Objective: To document a case of macular hole managed with an innovative new procedure, the Inverted Flap Technique of Internal Limiting Membrane (ILM) Peeling.
Methods: A 67-year-old female presented with central visual loss on left eye for more than a year. Pre-operative visual acuity of counting fingers at 2 feet. Baseline macular Optical Coherence Tomography (OCT) showed a large full thickness macular hole measuring 710 μm in diameter associated with chronic cystoid degenerative changes and posterior vitreous detachment. The patient underwent Closed Vitrectomy with Inverted Flap Technique of ILM Peeling. Intra-ocular air tamponade was done and face down position was advised for 5 days.
Result: One-month post-operative showed reduction in size of the macular hole with a decrease in diameter to less than half (310 μm) of its initial measure (710 μm). Three months post-operative showed decreased diameter to 262 μm. Visual acuity improved from counting fingers at 2 feet to 3/60 to 5/60 respectively.
Conclusion: The Inverted Flap Technique of ILM Peeling is capable of successfully managing even large and chronic full thickness macular hole resulting in limited recovery of vision.
ILM peeling, Macular hole, Inverted Flap Technique
The macula is the center of the retina responsible for 80-90% of functional vision as we know it. Hence, pathologies afflicting this prime half millimeter at the back of the eye result in profound visual disability. A macular hole is defined as a partial or full thickness defect of the neurosensory retina in this region. It has a prevalence of 3:1000 individuals with peak incidence of onset in the 6th-7th decade of life. The majority of patients complain of central visual loss beginning with metamorphopsia, micropsia or scotoma1. Accepted pathophysiologic mechanisms include vitreomacular traction and the centripetal traction from surrounding epiretinal membranes producing the histologic split in the fovea [1]. Optical Coherence Tomography (OCT) represents the prime diagnostic tool in evaluating and staging of the macular hole [2].
Macular surgery has been accepted to be one of the more successful procedures that can restore functional vision. It classically entails 1) The near-total removal of the vitreous gel and stripping of its attachment to the retina; 2) Dissection and stripping of the Internal Limiting Membrane (ILM); 3) drainage of subretinal fluid with concommittant fluid to air exchange; and d) Postoperative tamponade and positioning. The procedure aims to close the defect by relieving the tangential forces resulting to closing the edges of the lesion [3]. Done properly and within the appropriate time, visual results have averaged fair and functional results of 20/50 or better [4]. The size of the break (> 400 um), duration of symptoms (> 6 months), and chronicity (cystoid degenerative changes) are factors that dampen the subsequent visual prognosis of the condition and its management [5]. Closure rate after 6 months was only 58-68% for large macular holes with a diameter of greater 400 um. Visual prognosis after 6 months was improvement of less than 3 lines in chart [5].
Recently, a technique was developed to increase the chances of macular hole closure. So, in this case report, instead of conventional ILM peeling, the ophthalmologist does ILM peeling using the Inverted Flap Technique for a purpose of better closure and visual outcome. Michalewska, et al., have reported that using the inverted ILM flap technique improved the closure rate to a 98% and postoperative visual acuity as high as 3 more lines [5].
Hence, this report presents the surgical result of this technique in this institution.
A 67-year-old female patient came in at the De La Salle University Medical Center Out-Patient Department with a chief complaint of central blurring of vision on left eye. The patient reported decreased visual acuity of more than a year after she accidentally covered her one eye. She described it as a small black spot. The size of 25 centavo coin, with no other signs and symptoms noted. She had no medications taken or instilled. No consultation was likewise done.
However, on the day of consult, she noted an increase in the size of the black spot to as much as 4 times. This prompted patient to consult. Patient is non-diabetic. However, she is hypertensive with maintenance medication of atenolol 50 mg/tablet twice a day. She has no history of ocular surgeries and trauma. She started using reading glasses at age of 38.
Physical examination was done. Distance best corrected visual acuity on left eye is counting fingers at 2 feet. Near visual acuity is J1+ corrected. Gross examination, extra-ocular muscles examination, and intra-ocular pressure examination are normal. Funduscopy of left eye revealed dull foveal reflex.
Ancillary examinations such as amsler grid test revealed a central scotoma on left eye, slitlamp biomicroscopy with 90D lens revealed (+) Watzke-Allen and round defect on left fovea. Indirect ophthalmoscopy revealed no other abnormalities. Impression then was Full Thickness Macular Hole Stage IV with Posterior Vitreous Detachment. Optical Coherence Tomography (OCT) of left macula was requested for staging and visual prognosis.
OCT of left macula (Figure 1) showed a defect with a diameter of 710 um, with cystoid changes and posterior vitreous detachment. These indicate poor visual prognosis when operated using the present technique of pars plana vitrectomy with internal limiting membrane peeling. Despite the odds, patient remained optimistic that the pars plana vitrectomy with internal limiting membrane peeling using INVERTED FLAP TECHNIQUE will improves her vision.
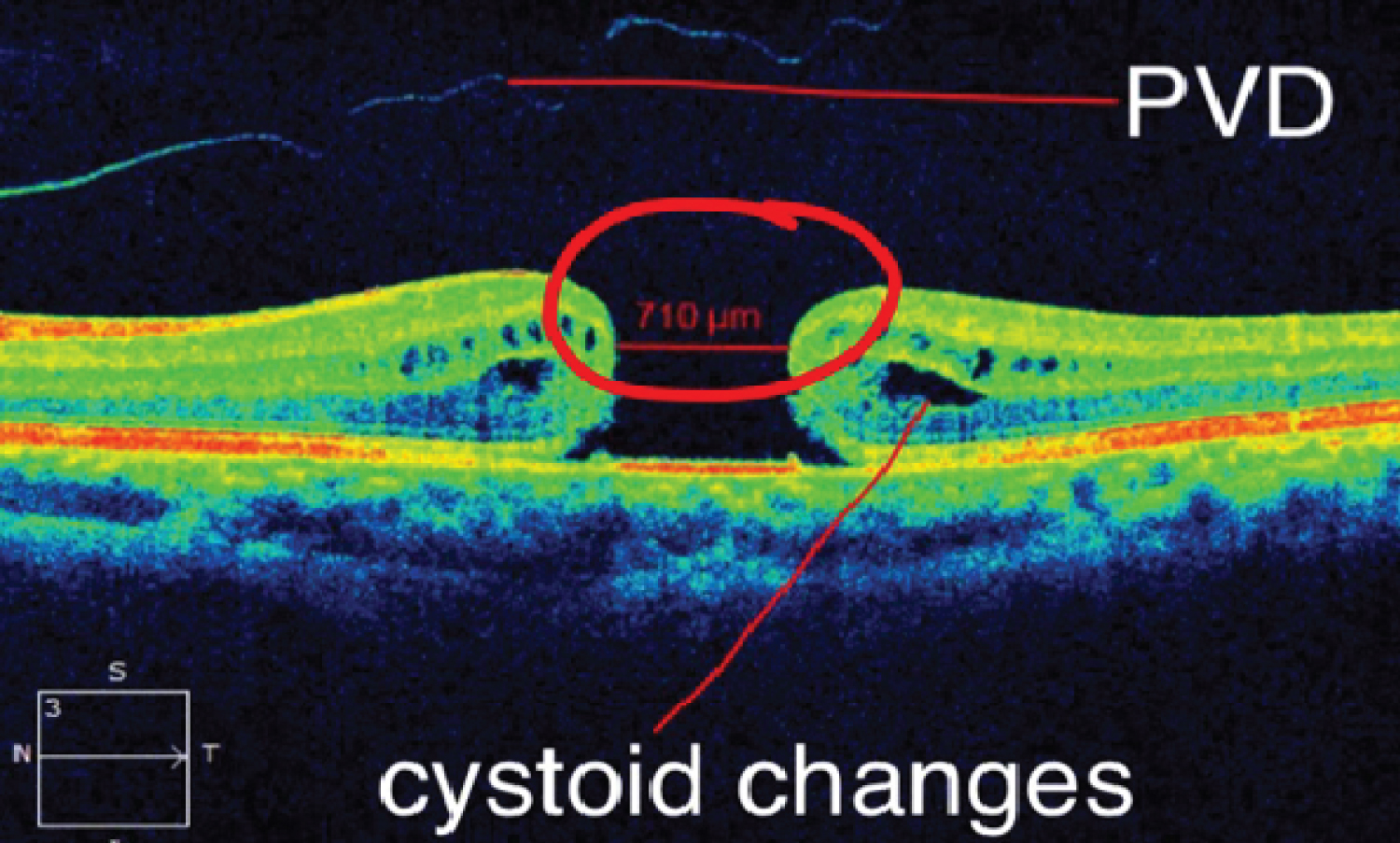 Figure 1: OCT macula OS.
View Figure 1
Figure 1: OCT macula OS.
View Figure 1
Since stretching the retina sufficiently to close the macular hole would be difficult in this case, pars plana vitrectomy using the inverted ILM flap technique, based on the method reported by the recent studies 5-8 was then proposed.
After performing a 23-gauge micro-incision pars plana vitrectomy using intraocular forceps, brilliant blue dye was injected to better visualize the ILM. ILM was peeled away from the periphery towards the macular hole in 4 directions, leaving the attachment to the edge of the macular hole in place. So that, a bowl-shaped ILM flap was created. It was then trimmed half of the peeled ILM using a vitreous cutter, to facilitate the inversion of the ILM. The remnant ILM was inverted to cover the entire macular hole. Fluid-air exchange was performed, and patient remained face-down for 5 days after surgery [5] (Figure 2).
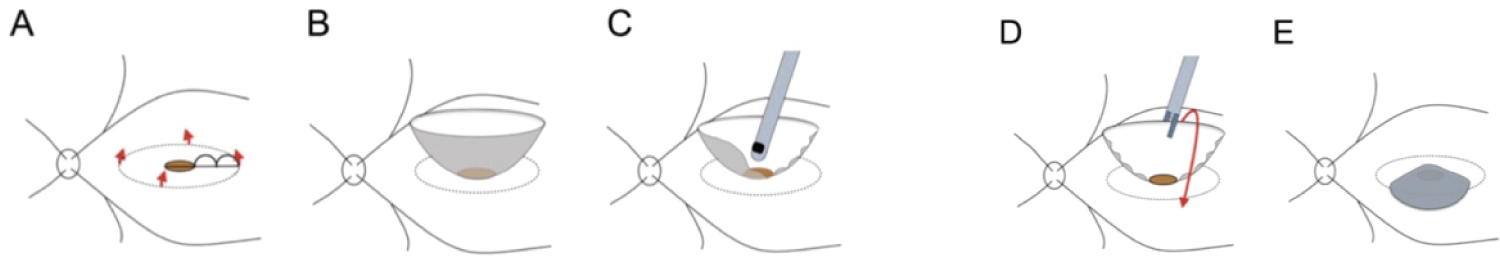 Figure 2: Diagrammatic representation of ILM peeling using Inverted Flap Technique.
View Figure 2
Figure 2: Diagrammatic representation of ILM peeling using Inverted Flap Technique.
View Figure 2
a. ILM was peeled off in a circular fashion. Red arrows show the direction of ILM peeling.
b. The ILM was not removed completely from the retina. It remained attached to the edge of the macular hole.
c. Then trimmed half of the peeled ILM using a vitreous cutter, to facilitate the inversion of the ILM.
d. The remnant ILM was inverted with intra-ocular forceps to cover the entire MH.
e. Fluid air-exchange was injected.
Face down position was discontinued after 5 days. One month and three months post-operative, visual acuity was 3/60 and 5/60 respectively. Repeat OCT was done (Figure 3).
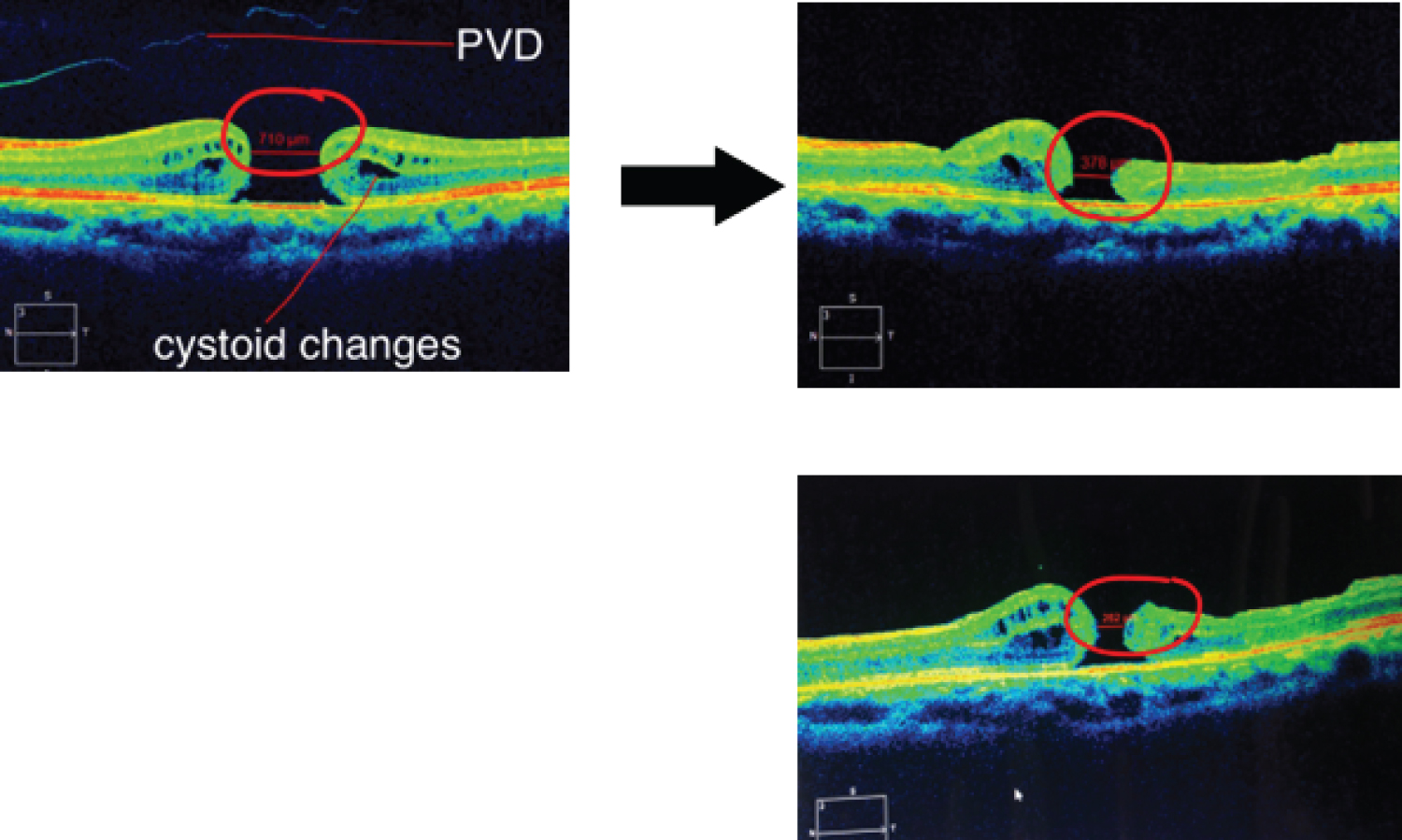 Figure 3: OCT after one month and three months post-operative.
View Figure 3
Figure 3: OCT after one month and three months post-operative.
View Figure 3
Diameter of macular hole decreased from baseline of 710 um to 378 um to 262 um.
The improvement in technique and development of finer instrumentation in vireo-retinal surgery has significantly improved the surgical outcome of macular hole in terms of anatomical and functional success [6].
The most reliable factor affecting the surgical outcome following the surgery is the size of the hole and its chronicity. A number of studies have established that diameter of the hole and duration are closely related to the rate of anatomic success [6,7].
It is hypothesized that the inverted ILM flap technique stimulates proliferation of glial cells that fill macular hole, thereby enhancing closure and improving closure rates [5]. In the neural tissues of the retina, activation of glial cells occurs in response to any form of injury and has protective effects. Müller cells are the principal glial cells in the retina and play crucial roles in supporting neuronal function. At any stage of tissue damage, gliosis is an important neuroprotective event that is thought to be a cellular attempt to limit the extent of tissue damage [8-10].
Improvement in visual acuity was believed due to the scaffolding effect of the muller cells. It connects the remaining photoreceptors to each other thereby enhancing neuronal transmission [7].
In this report, anatomic success was measured through OCT results from pre-operative to one month and three months post-operative. The functional outcome was the improvement of visual acuity. Both anatomic and functional outcome have shown improvement. However, larger study group and longer follow-up period are required to further evaluate this technique.
Complications may include iatrogenic retinal breaks, retinal detachment, vitreous hemorrhage and endophthalmitis [11].