The human larynx is a complex organ, playing a major role in the protection of the lower airway; It's unusual for a foreign body to be inhaled rather than swallowed and when it happens constitutes a real life-threatening emergency. We present a case of a middle age female with a 13-month history of stridor and dyspnea, managed and treated as an asthma patient. After the airway was secured a direct microlaryngoscopy was performed removing the obstruction resulting to be a dental prostheses 50 mm long. This kind of pathology has to be suspected and correctly diagnosed and treated to prevent further complications.
The human larynx is a complex organ that functions as a sphincter in the aerodigestive and respiratory tract junction and plays a major role protecting the airway [1,2]. For this reason, it is unusual for a foreign body to be inhaled rather than swallowed [2,3]. However, when occurs, constitutes a real emergency, requiring immediate medical attention when airflow obstruction is involved [4]. Foreign body aspiration in adults is rare and usually shows nonspecific symptoms and most of them go unnoticed especially if the situation is chronic [5].
We present the case of a 49-year-old female with 13-month history of biphasic stridor and dyspnea, with history of epilepsy treated with levetiracetam and no other important comorbidities. The patient was sent to our service with the diagnosis of subglottic stenosis since her symptoms began thirteen months ago and was treated for misdiagnosed asthma and chronic bronchitis, Nebulized steroid and bronchodilators were prescribed having partial remission of symptoms, slowly progressing with the expiratory dyspnea and stridor.
The rigid laryngoscopy showed a subglottic mass occluding 70% of the light, with preserved chordal mobility.
Computer Tomography (CT) performed as a diagnosis protocol showed in the tracheal lumen a soft tissue isodense mass extending from subglottis to the 3rd tracheal ring, approximately 5 × 10 × 5 mm wide, with irregular edges (Figure 1, Figure 2 and Figure 3).
 Figure 1: Sagittal CT scan with the soft tissue isodense obstruction in the airway (arrow).
View Figure 1
Figure 1: Sagittal CT scan with the soft tissue isodense obstruction in the airway (arrow).
View Figure 1
 Figure 2: Coronal CT scan with the obstruction resembling a membrane or granulation tissue (arrow).
View Figure 2
Figure 2: Coronal CT scan with the obstruction resembling a membrane or granulation tissue (arrow).
View Figure 2
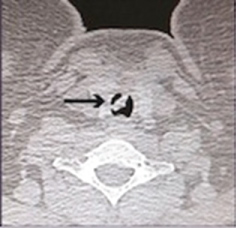 Figure 3: Axial CT scan showing the level of obstruction (arrow).
View Figure 3
Figure 3: Axial CT scan showing the level of obstruction (arrow).
View Figure 3
A tracheotomy was performed under local anesthesia followed by a direct microlaryngoscopy, achieving the removal of the intratracheal mass. The extracted object resulted to be a dental prosthesis about 50 mm long that was surrounded by granulation tissue, which was removed with laryngeal microelectrodes (Figure 4 and Figure 5).
 Figure 4: Transoperatory photograph after removing the strange body, with the granulation tissue underneath it.
View Figure 4
Figure 4: Transoperatory photograph after removing the strange body, with the granulation tissue underneath it.
View Figure 4
 Figure 5: Dental prostheses after removal.
View Figure 5
Figure 5: Dental prostheses after removal.
View Figure 5
The patient was decanulated a week later with no other complication.
The foreign body aspiration is way more common in children than in adults [6,7], approximately 80% of the reported cases are children younger than 15-years-old [8,9]. A history of aspiration can be documented when the patient presents acute symptoms [10], however, when the story is chronic only 3.4% of patients remember the event. The symptoms may differ according to the location with partial obstruction stridor, hoarseness, cough, sore throat, wheezing and dyspnea. This symptomatology often suggests diagnoses of other pathologic processes especially when the history of aspiration is not remembered.
The nature of a foreign body varies significantly according to the cultural and geographic differences in the world [11-13]. Foreign body aspiration although is a rare complication of seizures it derives from a combination of factors, such as impaired swallowing mechanisms and difficulty in attaining adequate patient positioning [14]. The most common aspirated foreign body is food related [8,15], while dental prostheses as in this case, represents up to 27% of cases in adults.
Foreign bodies may go unnoticed for months causing unresolved pneumonia, bronchiectasis [6,16] and lung abscesses, leading to the formation of granulation tissue around the foreign body resembling a tracheal tumor [17].
A foreign body aspiration is a well-recognized complication of orthodontic practice that's why the emphasis on performing and appropriate technique of affixing the dental prostheses to prevent aspirations and to manufacture them with radiopaque materials to prevent misdiagnose. Therapeutic removal of a foreign body can be done through a fiberoptic bronchoscopy with a success rate of extraction in adults of 60-90%. The removal through direct microlaryngoscopy is the most recommended technique, since the surrounding granulation tissue can be resected during the surgical procedure, preventing the organization of subglottic fibrosis.
The Authors have no relevant financial or nonfinancial relationships to disclose.
The Authors have no conflicts of interest to disclose.