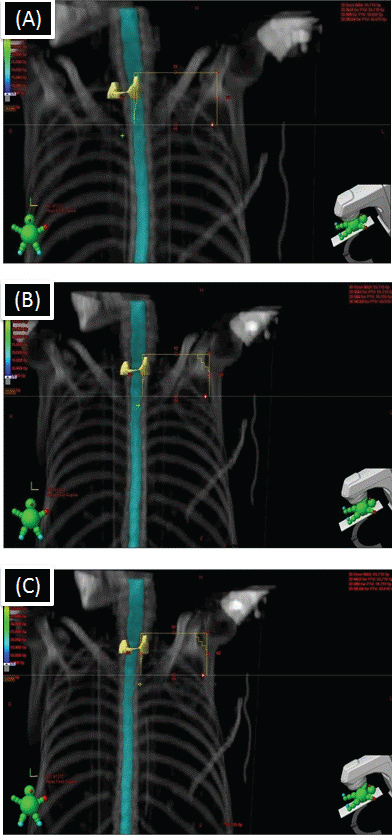 Figure 1: CT Planning shows the effect of different angles of anterior supraclavicular field and corner spinal cord shield at (A = 0º, B = 10º and C =15º) on inclusion of contoured thyroid volume. View Figure 1
Figure 1: CT Planning shows the effect of different angles of anterior supraclavicular field and corner spinal cord shield at (A = 0º, B = 10º and C =15º) on inclusion of contoured thyroid volume. View Figure 1
After cleaning and checking the accuracy of the data, we imported the data on SPSS program version (22.0.0.0) for statistical analysis. We provided descriptive statistics using percentages, mean and standard deviation (SD). For the comparison between the two groups, a two-tailed t-test was used. A P-value of (< 0.05) is considered statistically significant.
Of the 50 eligible BC patients, 10 underwent BCS and 40 underwent MRM. The patients' characteristics are summarized in (Table 1). The mean thyroid volume of our population was 8.3 cc (1.8-20 cc) (Table 1). The patients' mean age was 51.38 years (range: 28-75 years of age). The SCV nodes were treated in only 27 cases and full regional nodes were included in the remaining 23 cases.
Table 1: Population characteristics. View Table 1
The mean percentage volumes of thyroid absorption were as follows: low dose (V15) = 26.7%; intermediate dose (V30) = 16.9%; and high dose (V50) = 2.5%.
We found that smaller field angles were associated with lower mean percentage volumes for the thyroid absorption of radiation at all low, intermediate, and high doses (Table 2), which was statistically significant (P < 0.05). Conversely, the mean maximum dose absorbed by the spinal cord was lower with larger angles (15º, 10º, 0º angles; 9.6 Gy, 17.3 Gy, and 33.6 Gy respectively); the maximum dose absorbed by the spinal cord (47.9 Gy) was noted at 0º (Table 3). We also found that the mean thyroid volume had no effect on the dose absorbed by the thyroid, except for volume percentages of radiation absorbed by the thyroid at high doses and at smaller angles (≤ 10º), which was statistically significant (P < 0.05).
Table 2: The percentage volume of the thyroid gland absorbing low, intermediate and high dose radiation with anterior supraclavicular field and corner thyroid shielded at different feild angles. View Table 2
Table 3: The maximum absorbed dose (Gy) to the spinal cord with different angle of anterior supraclavicular field and corner thyroid shielded. View Table 3
Radiation therapy to supraclavicular nodal region in breast cancer patients will encompass unavoidably part of the thyroid gland within the irradiated volume. This is associated with several potential long-term side effects.
Primary hypothyroidism is the most common radiation induced thyroid disorder within 5 years after curative radiation to neck area (30%) [15]. In one retrospective study of about 200 patients which were diagnosed with breast cancer and received regional lymph nodal irradiation of 40-50 Gy, subclinical and clinical hypothyroidism were much higher in irradiated group when compared with the control group (P = 0.00001) [13].
Another detrimental effect of radiation to the thyroid gland is that develop thyroid tumors. Most thyroid tumors diagnosed after radiation are benign and about one-third are malignant [19]. Some reported, that risk of secondary thyroid malignancy is about 30-fold greater in irradiated population [20].
In the current study, we found that smaller anterior SCV angles were associated with lower percentage volumes of thyroid absorption for RT doses in BC patients planned with both 3DCRT and a medial spinal cord shield. Tunio, et al. found that small thyroid gland volumes and V30 > 50% (the absolute thyroid volume receiving 30 Gy) significantly increased the risk of radiation-induced hypothyroidism [18]. In a case-control study on hypothyroidism post-BC RT, Johansen, et al. found that small thyroid gland volumes were associated with greater risk of post-treatment hypothyroidism, while the volume of the thyroid gland receiving < 30 Gy of radiation in controls was almost 2.5 times greater than the cases [21].
In our study, we utilized 3DCRT for all cases with different field angulations for the SCV nodes; we found that the mean volume percentages of the thyroid absorbing an intermediate dose (V30) at 0º, 10º, and 15º angles were 11.1%, 16.9%, and 21.0%, respectively, while the maximum percentage volumes were 43.8%, 43.5%, and 50.5%. Conversely, the mean maximum dose absorbed by the spinal cord was lower with larger angles (15º, 10º, 0º corresponding to 9.6 Gy, 17.3 Gy, and 33.6 Gy, respectively).
These results indicate that smaller field angles are associated with lower mean and maximum volume percentages for the thyroid's absorption of certain radiation doses; this increase in the anterior SCV field angle significantly increases the percentage volume of the thyroid-absorbed dose at all dose levels, which potentially increases the long-term complications of thyroid irradiation, as well as the development of hypothyroidism and radiation-induced secondary malignancy.
Large field angle (15 degree) has the advantage of reducing the dose to the spinal cord but at the same time, it increases the dose to the thyroid gland, which carries a higher risk for developing hypothyroidism and secondary malignancy. On the other hand, zero angle has the advantage of decreased thyroid dose, but it increases the dose and toxicity to the spinal cord. Therefore, we found that the utilization of small anterior SCV field angles with a medial spinal cord shield is the optimal strategy to minimize the doses absorbed by both the thyroid gland and spinal cord.
We conclude that 3DCRT planning of SCV nodal irradiation with larger anterior field angles significantly increases the percentage volume of thyroid-absorbed radiation doses at all dose levels. Since thyroid gland contouring and 3DCRT are not routinely used in planning RT to SCV, we recommend the utilization of small anterior SCV field angles with a medial spinal cord shield as an optimal strategy to minimize the doses absorbed by both the thyroid gland and spinal cord.
English-language editing of this manuscript was provided by Journal Prep.
Our study was approved by Institutional Review Board of King Abdullah Medical city under registration at National BioMedical Ethics Committee, King Abdulaziz City for Science and Technology: (Registration no.H-02-K-001).
Due to retrospective and non-interventional nature of the study participant consent was waived.
The datasets of the current study are available from the corresponding author on request.
This study was not funded.
TN and MM participated in the study design and analysis as well as prepared the background research. MG and RZ provided treatment planning support and participated in data collection. TN wrote the draft manuscript. TN and MM reviewed and revised the draft and final manuscript. All authors read and approved the final manuscript.
Not applicable.
All authors declare that they have no competing interests.