Introduction: Dentoalveolar Trauma is a condition that requires immediate emergency management. The revision of its prevalence is the basis for the allocation of resources focused on its management, which differs between health centers. We present the prevalence of these injuries in patients treated in the Emergency Service of the Barros Luco Care Complex.
Materials and methods: Retrospective study was carried out by reviewing the Urgent Care Data of patients seen between January 2018 and June 2019. From each instrument, the patient's age, gender, diagnosis and affected tooth or supporting structures were taken.
Results: 280 records were incorporated, 123 women, 157 men. The second and third decades were the most present, with a male predominance, since the fourth decade there was a greater frequency in the female gender. Upper central incisors had the highest frequency of involvement (57.67%), followed by upper lateral incisors. The supporting tissues were more affected, being the diagnosis of Subluxation the most prevalent (27.6%), followed by uncomplicated coronary fracture (20%) and Concussion (9.7%).
Discussion: Similar results are presented to those reported in other hospital emergency care centers but dissimilar to other health centers specialized in secondary-level pediatric dentistry or university clinics, where there are mainly cases of greater complexity or that cannot be resolved in care primary. It is relevant to characterize the population cared for in each center as well as its most frequent pathology in order to direct resources in a focused manner.
Conclusions: The results are similar to those presented in other urgent care centers. The individual cost that an untreated or late-treated trauma can entail is high, being greater if the patient does not receive adequate initial management, complicating subsequent rehabilitative therapeutic actions.
Dentoalveolar trauma, Emergency service, Epidemiology
Dentoalveolar Trauma (TDI) groups a set of traumatic injuries that compromise dental integrity and associated supporting tissues as a result of a release of energy on them, being a medium or high energy blow causal [1]. Its clinical presentation is variable due to differences in the amount and direction of energy involved in the process, the age of the patient associated with its morphological development, associated morbid history, causal agent of the trauma and the context in which it occurs [2].
Part of the factors associated with the different incidence between tissues affected by trauma are anatomical conditions (more protruded dentition), increased risky physical activities, lack of coordination by sensory systems in development and non-use of road safety elements in case of injury vehicular accidents [3,4]. With the increase in the automobile fleet subject to a greater number of road accidents, an increase in the practice of contact sports and the rise in situations of street violence such as fights or fights, there has been an increase in TDI reports, a generalized situation at the worldwide [5].
Studies regularly describe the condition at all ages, giving higher prevalence in pediatric patients where it has been reported that up to 35% of children have a history of TDI, including primary and permanent dentition [6]. In relation to this, the International Association of Dental Trauma (IADT) estimates that 25% of school patients have experience of TDI in permanent teeth, as well as 33% of the adult population, presented at an age younger than 19 years [7,8].
Among dentitions, lateral dislocation has been reported to be the most common injury in the primary dentition while crown fractures with or without pulpal involvement have been reported mostly in the permanent dentition [9].
The Emergency Unit of the Barros Luco Assistance Complex (CABL) has a Dental Emergency service with an uninterrupted care system, with priority for adult patients (over 12 years of age) where TDI is usually received, but without real knowledge about the percentage of the attentions that are carried out for the resolution of these pictures. The study regarding the prevalence of injuries that may occur must be of general interest to officials who work in emergency care centers, in order to be able to objectify and focus the available resources. The objective of this study is to quantify the visits to the CABL Emergency Unit and to classify the type of TDI treated according to the anatomical structures involved.
A descriptive retrospective study was carried out by collecting the Emergency Care Data (DAU) of patients treated at the CABL Emergency Unit, information that was provided by the South Metropolitan Health Service through an Excel™ database, for the period between January 2018 and June 2019 (18 months). The inclusion criterion was all DAU with the following complete data: Age, gender, diagnosis and description of the TDI (compatible with the IADT classification criteria) and affected tooth or supporting structures.
All records of patients whose UAD were not complete, patients under 12 years of age (population not targeted by the CABL) and follow-up care after the initial management of TDI were excluded.
The information was ordered and analyzed by the researchers in Microsoft Excel™, the final analysis included any record that presented a full description of the clinical case, excluding all records whose variables were incomplete. Consultations were recorded as a total number (n) and the percentage (%) and ratio were used as point estimators.
During the 18-month period, 372 patients with diagnoses associated with TDI were admitted, of these 92 records were excluded as a result of incomplete information or being under the age range of 12 years, whose attention was referred to the Pediatric Emergency Service of the Exequiel Hospital Gonzalez Cortes, leaving a total of 280 records.
In relation to gender, males presented a higher frequency of TDI, with 157 patients admitted versus 123 females, a general ratio of 1:1.3. The age range with the highest frequency of affection was between the second and third decade. In the cases reported from the fifth decade, there was a higher frequency of TDI in the female gender. The breakdown of the data is presented in Table 1.
Table 1: Distribution of ADD by age and gender. View Table 1
In relation to the affected teeth, a total of 300 were observed, being the upper central incisors the ones that presented the highest frequency with 57.67% of the cases, followed by the upper lateral incisors with 22.67%. The anterosuperior dentoalveolar group presented greater affection in the cases of TDI included, observing a relationship between maxillary and mandibular teeth of 7.3:1. The breakdown is presented in Figure 1.
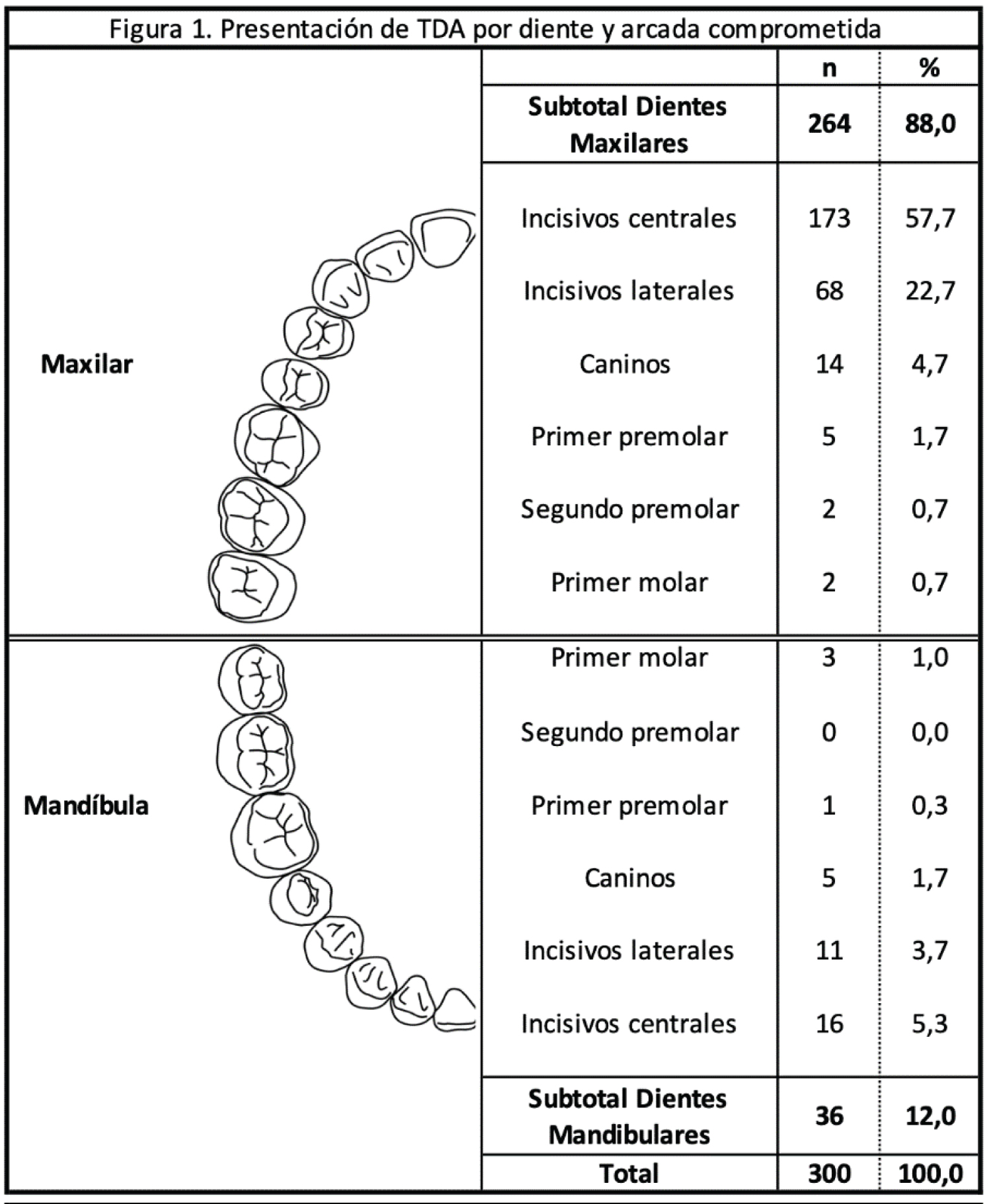 Figure 1: Presentation of TDI due to compromised tooth and arch.
View Figure 1
Figure 1: Presentation of TDI due to compromised tooth and arch.
View Figure 1
In relation to the classification of TDI according to the IADT, there were 370 injuries, being related to the most frequent supporting tissues compared to dental and/or bone hard tissues, in a ratio of 1.15:1. It should be noted that the total number of reported injuries is greater than the number of affected teeth and patients, as a result of which more than one type of TDI may occur per patient and per affected tooth, with a frequency close to 1.
Among the involvement of the supporting tissues, the diagnosis of subluxation presented the highest prevalence (27.6%) followed by the diagnosis of concussion (9.7%), while in the hard tissues, the uncomplicated coronary fracture presented the highest prevalence (20%) followed by complicated crown fracture (9.2%) and crown root fracture (8.4%), respectively. The breakdown is presented in Table 3.
Table 2: Tissues affected in TDI according to IADT classification. View Table 2
Regarding the results, between genders, a higher prevalence was observed in males over females in a 1.3:1 ratio in the first three decades, results similar to reports presented in the region and at the national level [10]. Moving on to the fifth decade, it was possible to show that the female gender has a 1.7:1 ratio compared to the male gender, results similar to those presented by Rezende, et al. [11], where there was a 2:1 female to male TDI ratio. Answers to this have been found, justifying the greater inclusion of women in actions that were previously considered male-oriented, such as contact sports, physical work and high-impact work. A situation that is expected to be maintained and strengthened over time [11].
Regarding the distribution of affected teeth, the upper anterior group presented the highest frequency of TDI, specifically in central (57%) and lateral (22.67%) incisors, results that are similar to those expressed by national and international authors [5,10,12,13]. This relationship is explained due to the greater exposure of this group to direct trauma by objects or falls, accentuating the severity of the damage in patients with class II dentofacial anomalies given the greater protrusion and therefore exposure of these teeth [14].
Risk factors have been described that regularly facilitate an TDI in the event of an event: Class II modification I malocclusion together with a type II skeletal relationship which project the upper anterior dental group to a position of greater risk with an increased overjet; underlying diseases such as epilepsy or physical disabilities that are associated with an increased risk of falls [5]; consumption of substances that alter the perception of the environment or that lead to aggressive situations (drugs, alcohol); and human behavior itself, such as sports activities, situations of bullying or hyperactivity [5,15-17].
Postural instability, cardiovascular, visual or motor disability must be considered when receiving adults and older people who consult due to a TDI, since in the older population the probability of presenting a risk of falls is increased compared to the rest of the population [18]. These last two factors are associated with greater frequency in the adult population such as the one received in the Health Service presented in this situation. When reviewing the classification of TDI according to IADT, there was a higher frequency of injuries in supporting tissues, with subluxation being the most frequent. The diagnosis of uncomplicated coronary fracture was the most prevalent in hard tissue injuries, being the second most prevalent injury among the total. These results are similar to those reported in other hospital emergency care centers such as Velasquez, et al. and Brezzo and Dreyer [10,19]. Situation dissimilar to that reported by Veliz, et al. and Diaz, et al. and Lemos, et al. [12,13,20] where complicated coronary fractures, root fractures and extrusive dislocations are presented within the main prevalence. This difference can be attributed to the type of health center analyzed, since in the last group a population was taken that was treated in secondary health centers, focused on the treatment of the pathology by specialists, where there are mainly derived cases or those that do not they can be resolved in primary care [10,12,13,19,20], Breakdown of these data in Table 3.
Table 3: Tissues affected in TDI between populations. View Table 3
To remember, in Chile the emergency management of TDI is stipulated within the Clinical Guide for the management of Dental Emergencies belonging to the Explicit Health Guarantees (GES), and covered by Law No. 19,966 Decree No. 44, for users linked to the National Fund of Health (FONASA) and Social Security Institutions (ISAPRES) [21].
The high individual and social cost that an untreated or late-treated TDI can entail is high, and this is greater if the patient does not receive adequate initial management of the emergency, which complicates subsequent rehabilitative therapeutic actions [16,17,22,23]. The GES program in the treatment of TDI has delivered great benefits to the patient, but it does not include management after the resolution of the emergency, dropping the entire cost of the rehabilitation treatment on the patient, a situation to work and avoid in the future through the establishment of comprehensive policies for treatment and follow-up after an TDI with the users of the health system.
The main traumatic injuries are concentrated between the second and third decade of life in both men and women, with the majority of the supporting tissues being compromised (53.5%) and leaving hard tissue in second place (46.5%). As in the rest of the literature, the anterosuperior dentoalveolar group is the most compromised, covering 85.1% of all injuries. The results are similar to those presented in the literature compared to other emergency care centers for the adult population.
The omission of data in the DAU when registering the patient's clinical history did not allow a full and unbiased analysis of other important variables such as the place of occurrence of the TDI, causal reason, means of admission, compromise of the patient's general condition and interventions performed for management in an emergency setting. This limitation is not uncommon among research groups, which is why it is necessary to work locally as teams on how to record a complete clinical history that can be the basis for more complex analyses, in order to guide work measures towards the improvement of patient care.