Charcot neuroarthropathy (CN) is a syndrome that was first described over 300 years ago. Sir William Musgrave was the first person to define neuropathic osteo-arthropathy in 1703 as an arthralgia whereby he described that syphilis was the supreme cause. 178 years later, Jean-Martin Charcot, (1825-1893) gave a thorough description on the condition in the year 1886 [1]. Consequently, the condition was named after him. Charcot defined the condition as a continuous, denervation-induced decadence of the foot and ankle [2]. Charcot's description remained valid until 1936 when Jordan documented that the condition occurs as a result of miscellaneous Peripheral neuropathies. However, Jordan considered Diabetes Mellitus as the primary possible agent causing neuropathic osteo-arthropathy. Since that time, Jordan's consideration was adopted as the main etiology of Charcot arthroplasty to this date.
CN refers to a devastating aggravation of diabetes mellitus (DM) affecting bones and joints. CN mainly affects the osteoarticular architecture of the foot and ankle joint causing subluxation, dislocation, deformity, and ulceration [3,4] stated that bone prominence lesions affecting midfoot due to the deformity of the osteoarticular architecture stimulate the collapse of the medial arch. CN Early diagnosis followed by rapid treatment measures may be incompetent as the risk of amputation is heightened [5]. 15% of diabetic patients at are prone to cultivate diabetic heel ulcers at one point. Around 14% to 20% of diabetic patients requires amputation [6].
The objective of the current paper is to:
1. To outline the Etiology/Biomechanics CN affecting the midfoot.
2. Classification.
3. Treatment and outcomes.
The precise etiology of CN is not properly comprehended. CN refers to a severe condition perturbing the musculoskeletal system and the tender tissue progressively. CN causes joint deformity and pathological fractures at any joint of the human body. The weight-bearing joints at the foot and the tarsus are the common sufferers of this ailment. There are multiple factors causing diabetic heel problems, tangential vascular ailment, traumatization, disease and neuropathy. The condition is observed in patients suffering from diabetes, venereal disease, leprosy, poliomyelitis, alcoholism, and micro trauma. Disruption of blood circulation weakens the bone hence making joints prone to dislocations and fractures.
Diabetic neuropathy and the presence of foot ulcers are known to be the main causative factor. Neuropathy is the main factor and complication of diabetes causes a delay in the manifestation of pain that helps in early diagnosis. It is usually present in 30-50% rising up to 78% CN cases in a pre-existing injury in some patients. DM results in loss of pain susceptibility and escalates the risk of joint movement limitation. It also increases the risk of digital pathology, prominence in the middle portion of the foot causing an increased plantar pressure in its turn leading to ulcers formation accompanied by other factors like age, obesity, sex, immobility, deformities and foot hyperkeratosis [7].
Biomechanics is a study that illustrates the movement of the body utilizing kinetics and kinematics. A human gait cycle begins with one foot contacting a rough surface and ends when the same foot touches the surface again. Gait revolution is divided into gait phases; the stance phase involves loading response (when a foot is in contact with a rough surface), mid-stance (when the opposite foot is off the surface, while the other foot is bearing full body weight), terminal stance (propulsion phase) or referred as heel-off the ground ending when the toe is off the ground, and, swing phase which is further subdivided into three time frames. In the swing stage the heel is in the air; therefore, it starts after the toe-off and finishes with the first ground connection of the reference heel. The swing phase can be separated into the first swing, mid-swing and final-swing phases or acceleration phases. It starts when the foot leaves the surface until when the knee reaches its maximum flexion. In its turn, the ankle dorsiflexes to secure stability and the foot is carried forward. The entire process also relies on ground reaction forces (GRF) as the body advances forward or backwards [8].
The human foot is a sophisticated shock absorbing structure consisting of soft tissue, bones and joint. The foot functions as a force transmitter between rough surfaces (ground) and the lower limb, supporting and balancing, in ambulation, and stance, by performing biomechanical changes that enable the foot to act as a rigid lever on external surfaces to provide walking stability and plasticity [9]. The role of the hind foot is inversion and eversion of the foot. The hind foot involves the talus, calcaneus, and the cuboid. It also comprises of subtalar, calcaneocuboid (CC) and talonavicular (TN), together named as midtarsal, transverse tarsal, or Chopart joint, which stabilizes the midfoot and hind foot to act as a rigid lever at heel rise.
The midfoot acts in abduction and adduction. The midfoot is made of the navicular, cuboid, fifth metatarsal, fourth metatarsal, and three cuneiforms which are shaped convexly on their dorsal aspect whereas plantar surface is concave giving an impression to point inferiorly to the apex. The midfoot through cuneiforms also articulates with tars metatarsal (TMT) joint, distally (lisfranc joint) which consists of bone and ligaments to provide stability to the joint. All structures located distally to TMT are referred to as the forefoot. Midfoot articulates between the navicular and the cuneiforms. The navicular lies medially to the cuboid articulating with the head of the cuboid anteriorly acting as a key-stone at the medial longitudinal arch. The midfoot structure with the conjunction of ligamentous (longitudinal and transverse ligaments on the plantar and dosal aspect of the joint) and muscle connectivity are considered to be the contributing factors to the stability of the midfoot that is essential for push-off in gait cycle and movement. Midfoot is the connecting structure between the hind foot and the forefoot providing the necessary stability and flexibility needed for various activities and essential for a normal gait. The forefoot incorporates the metatarsal and phalanges. Where the first metatarsal is the shortest and second metatarsal is the longest which makes it more prone to stress fractures than other lesser toes, while lesser toes are under the influence of both. The first metatarsal carries 50% of body load in the course of the gait cycle [10].
The Charcot foot was classified according to its clinical (Acute or chronic) phase, anatomical restriction, and condition of natural background.
Charcot foot patients could be present in either the Acute or the Chronic stage.
The acute stage is a pathological condition mainly affecting the midfoot. Patients exhibit discomfort, painless, red, and warm swollen foot similar to cellulitis. At this stage, the physician examines the foot using an infrared thermometer detecting an increase of 2-6 ℃ compared to a healthy foot. The chronic stage is distinct from the acute stage. It is defined as an inactive stage since there is no significant difference in an affected foot temperature compared to a healthy foot. However, redness and inflammation subsides, it is frequently replaced by a clear presence of rocker bottom deformity due to collapse of midfoot plantar arch and midfoot prominence at the medial convexity of the foot. These deformities are due to elevated pressure areas susceptible to ulceration [11].
[12] reveal that the most widely used classification is the Brodsky anatomic classification of Charcot foot arthroplasty (Figure 1 and Table 1).
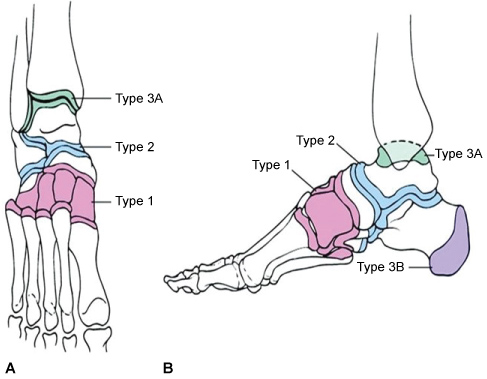 Figure 1: • Category 1 (midfoot) arthroplasty pertains the navicular cuneiform and tars metatarsal joints.
Figure 1: • Category 1 (midfoot) arthroplasty pertains the navicular cuneiform and tars metatarsal joints.
• Category 2 (hind foot) pertains the Chopart and/or subtalar joint.
• Category 3A (ankle) pertains the tibiotalar joint; Category 3B (calcaneus) embroils a fragmentation of the calcaneal tuberosity. Trepman, et al. modified the classification to encompass:
• Category 4 (multiple areas) and 5 (forefoot), which correspond with sequential or coincident involvement of numerous areas and metatarsophalangeal entanglement, respectively” (Table 1).
View Figure 1
Table 1: Brodsky anatomic classification of Charcot arthropathy (Types 1-3B) with Trepman, et al. modification (Types 4 and 5). View Table 1
Natural history classification was published in 1966 as "Charcot joint" by Sidney N. Eichenholtz, (1909-200). Eichenholtz, described the three stages as (I) Buildup; (II) Conglutination; and (III) Reestablishment and reconstitution (Table 2) [13] in which he described the advancement over a period of time lasting from weeks to years. Eichenholtz's, studied a group of patients diagnosed with DM, venereal disease, alcoholism, leprosy, and syringomyelia. Each patient was suffering from arthropathy in the heel, tarsus, knee, and hip joints. Shibata, et al. included an additional phase later. It is described that the clinical signs of Charcot arthropathy always occurs before radiographic changes [12].
Table 2: Eichenholtz classifications [13]. View Table 2
Other classifications existing to Identify ulcer characteristics in the treatment of CN are of crucial significance in evaluating the etiology of an ulcer to if the lesion is ischemic, neuropathic or neuro-ischemic. Because of that purpose, classifications have been introduced as a method to assess severity of lesions by determining the ulcer size, its depth, presence of ischemia, infection and neuropathy [14].
Most important classifications:
• Wagner-meggit subdivision mechanism.
• Brodsky Depth-Ischemic subdivision.
• University of Texas subdivision.
• International Working Group gradation.
The main manifestation of CN in the foot and ankle joint is by causing various foot deformities and complications. These deformities include rocker under foot impairment from midfoot Charcot neuropathy, front foot supinates, front foot abduction, back foot medical transcription, tarsus contracture and Varus calcaneus. There are two types of treatment for this condition, nonsurgical and surgical. Physicians exhaust all therapeutic methods before resorting to surgery when treating Charcot neuropathy. These therapeutic techniques include removal of all intrinsic and extrinsic factors (trauma, improper shoes). They also consider other factors acting on the foot that enable the minimization of plantar pressure like immobilization and stress reduction of the affected foot. Minimizing pressure load is crucial due to patients' loss of sensation in the affected foot. Early intervention diminishes the condition and it might even prevent the tissue damage that leads to ulceration. A non-weight bearing regime (long bed rest) walking aids (crutches) are other things doctors examine before recommending surgery. However, patients find it difficult not to bear weight or endure a prolonged bed rest. Dr. Paul Wilson Brand asserts that total contact cast (TCC) is the most effective immobilizing method that is highly beneficial for patients suffering from plantar neuropathic ulcers of the front foot and middle foot. TCC is maintained for a lengthy period until the inflammatory stage resolves. It lasts up to 12.5 weeks and after its removal, patients are advised to acquire custom footwear with extra shoe depth and a rigid sole like a Charcot orthotic walker (CROW). Nonetheless, the recurrence of an infection and ulcers leading to instability of the joint will end up with surgical intervention [6,15].
There are various surgical treatments of midfoot CN; internal and external fixation methods, bone graft, osteotomy, or a combination method. [16] considered intramedullary foot fixation (IMFF) as the suitable method to stabilize/fuse a Charcot midfoot deformity. The crucial point in surgical intervention is to ensure formal fixation of entire medial column connections with the patient posing supine knee placed at a 90° angle. A 1.8-mm Ilizarov cable is immersed through the plantar aspect of the initial MTPJ focalized to the initial MTP head while dorsiflexing the first MTPJ maximally. The same approach is performed with the third or fourth metatarsal and medial column stabilization through the second metatarsal. The whole procedure is done AP and in Lateral fluoroscopy 7.0/8.0-mm alignment pins are immersed and verified under anteroposterior and lateral fluoroscopy. The spherical screws are then interpolated. IMFF final stages is indicated by inserting two moderately threaded 7.0/8.0-mm bolt, and one entirely threaded cannulated 7.0/8.0-mm bolt.
During surgery, a proper anatomical realignment preserving the foot length and joint fusion above CN collapse to finally achieve a stable plant grade, and full ambulation with a custom-made shoe [16,17]. The Ante grade mechanism for a Medial Column Beam bolt in Midfoot CN starts in a posterior position of the talus. Nevertheless, surgeons consider the posterior approach risky because of the presence of an anatomical structure prone to injuries during the procedure (neurovascular bundle, Sural nerve, Tarsus joint, Flexor halluces, Achilles tendon, Posterior tibia, longus tendon, and peroneal tendon sheath). Consequently, surgical procedures encounter Postoperative complications like wound dehiscence and irritation soft-tissue, infection osteomyelitis, delayed union and non-union of the fusion [18].
Amputation is considered as the last resort intervention. It is performed after the presence of recurrent ulceration or the failure of arthrodesis due to the difficulty in treating the spreading infection. Amputation could minimize the patient's suffering by avoiding multiple surgeries and a lengthy hospital stay. Amputation can be performed on various limb levels. However, a transtibial amputation is favorable since it is considered easier to obtain and use prosthesis [19].
Using routine Magnetic Resonance (MR) imaging to differentiate between osteomyelitis and osteoarthropathy is difficult. Despite both the high sensitivity and specify of MR imaging for osteomyelitis in the foot, osteoarthropathy can mimic infection on MR imaging with regards to bone marrow edematous changes following gadolinium administration therefore making differentiation difficult. The ability to differentiate between these conditions is further hampered as infection often coincides with neuropathic disease [20-24]. As such, advanced MR imaging techniques have been applied with regards to the investigation of CN, however, similar results were identified between dynamic contrast enhanced MR imaging and proton MR spectroscopy [23,25].
In 2017, Razek, et al. studied the diagnostic performance of diffusion weighted MR imaging in differentiation of diabetic osteoarthropathy and osteomyelitis in the diabetic foot. It was concluded that the apparent diffusion coefficient (ADC) value can aid in the differentiation between osteoarthropathy (high ADC value) and osteomyelitis (low ADC value) [26s].
The initial symptom of acute CN is reactive skeletal inflammation; therefore, MR imaging is the primary imaging modality in detection of CN. On MR imaging, the reactive skeletal inflammation is seen as bone marrow edema which is a result of inflammatory cell invasion and vascular and connective tissue proliferation [27] Early use of MR imagine improves the identification, management and prognosis of CN [28].
CN remains to be an immense challenge to treat and it is not precisely understood. This is due to the devastating complications, neuropathy, bad bone quality, insufficient vascularity and bad nutrition leading to delayed healing in patients with DM. Various treatment techniques, both conservative or surgical, aim to reduce ulcerations of the foot, decrease deformity, maintain anatomical alignment, provide a rigid interosseous fixation, preserve the foot and minimize the risk of amputation. The most important matter is a successful outcome after treatment. A surgical principle helps in the progression of the healing process by stabilizing the foot axial load since the fusion involves single or multiple joints. Despite limitations, surgical treatment remains important as it acts on limb salvation. The major necessity is to have an early diagnosis followed by a fast-interventional treatment method.