Lipomas are the most common benign soft-tissue tumour arising from mature adipose tissue "composed of mature adipocytes", mainly from subcutaneous tissues and usually surrounded by a thin fibrous capsule.
Still, the underlying cause of lipomas remains unclear. In literature, different theories described the pathogenesis of adipose tissue tumours, and also different histological variants have mentioned. It can occur anywhere in the body, its incidence being 0.1-5% of all head and neck tumours. Different types of lipoma may present based on the constituent tissue type and its location. Lipomas present, clinically, as well-circumscribed, slow-growing, painless masses, usually treated by complete excision. Some literature ranges the average of cheek lipomas from 1.5 to 2.5 cm, with a maximum size of 5 cm. Most of them seldom cause pain, subsequent in the delay to look for treatment.
This case aims to present a 65-years-old Malay female patient present with a giant cheek lipoma (10 × 10 cm), increasing in size over 20 years, compromising facial esthetics and treated surgically through an intra-oral excision, with uneventful postoperative period. This case report concludes that the main advantage of the intra-oral approach is an excellent aesthetic outcome as it is guaranteed no external scarring. Intra-oral approach lipoma excision is a relatively simple technique that should be taken into account when considering the surgical removal of cheek lipomas to reduce the probability of injury to the facial nerve as well.
Lipoma, Intra oral lipoma, Giant cheek lipoma, Lipoma excision, Intra oral approach, Soft tissue tumour
Lipomas are common benign soft-tissue neoplasms composed of mature adipose cells that represent the most common benign mesenchymal tumours admixed with collagen streaks and is often well-demarcated from surrounding connective tissue. A thin, fibrous capsule may be noticed, and a distinct lobular pattern can be present. It can found in all sites containing fatty tissue. Lipomas stand out from usual body fat because their lipids are not subject to metabolism "metabolically inactive in terms of catabolism during starvation, unlike normal adipose tissue which breaks down during starvation that normal body fat undergoes" besides, they undergo uncontrolled proliferation [1]. Commonly lipomas occur in the chest and extremities, but head and neck are less frequent, representing approximately 13-20% of cases and a majority of head and neck lesions located in the posterior portion of the neck and rarely develop in the anterior neck, face, and other regions [2].
The peak age of incidence is usually in the 5 or 6 decades of life while the occurrence in children is very uncommon. Usually, the size of the lesion is ˃ 3 cm at the time of diagnosis but can reach 5-6 cm over the years [3]. Majority of lipomas grow in the subcutaneous tissues, but deeper tissues may be involved as well; the oral cavity is not frequently affected. The first description of an oral lipoma was provided by Roux in 1848, who referred to it as a "yellow epulis". Hormonal factor, trauma and chronic irritation considered to play a role in the development of lipoma. However, trauma is widely accepted as a causative factor in the discovery of the lesion rather than the aetiology [4]. The overall incidence in the oral cavity is between (1%-4%) [5] of all benign oral lesions with female predominance, as shown in some studies. Although intra-oral lipoma is benign, some are continued to grow and may cause interference with speech and mastication due to the size of the tumour. The most common site of lipoma involvement is the cheek (32%) "Because it is an area of fat accumulation" followed by the tongue (20%), the floor of the mouth (15%), buccal sulcus and vestibule (12%), and other locations (21%) [3].
Generally, intra-oral lipomas are soft, slow-growing, mobile, and painless lesions that have been reported in the buccal mucosa, tongue, floor of the mouth, and lips. Usually, the patients are asymptomatic (except in cases where there is compression or obstruction). The usual presentation is in a subcutaneous location with distinct separation from the surrounding tissues, which can be appreciated by the relatively easy detachment from surrounding tissues during excision Surgical excision is the preferred treatment and is rarely associated with recurrences [6].
Ms M. is a 65-years-old Malay female present with left giant cheek swelling. The condition started 20 years ago when the patient developed left cheek swelling and gradually increased in size all over the prior period. Through the course of swelling no associated signs and symptoms "pain, fever, inflammation, discharge, change of colour, drooling of saliva, change in speech and change of facial expression".
Huge left facial side swelling about 10 × 10 cm extending from left cheek to left submandibular region. Swelling smooth surface, firm in consistency, non-tender, average in temperature, no skin changes, no intra-oral ulceration, no dilated veins over the swelling and all lymph nodes are intact. Local examination of facial expression and the facial sensation was normal. Patient denies change in salivation or dryness of the mouth.
- Fine Needle Aspiration performed: Result was a lipoma.
- CT scan impression: Benign soft tumour at the left side of the face, most probably benign "Differential is lipoma".
- MRI impression: Correlating with CT findings, features are suggestive of left face subcutaneous tissue lipoma.
Intra-oral small vertical incision made over the left buccal mucosa, dissection performed till lipoma capsule. Lipoma squeezed from outside and delivered intra-orally. It was well defined capsulated and looked lobulated lipoma; however, specimen sent for histopathology. Drain placed intra-orally and incision closed by catgut 5/0 (Figure 1, Figure 2 and Figure 3).
 Figure 1: Antero-posterior/lateral view of the giant left cheek lipoma.
View Figure 1
Figure 1: Antero-posterior/lateral view of the giant left cheek lipoma.
View Figure 1
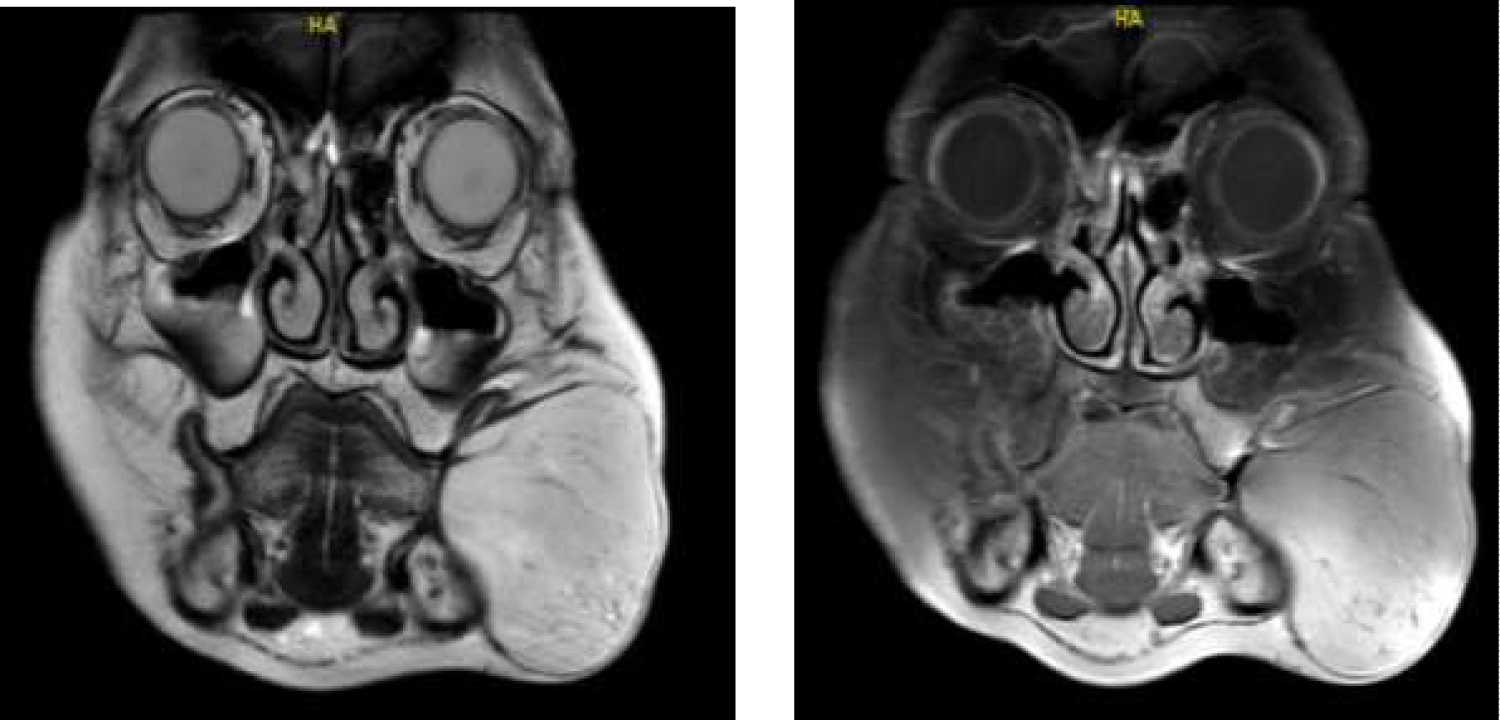 Figure 2: Coronal MRI view of the giant left cheek lipoma.
View Figure 2
Figure 2: Coronal MRI view of the giant left cheek lipoma.
View Figure 2
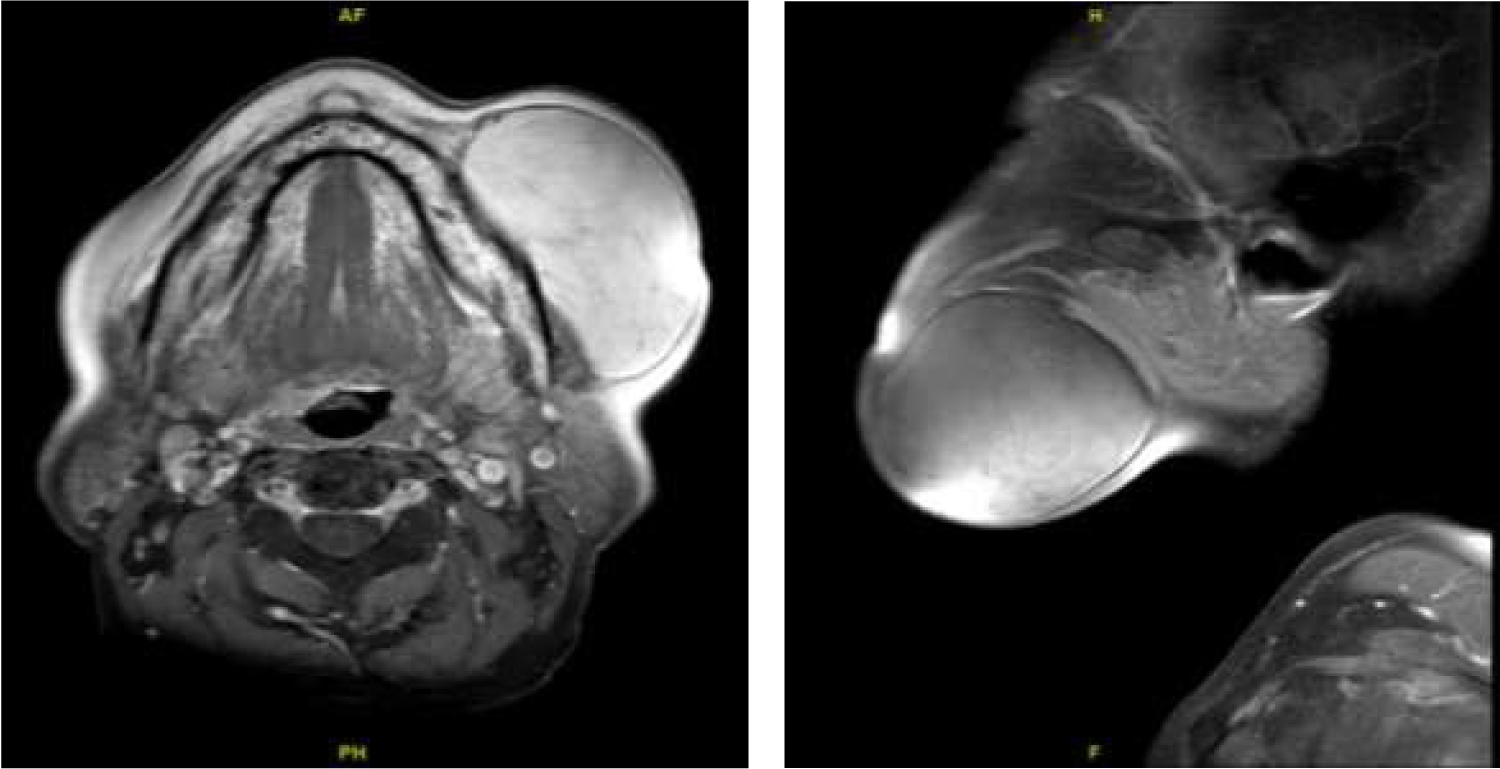 Figure 3: Axial and Sagittal MRI view of the giant left cheek lipoma.
View Figure 3
Figure 3: Axial and Sagittal MRI view of the giant left cheek lipoma.
View Figure 3
After three months of the follow-up period, skin over the submandibular and cheek region is soft with no underlying nodularity. There is a slight skin redundancy, but almost redundant skin regress in about 90% within three months. Intra-orally there is just fine linear well-healed scar, which does not cause any discomfort to the patient as well as the patient is fully satisfied with this approach and its outcome (Figure 4A, Figure 4B and Figure 5).
 Figure 4: A) Post-operative result with 3 months.
View Figure 4A
Figure 4: A) Post-operative result with 3 months.
View Figure 4A
 Figure 4: B) Post-operative result with 3 months (closer view).
View Figure 4B
Figure 4: B) Post-operative result with 3 months (closer view).
View Figure 4B
 Figure 5: Post-operative left small fine intra-oral scar.
View Figure 5
Figure 5: Post-operative left small fine intra-oral scar.
View Figure 5
Lipomas are the most common soft tissue mesenchymal tumours. Lipomas develop mostly in the subcutaneous tissues and only rarely in deep tissues. The most commonly involves site the trunk, limbs and with 15% to 20% of involving the head and neck region, and seldom the oral as only 1% to 4% of lipomas in the maxillofacial region [7]. Furlong, et al. found only 125 cases of oral lipomas over 20 years, which again shows the rarity of intra-oral lipomas [8]. The occurrence is higher in females than in males. Lipomas usually develop in patients over 40-years-old [3]. Possible theories regarding the aetiology of lipomas include heredity, fatty degeneration, hormonal basis, trauma, infection, infarction, metaphase of muscle cells, lipo-blastic embryonic cell nest in origin, and chronic irritation, but to the date, its real aetiology is not clear. One of the suggested pathogenic mechanisms of lipomas called "hypertrophy theory" which states that: Obesity and inadvertent growth of adipose tissue may contribute to the formation of these oral lesions, but this theory is less convincing in explaining those lesions were occurring in areas devoid of preexisting adipose tissue. Another theory known as "metaplasia theory" suggests that lipomas developed due to aberrant differentiation of in situ mesenchymal cells into lipoblast since fatty tissue can be derived from mutable connective tissue cells almost anywhere in the body [9].
Histologically, lipomas are mesenchymal tumours with no sign of cellular atypia composed of mature adipocytes that are subdivided into lobules by septae of fibrous connective tissue, occasionally associated with other mesenchymal elements and usually circumscribed by a thin capsule. They can be classified as simple lipomas, fibro-lipomas, spindle cell lipomas, intramuscular or infiltrating lipomas, angiolipomas, salivary gland lipomas, pleomorphic lipomas, myxoid lipomas, and atypical lipomas. A simple lipoma is the most common diagnosis in the literature as the patient-related herein, which presented with a thin capsule of connective tissue allowing blunt dissection during the surgery [7]. Clinically the features may vary according to the location of the lesion. Usually, they manifest by palpation revealing a soft, painless "resulting in a delay to seek treatment", and mobile mass, sessile to ovoid covered by normal mucosa, which gradually enlarges over several months or years. Usually, deep lipomas are not palpable. It is difficult to distinguish between the mass and the adjacent tissues, especially when the mass is adherent to muscles and salivary glands. Signs and symptoms may include a feeling of fullness and discomfort. Rarely few functional problems like dysphagia, trouble in speech, and mastication have also been encountered in large sublingual lipomas.
In diagnosing lipomas, many investigations may perform include, Fine Needle Aspiration biopsy, which is useful for direct diagnosis. Many imaging techniques could be used to identify soft-tissue masses, such as Computerized Tomography, Magnetic Resonance Imaging, and Ultrasonography. Imaging, in the form of an MRI scan in combination with the clinical findings, resulted in the appropriate diagnosis and management of the condition [1].
The clinical differential diagnosis includes oral dermoid/epidermoid cyst, oral lymphoepithelial cyst, benign salivary gland tumour, mucocele, benign mesenchymal neoplasm, ranula, ectopic thyroid tissue, pleomorphic adenoma, mucoepidermoid carcinoma, angiolipoma, fibro-lipoma, and malignant lymphoma.
The mainstay of treatment for intraoral lipoma is complete surgical excision. In cheek lipoma, an intra-oral approach excision provides an excellent alternative to access the tumour and without esthetic compromise [7]. Generally, the surgical approach is dependent on the site of the tumour and the proposed cosmetic result. No recurrence has been described after local excision, but infiltrative lipoma tends to recur after inadequate excision since they are not encapsulated like simple lipomas.
The prognosis of intra-oral is always good. In adults, the recurrence is rare after complete surgical resection; the complete resection should be emphasized during the first surgical operation, which is the crucial factor in order to avoid recurrence [3].
This case report concludes that:
i. Intraoral approach surgical excision of intraoral lipomas is the perfect treatment with excellent outcome, especially esthetic outcome, which results in patient satisfaction.
ii. Intraoral approach guaranteed no external scarring and reduced the probability of injury to the facial nerve.
iii. The intraoral approach is a relatively simple technique and should be taken into account when considering the surgical removal of cheek lipomas.