Parkinson's disease is one the most widespread illnesses in the world, affecting up to 1% of the whole population above 60 years. It is also considered the most frequent movement disorder and the second most common degenerative disease of the central nervous system. The main goal of prosthodontists should be to guarantee a good quality of life for patients ill with Parkinson's disease (PD).
The PubMed database was used to search the literature published from January 1, 2015 until February 20, 2020. The aim was: 1) To critically review the literature on dental prosthetic treatments that can be done for patients, who have Parkinson's disease; 2) To analyze what is the best time to assign the treatment; 3) To find out how it affects the patients quality of life. Analysis of literature was performed using the PRISMA analysis protocol. Articles were identified in both PubMed and ScienceDirect databases. In each of the studies, we analyzed information for: Prosthetic dental treatment options for patients with PD, most successful approaches to the treatment and factors ensuring good life-quality afterwards.
15 studies were included in the systematic review, according to inclusion and exclusion criteria. It is suggested, that the best way to restore PD patients' masticatory function, is by using implant-supported fixed prosthesis. Also, removable dentures are a viable restorative option for PD patients, although, reduced biting forces and lower jaw movements need to be taken into consideration. Moreover, before any prosthetic dental treatment, the doctor has to be informed about the patients' medication consumption time, to prevent the occurrence of tremors during the visit. In addition, the most viable treatment plan should always be chosen according to patients' quality of life as one of the main factors. For this reason, it is concluded, that non removable restorations increase the patients' quality of life significantly more than removable ones.
Parkinson's disease affects not only mastication, but also swallowing and verbal functions. In order to improve patients' quality of life, these functions need to be rehabilitated by using implant-fixed dental prosthesis as the best option. Because of functional impairment, prosthodontists should pay attention to keeping the patient in vertical sitting position, strictly control salivation, and also assess patients' medication intake time. Moreover, when helping the patients to clearly understand the treatment plan and maintain good oral hygiene, caregivers' assistance is needed. In addition, during aftercare, an electric toothbrush is recommended, since PD patients have trouble sustaining repetitive motions. This is the best way to ensure a successful prosthetic treatment.
Dentistry, Prosthetic, Parkinson's, Treatment, Prosthesis
PD: Parkinson's Disease; ME: Masticatory Efficiency; IV: Intravenous; GOHAI: General Oral Health Assessment Index; OHRQoL: Oral Health-Related Equality of Life
Parkinson's disease (PD) is one the most widespread illnesses in the world, affecting up to 1% of the whole population above 60 years [1]. It even affects up to 1-2 per 1000 people of the whole population at any given moment [2]. It is also considered the most frequent movement disorder and represents the second most common degenerative disease of the central nervous system [3]. Although the causes of Parkinson's disease are mostly unidentified and unknown, the wide occurrence can be explained by up to 3 times increased risk in population, whose family members and siblings had this disease [4]. This disease is usually chronic and causes neurodegeneration in motor and also nonmotor features. This affects not only the patients themselves, but also their families and caregivers, because of restricted mobility and control of their muscles [5]. Various treatment options can help the patient, including drugs, such as dopamine agonists, monoamine oxidase B inhibitors, COMT inhibitors, and Levodopa (L-dopa) formulations [6]. In dentistry, the main goal of prosthodontists should be to guarantee a good quality of life for patients who have PD. One of the most common treatment methods are removable partial dentures, which increase the Oral health-related equality of life (OHRQoL) and also improves patients' masticatory efficiency [7]. It is also very important to evaluate and repair the masticatory function of patient as fast as possible. Patients with Parkinson's disease are sometimes treated with drug L-DOPA, with the international non-proprietary name “levodopa”. During those periods, when patient is receiving this treatment, the masticatory function is impaired [8]. There are even incidents, of levodopa-induced buccolingual masticatory dyskinesia [9]. In order to assure a good oral health-related equality of life, patients' oral health needs to be addressed, multidisciplinary approach is essential, and the treatment can be done with either fixed, or removable prosthesis. The aim of this paper was to critically review the literature on dental prosthetic treatments that can be done for patients, who have Parkinson's disease, to analyze what is the best time to assign this kind of treatment and to find out how it affects the patients quality of life.
Our focused questions were: 1. To review and analyze the literature on available prosthetic dentistry treatments for patients, who are suffering from Parkinson's disease (PD).
2. To review and analyze the literature to evaluate the best prosthetic dentistry treatment timing after consuming PD medication.
3. To review and analyze the literature on quality of life of the patients, ill with PD, who have had their masticatory function restored with fixed or removable dental prosthesis.
Analysis of literature was performed using the PRISMA analysis protocol. The last date of search was 2020 March 1. Article search electronic databases, keywords and filters are described in Table 1.
Table 1: Search information. View Table 1
First, articles were identified in both PubMed and ScienceDirect databases. Keywords "Prosthetic dentistry Parkinson", "Parkinson dental prosthesis", etc. were used, which yielded the most results. During Identification phase, in PubMed, n = 60, and in Science Direct n = 332 articles. Filters for English language were applied. PubMed articles decreased to n = 56, Science Direct had no filter for language. Filters for articles were applied, to be not older than 5 years, clinical trials, controlled clinical trials, meta-analyses and species: Humans. PubMed articles decreased to n = 15. Science direct articles were n = 85. After screening, we evaluated articles for eligibility.
Full-text articles assessed for eligibility n = 15;
Full-text articles excluded, with reasons n = 88.
From these articles, we reviewed and selected 15 articles, describing prosthetic dentistry treatments, available for patients, who are suffering from Parkinson's disease, their quality of life and the best time to make such treatments possible. Inclusion and exclusion criteria are described in Table 2.
Table 2: Inclusion and exclusion criteria. View Table 2
The synthesized results of each article are shown in Table 3. The methodological characteristics of the 15 selected papers were summarized as follows: P-Patients/problem/population, I-Intervention/indicator, C-Comparison, O-Outcome (PICO). Data were collected from the selected articles and arranged in the following fields:
Table 3: Descriptive characteristics of the reviewed articles based on PICO structure. View Table 3
1. Author, year-Describes the author and the year of publication.
2. Population (P)-Describes the demographic features by which the population was selected, including sample size, age, sex, etc.
3. Intervention/Indicator (I)-Defines the disorder diagnostic parameters and research methods used.
4. Comparison (C)-Reveals whether a control group was used and describes its features.
5. Outcomes (O)-Describes the resulting outcomes according to the targets of the study.
The flow diagram of study selection is shown in Figure 1. Of the total of 392 studies identified through the search in the databases, 15 articles were included for the systematic review.
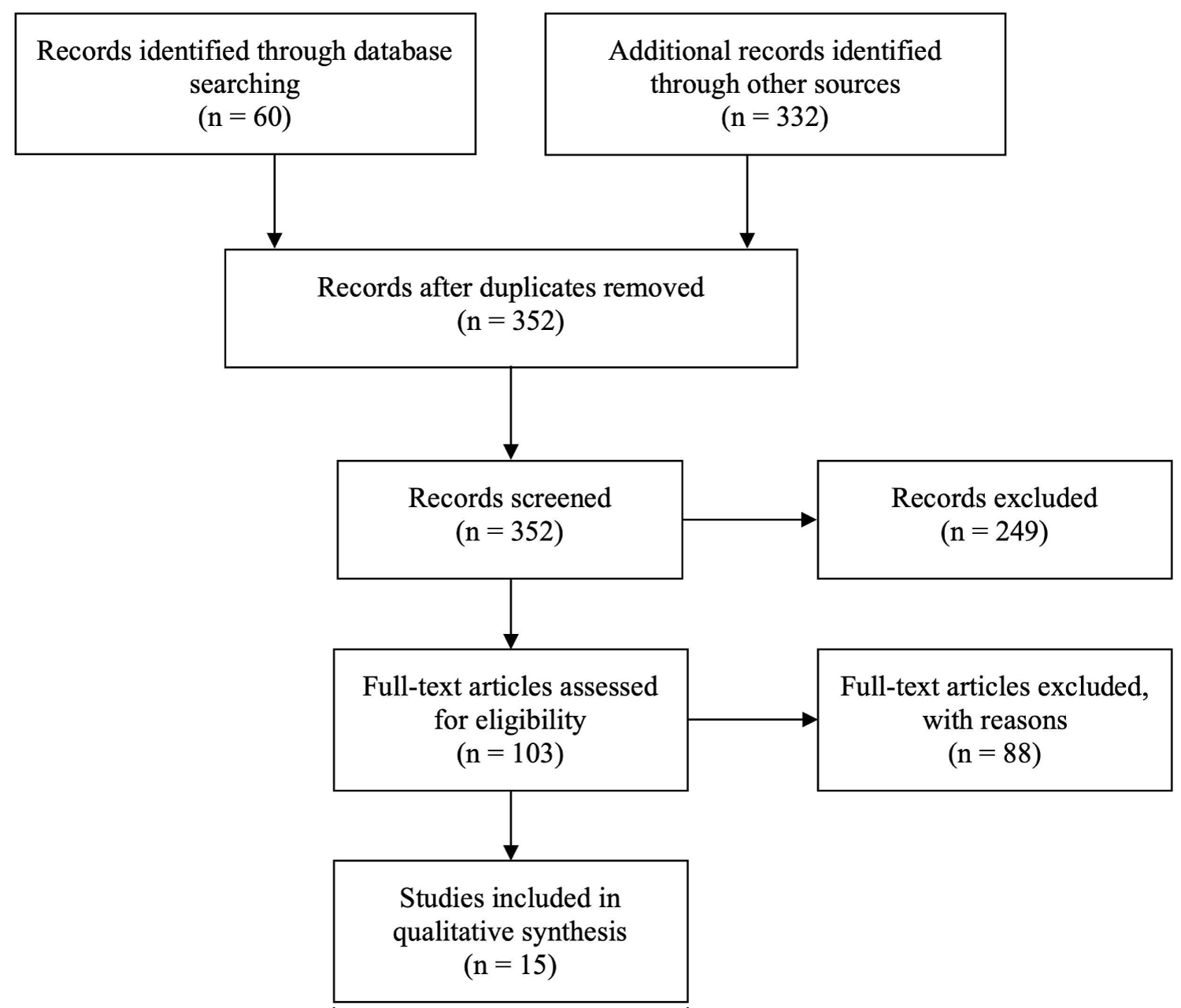 Figure 1: The PRISMA flow diagram of study selection.
View Figure 1
Figure 1: The PRISMA flow diagram of study selection.
View Figure 1
During any prosthetic dental treatment, especially in challenging cases, like PD, it is very important, to maximize the functional, phonetical and aesthetical results. Ribeiro, et al. had observed, that PD has association with impaired masticatory function-reduced lower jaw movements and maximum biting forces [5]. One of the ways to treat PD patients is their masticatory function rehabilitation with prosthesis on implants. Liu, et al. suggested using All-on-4 prosthetic dental treatment, by making a fixed detachable dental prosthesis on 4 implants in the patients' mouth. It proved to be a good choice, with no complications after1-year follow-up, no loss of bone around the implant was present. The soft tissues were also found in good condition [10]. Packer analyzed PD patients and their prosthetic dental treatment plans. In one of the cases, dentures, with removable LOCATOR® abutment systems held for 8 years, but the retentive elements needed to be chosen carefully [11]. Patients, with PD, can have some difficulties in removing the prosthesis from the mouth, if the retentive inserts are too tight, so it is always wise to choose the lighter ones. Also, the inserts in the removable denture, should be used with an angle placement capability, because it may be hard for the PD affected patient to insert them in only one way. It should also be mentioned, that patients with PD have a lower implant survival rate-82%, so treatment should be planned accordingly. Furthermore, the number of implants, that are used to treat prosthetic problems in PD patients, should be kept to a minimum, because of the increased chance of negative outcomes, such as periimplantitis [12]. Nevertheless, two-piece implants are more viable option for prosthetic treatment, than a one-piece system, because, if needed, an implant can be put to sleep [13].
Removable dentures can also be used to treat patients with PD. Although, authors Ribeiro, et al. have observed, that patients with PD have had more biofilm accumulation on their prostheses, compared to non-PD patients. During their research, results were more apparent on the maxillary prosthesis [14]. Also, Fukoka, et al. used video fluorography, which led them to results, that dysphagic PD patients have prolonged duration of tongue pressure, and the time that they take to reach maximum pressure is longer. This may cause problems for the patient, in holding the removable denture in its place [15]. In 2017, scientists Ribeiro, et al. did a research, where they measured Masticatory efficacy (ME), which was calculated according to patients bite force and jaw movements amplitude, and came to a conclusion, that removable dentures improved ME in elder individuals, but it not quite reached the levels of control group [4].
Kaka, et al. described a case with two patients, who suffered dyskinesias, which main relief of symptoms were observed from 30 to 60 minutes after taking medication and their symptoms started reappearing 3 hours after (in this case, the drug that was used was co-careldopa). Also, the same scientists suggested, that for longer treatment periods, a small dosage of Intravenous (IV) midazolam sedation can help reduce the symptoms [6]. Moreover, Boyd, et al. described, that when the patient uses anti-PD drugs (like levodopa, which enhances brain levels of dopamine), it can cause nausea and vomiting, which may aggravate any prosthetic procedure inside the patient's mouth [16]. According to Ribeiro, et al. the prosthodontist needs to evaluate, that during the levodopa "on" periods, the masticatory function of the patient is impaired, and it need to be taken into consideration, if any of the procedures involve these types of movements [5]. Also, the same scientists, Ribeiro, et al. came to a conclusion, that before patients take in levodopa, their mandible range of motion is reduced during specific movements, in this case, protrusion and laterotrusion [17]. It should also be noted, that patients, who have PD, may need a lot of visits for review, and alterations of prostheses. Packer treated 4 patients with PD, and a total of 116 visits were required through a 10-year period [11]. Also, the patient can have impaired swallowing, therefore, dentists should always be careful in leaning back the patient in the chair, which means, that vertical position is more favourable [16]. It should also be noted that the procedure of Deep brain stimulation (DBS) before any kind of prosthetic dental treatment improves patients resting tremor, which helps the clinicians in their work, for example-registering occlusion or taking impressions [10].
One of the main goals of treating patients with PD is to ensure the correct treatment for symptomatic motor and non-motor features of the disease [8]. Fereshtehnejad, et al. in their nationwide study examined individuals with dementia and Parkinsonism, which showed their reduced abilities in utilizing dental care. The most affected groups of patients either had mixed dementia or dementia in the context of Parkinsonism [18]. It should also be noted, that patients, who have PD often develop dysphagia, which can cause serious side effects, such as inability to take medication, malnutrition, and one of the most serious complications-aspiration pneumonia which furthermore reduces the patients' quality of life. For these types of situations, prosthesis on implants is one of the main treatment possibilities, in order to restore patients' masticatory function, and also improve their everyday life quality [19]. Liu, et al. concluded, that rarely, removable denture is a valid type of restoration, because of the involuntary tongue movements, and sialorrhea, which reduces the prosthesis ability to hold well onto the gums, without any additional attachments. Also, relining did not fix the problem. The most favorable type of treatment for this situation is an implant fixed dental prosthesis, rather than an implant-retained overdenture [10].
Patients with PD also usually have a lot of non-favorable conditions, such as xerostomia or sialorrhea. They can also experience nausea, vomiting, which can have negative impact on patients' oral health. It is difficult, for PD patients to brush their teeth, because of the required sustained repetitive motions, therefore, electric toothbrush is recommended, which greatly increases the patients' quality of life [16]. Also, not only the doctors, but also the caregivers should be involved in the prosthetic dental treatment, by learning how to take care of prosthesis on implants [12].
Ribeiro, et al. study evaluated 37 patients (17 of them were ill with PD) according to the General oral health assessment index (GOHAI) who had removable dentures, and the results have shown, that GOHAI Index was low in the PD group of patients, compared to control group, which index was moderate [20]. By making non-removable, all-on-4 implant systems, scientists Liu, et al. observed, that life quality greatly improves with these types of prosthetic restorations, compared to removable ones [10].
1) According to the article data, the most successful form of prosthetic dental treatment for PD patients is implant supported fixed prosthesis. Nevertheless, during regular visits, patient's tissues, around the implant-prosthesis system, should always be evaluated for inflammations in order to avoid peri-implantitis. As an alternative, removable dentures can also be taken into consideration, as a viable prosthetic treatment option for PD patients. Although, in comparison to non-PD individuals, the accumulation rate of biofilm, on removable prosthesis, is higher in the PD patients;
2) Also, for PD patients, the total number of visits to the prosthodontist should be kept to a minimum. Drug consumption time should always be taken into consideration. The procedures should be scheduled 60 to 90 minutes after taking PD medications (e.g. levodopa). This way it is easier to perform manipulations in the oral cavity since the muscle tone, which resists to jaw opening, is minimized and uncontrolled tremor is avoided;
3) In order to increase prosthetic treatment longevity and to guarantee a good quality of life for PD patients, it is very important, that the aftercare includes patients' relatives or caregivers. They should help the patient to clean their teeth and prosthesis, since PD affected individuals have difficulties in sustaining repetitive motions. In addition, an electric toothbrush is recommended, due to more effective results, compared to regular flossing and using a standard toothbrush.
NA.
NA.
The authors have no actual or potential conflicts of interest.
Authors have contributed equally to this research article.