Background: The National Heart and Lung Institute's guidelines advise against routine use of chest X-ray (CXR) for acute asthma exacerbation. Despite this recommendation, unnecessary CXR are still being performed. The objective of this study is to assess the association between abnormal CXR findings and the severity of asthma exacerbation and its impact on acute asthma management.
Methods: A retrospective chart review was performed of all pediatric patients 2-17 years of age who presented to the emergency department (ED) with acute asthma exacerbation between July 2017 and June 2019. Demographics, asthma severity, clinical parameters, and management were reviewed. Associations between severity of asthma and clinical management of patients with and without abnormal CXR findings were evaluated.
Results: Total of 2691 patients presented with asthma exacerbation to the ED. A total of 197 patients in whom CXR was performed, were included; 62% were male, 56.9% were between 5-11 years of age, 39.6% had abnormal CXR and 53.3% had a mild exacerbation. There was no significant association between abnormal CXR and severity of asthma (p = 0.104). More patients with abnormal CXR were given antibiotics and had a longer length of stay (p = < 0.0001 and p = 0.02 respectively). The need for supplemental oxygen and epinephrine were higher in patients with normal CXR (p = 0.036 and p = 0.033, respectively).
Conclusion: Abnormal CXR findings do not differ among patients with mild compared to moderate and severe asthma exacerbation. Those with abnormal CXR received more antibiotics and had a longer hospital stay. Further prospective studies are needed to delineate the use of CXR related to the severity of asthma exacerbation and the need for antibiotics in cases of abnormal CXR.
Asthma, Chest X-ray
Bipap: Bi-Level Positive Airway Pressure; CXR: Chest X-Ray; ED: Emergency Department; ICD: The International Classification of Disease; NAEPP: National Asthma Education and Prevention Program; PAS: Pediatric Asthma Score; SPSS: Statistical Package for Social Sciences Program
Asthma is a significant medical and public health-related burden and resulted in 1.6 million ED visits in 2018 [1]. Despite the increasing prevalence, important gains have been observed including better exercise tolerance and a decrease in mortality following the release of the NAEPP [2]. The total number of asthma-related deaths reported in the USA in 2019 was 3524 (death rate of 10.7 per million population) out of which 178 (death rate of 2.4 per million population) were children and adolescents less than 18 years of age [1]. The severity of asthma exacerbation on presentation to the emergency department can be classified clinically based on the PAS tool into mild, moderate, or severe [3]. Various treatment strategies are being used to treat acute asthma in acute care settings including short-acting beta-agonist, steroids, magnesium sulfate, and mechanical ventilation [4].
The National Heart and Lung Institute's guidelines advise against the routine use of CXR [5]. These suggestions are based on various studies which have shown that it has little yield and affects clinical judgment in an insignificant number of patients [6]. The number of CXR can be effectively reduced without impacting clinical outcomes [7]. Despite the current recommendation, unnecessary CXR are still performed [8]. Additionally, there is a limited investigation of the association of abnormal CXR with the severity of asthma and its impact on clinical outcomes. The purpose of this study is to assess the association between abnormal CXR findings and the severity of asthma exacerbation and the association with acute asthma management. We hypothesize that abnormal CXR findings have no association with the severity and management of asthma.
This is a retrospective study of all presentations for acute asthma exacerbations to a single center in New York City made by children and adolescents aged 2-17 years, inclusive, over a 24m period from 7/17 to 6/19. The study examined associations between abnormal CXR, and severity of presentation defined by the PAS, use of ancillary treatments, and length of stay. The study only included those participants who had both a CXR and a the PAS that could be calculated for them retrospectively.
All patients, presented to the emergency department, who had wheezing or respiratory distress and had either a prior diagnosis of asthma or reactive airway disease or had a history of one or more prior episodes of wheezing treated with inhaled bronchodilators were included. There were no institutional guidelines in place for obtaining CXRs in patients with acute exacerbation of asthma during the time the CXRs were taken.
Patients with underlying congenital heart disease, bronchopulmonary dysplasia, cystic fibrosis, sickle cell anemia, congenital or acquired immunodeficiency, or those who had CXR already done outside our ED and patient with incomplete data classifying them into different categories of severity were excluded. Demographic data including age and sex were recorded. Clinical data including the severity of asthma exacerbation based on PAS score [5], need for treatment such as supplemental oxygen therapy, BiPAP, continuous albuterol treatment, magnesium sulfate, terbutaline, epinephrine, antibiotics, endotracheal intubation, chest tube placement, cardiopulmonary resuscitation, death and length of stay were reviewed. Abnormal CXR was recorded as reported by the radiologist.
The PAS was used to classify the severity of asthma exacerbation [5]. The PAS is an asthma scoring system and had been used in various studies and has good interrater reliability (Pearson correlation statistic, 0.92) [9]. Based on the PAS score, patients were classified as having mild (PAS 5-7), moderate (PAS 8-11), or severe (PAS 12-15) asthma exacerbation.
The data was analyzed using Statistical Package for Social Sciences program (SPSS; IBM, Chicago, IL, USA) software.
Descriptive data were represented for each group, as a percentage for categorical variables. Comparison of baseline characteristics between the groups was tested using the chi-square test for categorical variables and the T-test for continuous variables. Comparison of normal and abnormal CXR findings among age groups was done using the Chi-square test. Comparison of normal and abnormal CXR findings between groups of patients with mild compared to moderate and severe asthma and the type of treatment provided was also done using the Chi-square test. For hypothesis testing, a p-value of less than 0.05 was considered significant.
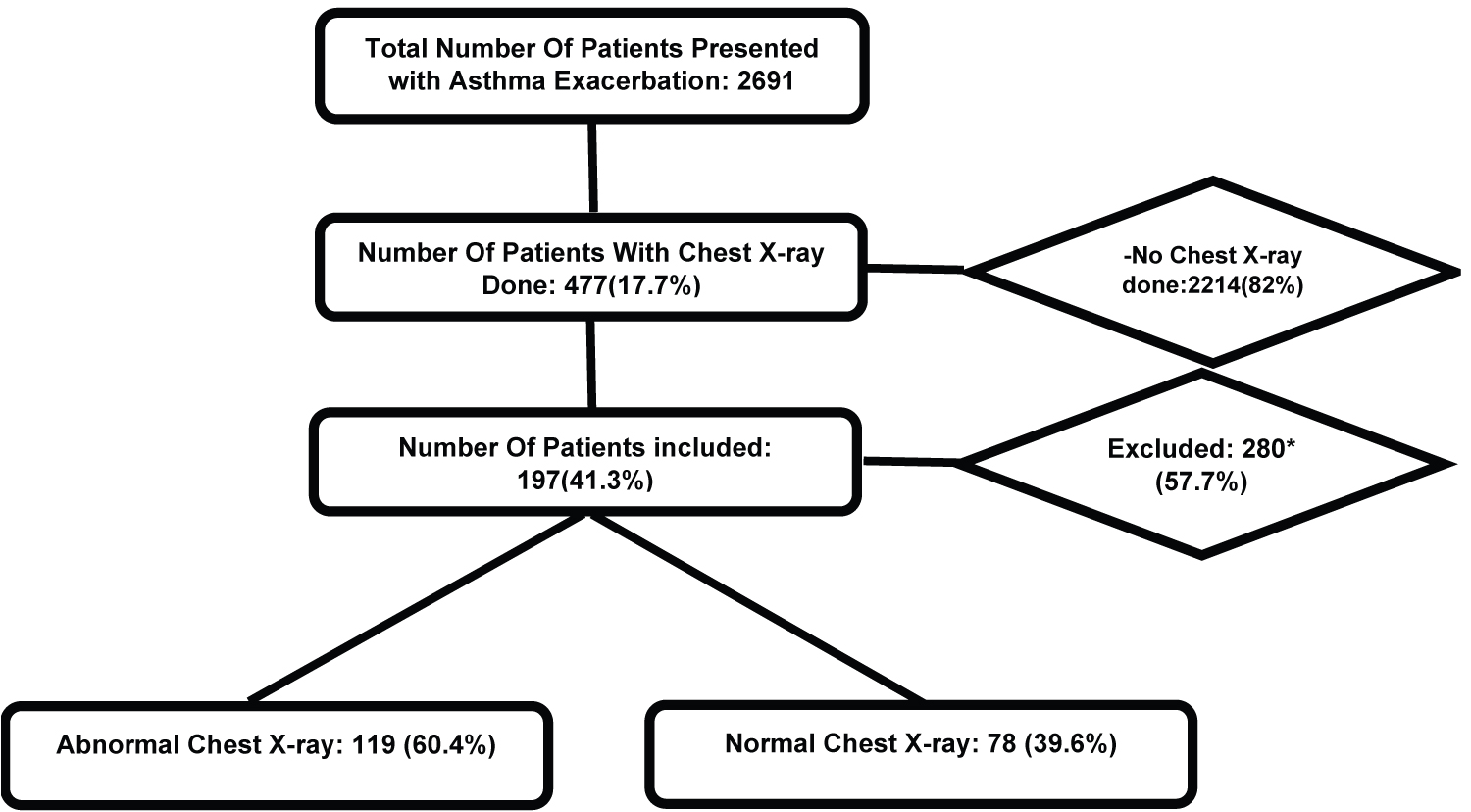
The cases were identified using the ICD Code 10. Of a total of 2691 patients' visits between July 2017 and June 2019, 2214 (82%) patients were excluded as CXR was not performed in those patients. Out of 477 (18%) of patients in whom CXR was performed, 280 (58%) were excluded due to incomplete information on charts for classification into different severity categories of asthma. 197 (42%) of patients with CXR were included in the final analysis (Flowchart).
Demographic and baseline clinical parameters are included in Table 1. Sixty two percent (62%) were male, 56.9% were 5-11 years-old and 53.3% had mild exacerbation of asthma. Abnormal CXR findings were present in 40% of patients. Forty four percent of patients required supplemental oxygen, 22% of patients required BiPAP, and 1 patient (0.5%) was intubated. No patient required cardiopulmonary resuscitation, and none died in this group of patients. 44% of patients received antibiotics and 72% were given magnesium sulfate. Forty-six percent of the patients required a hospital stay beyond 2 days.
Table 1: Demographic characteristics and frequencies of variables. View Table 1
The use of supplemental oxygen (52% vs. 47%) and epinephrine (91% vs. 9%) was significantly higher in the normal CXR group compared to the abnormal CXR group (p = 0.036 and p = 0.033 respectively) while the use of antibiotics (59% vs. 41%) and length of stay (2.8 days vs. 2.2 days) were significantly higher in the abnormal CXR group (p = 0.0001 and p = 0.02 respectively) compared to normal CXR group (Table 2). The use of antibiotics was significantly higher in the age groups 2-4 years (62% vs. 17%) and 5-11 years (76% vs. 33%) with abnormal CXR (p = 0.002 and p = 0.0001 respectively) compared to the group with normal CXR, however, there was no difference in the use of antibiotics in the age group 12-17 years (37.5% vs. 36%) with abnormal CXR (p = 0.881) compared to normal CXR group (Table 3).
Table 2: Association of abnormal chest X-ray findings with management of asthma. View Table 2
Table 3: Use of antibiotics in different age groups with abnormal chest X-ray findings. View Table 3
There was no statistically significant difference in abnormal CXR findings in patients with mild vs moderate to severe asthma exacerbation (18.3% vs. 21% with p = 0.104) (Table 4).
Table 4: Association of abnormal chest X-ray with severity of asthma. View Table 4
This study shows that there is no significant difference in the proportion of abnormal CXR between mild compared to moderate and severe asthma exacerbation. Previous studies have shown that performing ancillary testing such as blood testing and CXR routinely, adds little to the management of asthmatic children and may lead to unnecessary cost, pain, and radiation exposure [6,7,10].
We found that patients with abnormal CXR received antibiotics more frequently (59% vs. 41%, p-value = 0.0001) and had longer stays in the hospital (2.8 vs. 2.2 days, p-value = 0.02). The association of abnormal CXR findings with the use of antibiotics is previously studied and is inconclusive [11]. Certain features such as immunosuppression and chronic diseases may incline the physician towards using antibiotics with abnormal CXR [12]. In other cases, the clinicians may practice “defensive medicine” in the settings of uncertainty where the probability of litigation is present [13]. The use of supplemental oxygen and epinephrine was more common with those with normal CXR.
Overall, abnormal CXRs were more frequent in the younger age group. This is likely related to the airway anatomy as well as the prevalence of viral infections in this age group leading to asthma exacerbation [14-16].
The proportion of patients in whom CXRs were performed in asthmatic children in this study is 18% which is significantly lower compared to the previous studies in children with wheezing where CXRs were performed in 37% to 72% of patients [7,17]. This may be related to efforts at both national and institutional levels to reduce the number of CXR in the asthmatic patients' [5].
Our study has several limitations. It is a retrospective chart review performed at a single center. We excluded 58% of patients in whom CXR was performed due to missing data and has the potential to bias the results. Abnormal CXR classification was based on radiologists' interpretation who had access to the patients' history and could result in potential bias in reporting. Due to the retrospective nature of the study, the indications for starting antibiotics were not documented and are not fully known.
This study continues to support the limited utility of CXR in the acute exacerbation of asthma management. In fact, the use of CXR may lead to unnecessary interventions and potential harm. Further prospective studies are needed to further delineate the use of CXR related to the severity of asthma exacerbation and the use of antibiotics in cases of abnormal CXR.
None.
None.
All authors are responsible for reported research. All authors have participated in the concept and design, analysis, and interpretation of data, and drafting or revising of the manuscript, and they have approved the manuscript as submitted.