Background: Adult-onset xanthogranuloma (AOX) is a rare, non-Langerhans histiocytic disorder of the orbit, typically presenting without systemic involvement.
Methods: We report the case of a 48-year-old male with a 7-year history of progressive, painless right upper eyelid swelling.
Results: Imaging revealed a well-circumscribed, enhancing intraconal mass, and histopathological examination following orbitotomy confirmed xanthogranulomatous inflammation. Stains for infectious organisms were negative, and no systemic abnormalities were identified, supporting a diagnosis of isolated AOX. Although the patient experienced transient improvement with corticosteroids, definitive management required surgical excision.
Conclusion: This case highlights the importance of considering AOX in the differential diagnosis of chronic orbital masses and underscores the role of histopathology in establishing a definitive diagnosis.
Ocular xanthogranuloma refers to a group of rare, non-Langerhans histiocytic disorders and is characterized by the presence of foamy histiocytes and Touton giant cells within ocular tissues. Further classified into juvenile xanthogranuloma (JXG) and adult-onset xanthogranuloma (AOX), these disorders can present with distinct clinical presentations and histopathological features. Juvenile xanthogranuloma (JXG), typically seen infants and young children, present as yellow-tinged nodules on the corneoscleral limbus, conjunctiva, or iris. Histopathology may show Touton giant cells and foamy histiocytes, with positive CD68 staining and negative S-100 and CD1a staining [1,2]. JXG is typically asymptomatic and tend to spontaneously regress. Adult-onset xanthogranuloma (AOX) is less common and can present similar to JXG with nodules at the corneoscleral junction. However, management often involves surgical excision, especially in the case of corneal involvement, to prevent sight-threatening complications as these lesions do not typically regress [4-6]. We present the case of a 48 year-old male with a superior orbital mass found to be xanthogranuloma through biopsy. Collection and evaluation of protected patient health information were HIPAA compliant and adhered to the tenets of the Declaration of Helsinki.
A 48-year-old Caucasian male presented with painless edema of the right upper eyelid, progressively worsening over a span of 7 years. He reported partial symptomatic relief during multiple courses of corticosteroid therapy and was taking 10 mg of oral prednisone at the time of initial evaluation.
On examination, findings included right upper lid ptosis, inferior globe displacement, and medial canthal fullness with a subtle yellow discoloration (Figure 1). Visual acuity was 20/30 in the right eye, intraocular pressure measured 12 mmHg, and extraocular movements were full. Color vision testing was normal (15/15 Ishihara plates), and Hertel exophthalmometry showed measurements of 17 mm OD and 16 mm OS (base 95 mm). Orbital MRI revealed a 2.7 x 1.1 x 3.2 cm heterogeneous enhancing intraconal soft tissue lesion seen within the anterosuperior aspect over the right globe (Figure 1A). There was inflammation surrounding the lateral and superior rectus muscles without lesions involving the optic nerves. No abnormal lesions were seen in the left orbit. The patient underwent a right orbitotomy with biopsy of the orbital mass. Intraoperatively, a yellow, fibrotic, encapsulated lesion was identified and excised from the superior aspect of the globe (Figure 1B). Pathology revealed xanthomatous inflammation consistent with xanthogranuloma on gross examination. Histopathological analysis showed no evidence of fungal organisms (GMS stain negative), acid-fast bacilli (AFB stain negative), or mycobacterial DNA (PCR negative), ruling out infectious etiologies. Upon follow up, patient had mild edema following completion of prednisone course but did not have any complications. Patient continues to follow with oculoplastics (Figure 2).
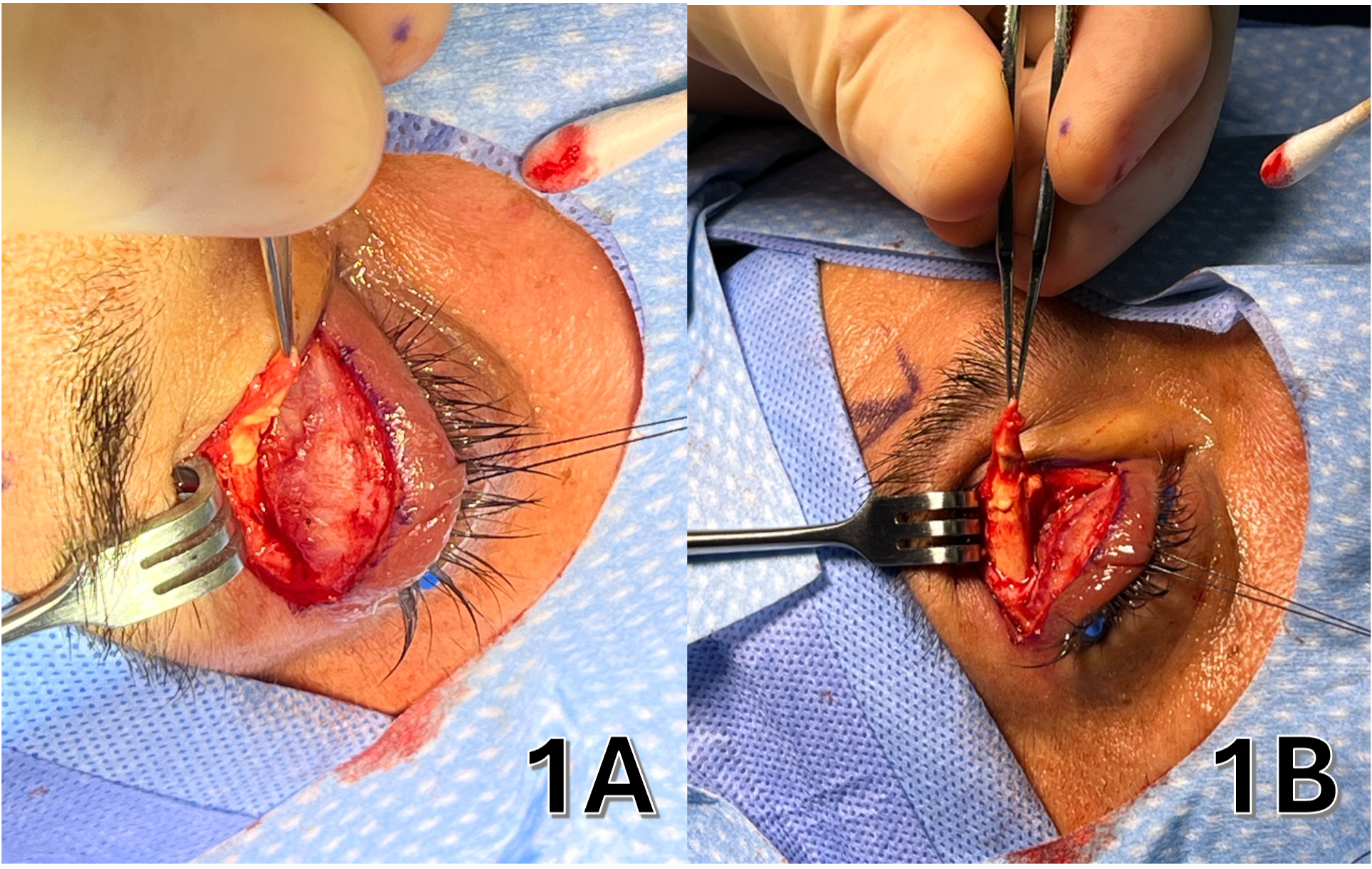 Figure 1: Peri-operative photos of patients with yellow-tinged medial canthus lesion.
View Figure 1
Figure 1: Peri-operative photos of patients with yellow-tinged medial canthus lesion.
View Figure 1
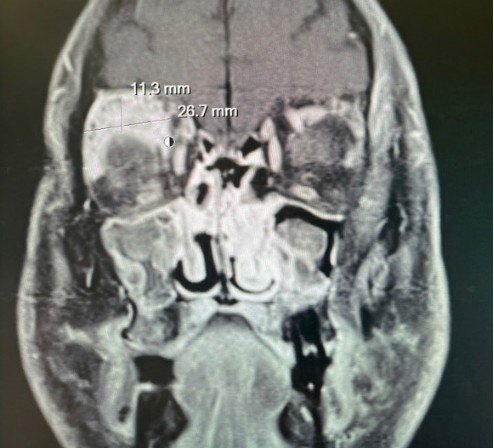 Figure 2: Coronal T1-weighted MRI revealing enhanced 2.7 x 1.1 cm mass at the right superior orbit.
View Figure 2
Figure 2: Coronal T1-weighted MRI revealing enhanced 2.7 x 1.1 cm mass at the right superior orbit.
View Figure 2
Adult orbital xanthogranulomatous diseases can be further broken down into four subtypes: AOX, adult-onset asthma and periocular xanthogranuloma (AAPOX), necrobiotic xanthogranuloma (NXG), and Erdheim-Chester disease (ECD). AOX, as seen in the described case, presents without accompanying systemic abnormalities. This distinguishes it from the other subtypes, which often involve systemic associations such as asthma (AAPOX), paraproteinemia (NXG), or multisystem involvement including bone and cardiovascular systems (ECD).
The absence of systemic symptoms or laboratory evidence of hematologic or autoimmune disease supported the diagnosis of isolated AOX in this patient. Imaging findings of a well-defined, hyperdense mass involving the lacrimal gland and histopathology ruling out infectious etiologies, confirmed the diagnosis. Management of AOX primarily involves surgical excision, as the lesions are less likely to regress spontaneously compared to their juvenile counterparts. While corticosteroids may offer transient reduction in inflammation or edema, they often do not prevent recurrence or progression of mass effect. In our case, the patient experienced partial relief with systemic steroids but ultimately required orbitotomy and lesion excision for definitive management.
Close follow-up is essential, as recurrence has been documented, and although rare, systemic associations or transformation to more aggressive histiocytic disorders may develop over time. Therefore, periodic systemic evaluations including hematologic and imaging work-up are warranted despite an initial isolated presentation. This case emphasizes the importance of including xanthogranulomatous disease in the differential diagnosis of chronic, painless orbital masses in adults. Histopathologic confirmation remains the gold-standard for diagnosis, and surgical management can provide both diagnostic tissue and symptom relief.