Initial infection with VZV causes varicella (or 'chickenpox'). This is a primary infection which can then lie dormant in sensory ganglion cells; when reactivated it is termed herpes zoster [1]. Common reported neurological complications of primary varicella infection are meningoencephalitis and acute cerebellar ataxia [2].
One of the rarer neurological complications of VZV is raised ICP, which was first reported in the literature in a 6-year-old female with VZV [2]. To our knowledge, 8 cases of raised ICP secondary to primary varicella infection or VZV reactivation have been reported in the literature [3]. All the reported cases were amongst children from the ages of 6 to 15-years-old with a predilection towards females (5 out of 8) [3]. This case report is the first reported case of presumed VZV induced raised ICP in an adult.
A previously healthy 19-year-old female presented to the emergency department (ED) with a 3-day history of a band-like headache and low-grade fever of 37.7 degrees Celsius (°C). The headache was associated with nausea and loose stools. Prior to presentation, she was started on acetaminophen and sumatriptan by her general practitioner (GP) with minimal improvement. Her examination was unremarkable with no focal neurology, but no retinal examination was conducted. Apart from a slightly elevated white cell count (WCC 12.3 × 10^9/L) her blood results were normal. She was treated for presumed tension headache with intravenous 0.9% normal saline (2 litres), oral acetylsalicylic acid 900 mg and intravenous metoclopramide 10 mg. Subjective improvement of her headache was noted, and she was discharged. Two days later she represented to the ED with worsening of her headache and vomiting. Neurological examination (without funduscopy) did not show any deficits. Blood tests once again were unremarkable other than a slightly elevated WCC 13.4 × 10^9/L. Her medical management in ED was similar to her previous presentation and she was again discharged home.
She presented two days later with a referral from her optometrist reporting bilateral disc oedema. After discussion with neurology, she underwent a computerized tomography (CT) brain and lumbar puncture (LP). The CT was unremarkable, but the LP opening pressure was > 34 cmH2O. She was started on acetazolamide 250 mg twice daily (BD) and admitted to the neurology ward. Initially, cerebral spinal fluid (CSF) showed WCC 1000 (cells per ml) with 89% mononuclear cells and 11% polymorphonuclear cells (PMNs), protein 1.23 g/L, and glucose 2.6 mmol/L. She was thus commenced on IV 2g Ceftriaxone three times a day (TDS) (for 5 days) and IV Acyclovir 1.2g TDS (for 3 days). The CSF culture detected VZV DNA which confirmed the diagnosis of VZV meningitis. Acetazolamide was ceased. However, the patient continued to experience headaches and vomiting, and a new onset of bilateral visual disturbance was described.
Magnetic resonance imaging (MRI) brain showed no features of encephalitis. Optic nerve sheath distension was noted bilaterally and there was bilateral transverse sinus stenosis. A formal ophthalmology consult was sought. Fundoscopy revealed moderate disc swelling bilaterally with haemorrhages and a cotton wool spot at the right optic nerve head. Optical Coherence Tomography (OCT) confirmed disc swelling bilaterally (RNFL OD 254 µm OS 243 µm - Figure 1) and the Humphrey visual field (HVF) 24-2 was normal. Diamox 250 mg BD was recommenced. Subsequently, the patient's symptoms improved, and she was then discharged on valaciclovir 2000 mg QID for 5 days and acetazolamide 250 mg BD.
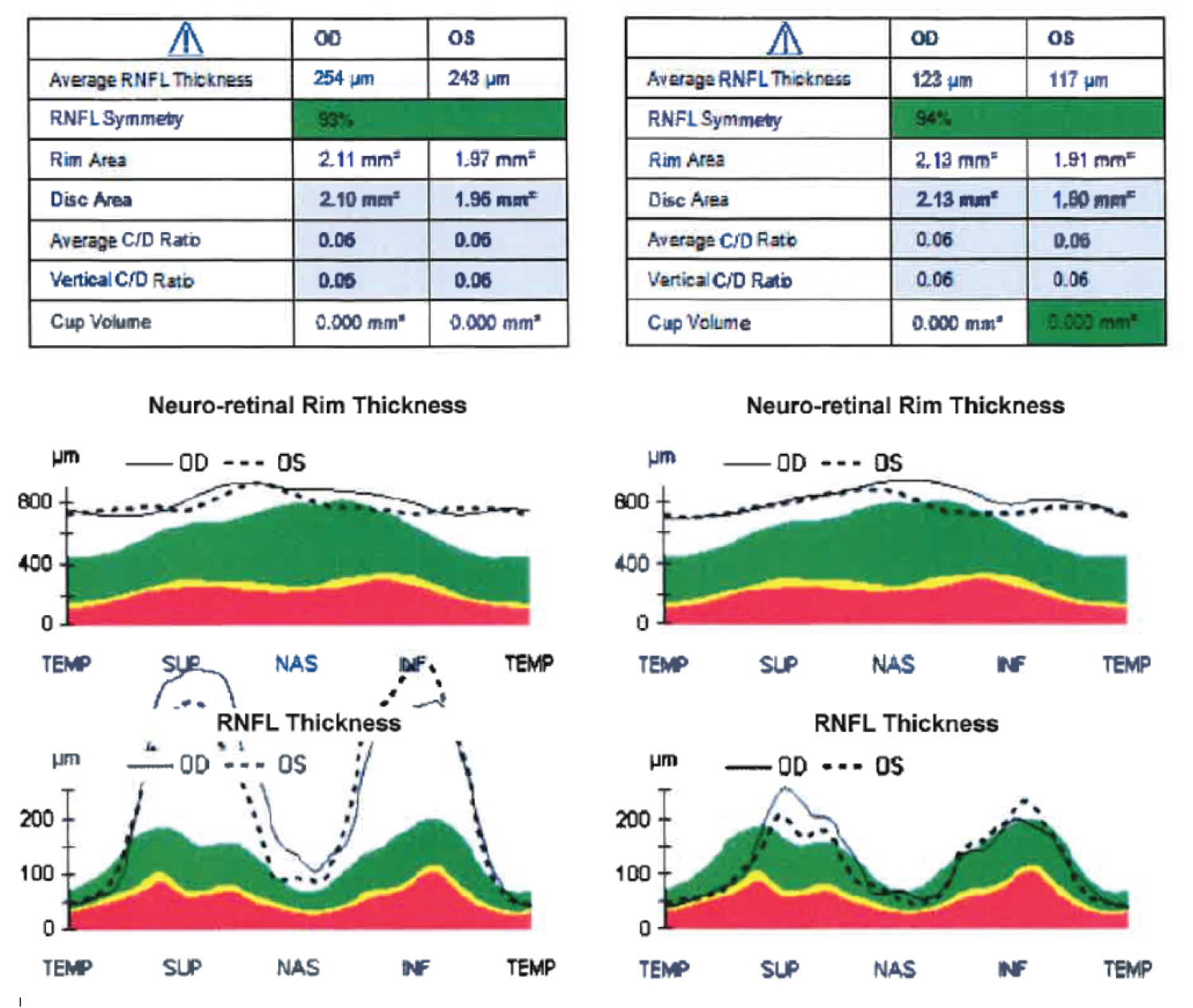 Figure 1: OCT imaging.
Figure 1: OCT imaging.
Left image shows RNFL thickness at presentation OCT RNFL R 254 µm L 243 µm.
Right image shows RNFL thickness at 3-months follow-up OCT RNFL R 123 µm L 117 µm.
View Figure 1
She was followed up in the neuro-ophthalmology clinic one week after discharge. Fundoscopy and OCT revealed worsening (RNFL OD 398 µm OS 360 µm) of disc swelling bilaterally and enlarged blind spots on 24-2 HVF. Acetazolamide was increased to 500 mg BD, and she was advised to start on a weight reduction program as her current weight was 118 kg (BMI 35.2). In the subsequent visit, acetazolamide was increased to 1.25g daily (500 mg/250 mg/500 mg) as there was still no clinical and OCT improvement in her disc swelling. The following week, her disc swelling on fundoscopy, and OCT (RNFL OD 286 µm OS 255 µm) had improved significantly. The follow-up appointment was extended to two weeks where further improvement was noted (OCT RNFL OD 128 µm OS 123 µm). Acetazolamide was tapered to 250 mg TDS with a follow-up appointment in one month. At one-month follow-up, the discs bilaterally appeared healthy and pink with OCT RNFL down to OD 123 µm OS 117 µm as shown in Figure 1. The dosage was reduced further (250 mg daily) before being tapered completely and the patient was followed up in 2 months' time. After 8 months, Diamox was ceased as the optic discs were of normal appearance with a stable RNFL thickness. The patient's weight had also reduced to 110 kgs (BMI 32.8).
Initial infection with VZV causes varicella (or 'chickenpox'). This is a primary infection which can then lie dormant in sensory ganglion cells; when reactivated it is termed herpes zoster [1]. Common reported neurological complications of primary varicella infection are meningoencephalitis and acute cerebellar ataxia [2].
One of the rarer neurological complications of VZV is raised ICP, which was first reported in the literature in a 6-year-old female with VZV [2]. To our knowledge, 8 cases of raised ICP secondary to primary varicella infection or VZV reactivation have been reported in the literature [3]. All the reported cases were amongst children from the ages of 6 to 15-years-old with a predilection towards females (5 out of 8) [3]. This case report is the first reported case of presumed VZV induced raised ICP in an adult.
Patients with raised ICP usually present with headache, vomiting, visual disturbances, and diplopia [4].
Raised ICP secondary to infection is most associated with otitis media, mastoiditis, sinusitis and less commonly associated with viral infections such as measles, VZV and hepatitis A [3]. In such cases, acetazolamide has been prescribed to treat the raised ICP and prevent vision loss due to papilledema [5].
Our patient did not present with the typical features of VZV reactivation such as a rash eruption. The main presenting complaint was a persistent headache, with low grade fever and nausea. In the literature, four of the reported cases had raised ICP secondary to a recent history of primary varicella infection with a typical zoster rash [3]. Only one of the reported cases, where a patient with primary varicella infection, presented with prolonged headache and papilledema from raised ICP, but no skin manifestations. The three reported cases of VZV reactivation presented only with symptoms including headache, vomiting and photophobia before being diagnosed with raised ICP [3]. This reinforces the importance of considering VZV as a potential differential diagnosis in patients presenting with headache due to raised ICP. Furthermore, all patients presenting with prolonged headache should have a fundus examination to assess for disc edema and permit early diagnosis of raised ICP, which was delayed in our patient until she self-presented to an optometrist.
The treatment used in the reported cases was acetazolamide 250 mg twice or four times daily for 3 to 6 weeks resulting in full resolution of papilledema and other symptoms [4]. Only in one study, acetazolamide 250 mg twice daily was used for 6 months [1]. The use of antibiotic (intravenous ceftriaxone for 3 days) with acetazolamide has been reported in only one case [4].
In this case, intravenous Ceftriaxone and acyclovir followed by oral valaciclovir 2000 mg QID for 5 days were prescribed. A tapering regimen of acetazolamide was prescribed, correlating the dosage and frequency with the clinical and symptomatic response. Acetazolamide 250 mg twice daily was initiated, which was increased to a maximum of 1.25g daily and then tapered down with corresponding clinical improvement and symptomatic management over 3 months (Figure 1). Total duration of medical therapy with acetazolamide was 8 months in addition to 7% weight reduction.
In conclusion, early fundus examination should be undertaken in patients presenting with prolonged headache, especially if representing multiple times. Assuming an obese female patient has idiopathic intracranial hypertension without performing a LP and CSF analysis, could lead to misdiagnosis. VZV should be considered as one of the differentials in patients presenting with raised ICP and headache, even in the absence of VZV infection or signs of meningism. The recommended treatment for the raised ICP and papilledema in VZV meningitis is acetazolamide, where the duration and regimen are tailored to the clinical improvement.
All authors contributed to the study conception and design. The first draft of the manuscript was written by [full name] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
The authors have no relevant financial or non-financial interests to disclose. There is no funding to declare.
This case report adhered to the tenets of the Declaration of Helsinki. The patient involved in this case report has been de-identified. Verbal informed consent for participation and publication was obtained.