The main objective of the present study is to investigate the effectiveness of the ventilatory strategy in decubitus in the prone position in patients with severe acute respiratory syndrome triggered by Covid-19.
This is an integrative literature review combined with the snowball technique, based on the following question: "What are the effects of the protective ventilatory strategy in prone decubitus in patients with SARS secondary to Covid-19? PUBMED and Academic Google were used as database, using the descriptors Artificial Respiration, Mechanical Ventilation, Cannula nasal high-flow, Pronation and Covid-19, from March 2020 to April 2021.
Seven articles were analyzed. The theoretical bases that supported this study are based on various sources, but may have as guiding elements the publications of the Ministry of Health, establishing an overview of conducts in respiratory treatments during the pandemic, combined with empirical research and perspectives, noting that in 10 SARS patients, all intubated, 6 of them were submitted to standard and PP position, 3 to PP and 1 only to standard, with satisfactory results. Similar research indicates that the prone position provides an increase in saturation to 95.9%, a decrease in pain complaints, an improvement in oxygenation and a decrease in mortality.
The findings obtained from this scenario involving the various sources consulted were that the practice based on scientific evidence ensures quality care and offers subsidies that provide knowledge and updating. Although PP has been elucidated since 2008, with the pandemic this became more evident and showed that it is effective in improving the oxygenation of patients with a PaO2/FiO2 ratio ≤ 150 mmHg and safe to be applied, as long as the institution train and qualify the team involved in the maneuver process and that they have strict controls and follow-up on possible complications.
Severe acute respiratory syndrome, Prone position, Covid-19
The virus spread around the world causing repercussions in various sectors of society is officially known as SARS-CoV-2, in English Severe Acute Respiratory Syndrome. The number 2 means that it is the second generation of the infectious micro-organism. The first caused an epidemic of SARS-CoV in 2003, which caused a disease similar to the pandemic faced in 2020/2021, more lethal, however, with lower contagion power, spreading less and which ceased more fast, according to Sobrinho, et al. [1]. The disease caused by this virus is currently called Covid-19, in English, Coronavirus Disease 2019, where the number 19 refers to the year when the disease recurred [2].
In view of the succession of events, in December 2019, a set of cases of pneumonia, caused by a newly identified β-coronavirus, initially named as the new coronavirus 2019 (2019-nCoV) was observed in Wuhan, China. 10, however, on January 12, 2020, the World Health Organization (WHO) officially named this disease as the new 2019 coronavirus known as Covid-19 [3].
On March 11, 2020, the WHO characterized the epidemiological scenario as a pandemic, as it was widely disseminated around the world [4]. According to the Pan American Health Organization, on August 29, 2021, in Brazil, the total number of cases reported is 20,741,815, with 579,308 deaths [5].
Furthermore, the end of 2019 and the beginning of 2020 brought new challenges to the world, which had to deal with a virus of little known evolution, highly contagious and that triggers a picture of severe acute respiratory disease. Covid-19's main form of contagion is droplets and aerosols generated by speech, coughing, sneezing, secretions or direct contact [4]. Acute respiratory disease can cause Severe Acute Respiratory Syndrome (SARS), secondary to Covid-19, which causes significant impairment of the lung parenchyma with severe hypoxemia, and consequently, the need for treatment with mechanical ventilation [6,7].
The correct strategies in mechanical ventilation (MV), aiming at protective ventilation, help to reduce lung injury induced by MV and improve the picture of hypoxemia. Among these, the Pronation Position (PP), with evidence level A, according to the III Brazilian Consensus on MV, ensures the maintenance of ventilation/perfusion and should be applied to patients with a PaO2/FIO2 ratio ≤ 150 mmHg per hair. At least 16 consecutive hours, PP being widely indicated for patients with SARS secondary to COVID-19 [8,9].
PP is a procedure in which the patient is placed in the prone position in order to reduce hypoxemia. Studies show that this strategy brings benefits such as improved ventilation-perfusion (V/Q), reduced pulmonary shunt and improved pulmonary compliance. It is noteworthy, however, that it must be performed by a trained and multidisciplinary team [8,10].
Although the physiological mechanisms of PP are not well elucidated, according to Guerra, et al. [11], the overload of organs and structures acts on alveolar ventilation and peripheral oxygenation levels. Changing the decubitus position promotes the redistribution of alveolar liquid contents, leading to a thinner alveolar-capillary membrane, favoring the diffusion of gases.
Given the above, the performance of the work is justified by the incidence of cases of the disease worldwide and by the number of people who need in-hospital care because of the severe clinical manifestations of Covid-19, in many cases having the need ventilatory support through MV. Thus, the objective is to carry out an integrative literature review on the effectiveness of the protective ventilatory strategy with the prone position in patients with SARS secondary to Covid-19.
The study is an integrative literature review, one of the techniques used in Evidence-Based Practices, which enables the incorporation of study results into clinical practice [12]. Thus, the integrative review can be used as a strategy to generate knowledge in the health area, as it allows for the inclusion of different methodologies and because it is capable of helping researchers to synthesize theoretical and empirical literature on a specific topic [13]. The stages of elaboration of this review followed the following order: 1: Formulation of the theme and elaboration of the guiding question; 2: Rescue of publications in selected databases; 3: Synthesis and analysis of the information evidenced in the studies; 4: Analysis of selected studies; 5: Presentation of results; and 6: Critical analysis of the findings.
The strategy (P - population; I - intervention; C - comparison; O - outcomes) [14] guided the development of the guiding question: What are the effects of the protective ventilatory strategy in prone recumbency in patients with SARS secondary to Covid-19?
To answer this question, from March 2020 to April 2021, searches for scientific evidence were carried out in the PUBMED and Academic Google databases, using as descriptors those established in the DeCS (Descriptors in Health Sciences) platform of the Virtual Health Library (VHL). The search strategy was systematized in these databases using the Boolean operators "AND" and "OR" as follows: (Respiration, Artificial OR "Artificial Respiration" OR "Artificial Respirations" OR "Mechanical Ventilation" OR " Mechanical Ventilations" OR "Respirations, Artificial" OR "Ventilation, Mechanical" OR "Ventilations, Mechanical" OR "High-flow nasal cannula" AND "Pronation" AND COVID-19 OR "coronavirus infection").
The methodological approach was based on the analysis of the titles, abstracts and full reading of the selected manuscripts, adopting as inclusion criteria articles on respiratory physiotherapy in the prone position, mechanical ventilation in a patient with SARS secondary to Covid-19, and respiratory physiotherapy in the Covid-19. After selecting the articles that met the study's inclusion criteria, the snowball method was used for non-systematic identification of works that are potentially of interest for research by searching the references of articles previously included in the work [15].
It is considered that this study investigates and presents the scientific evidence in respiratory physiotherapy for the treatment of Covid-19, aiming to guide health professionals in clinical practice.
Initially, 649 articles were found. After reading the titles, abstracts and review steps, seven articles were included. The search and selection of studies are presented according to the PRISMA instrument (Preferred Reporting Items for Systematic Review and Meta-Analyses) (Figure 1).
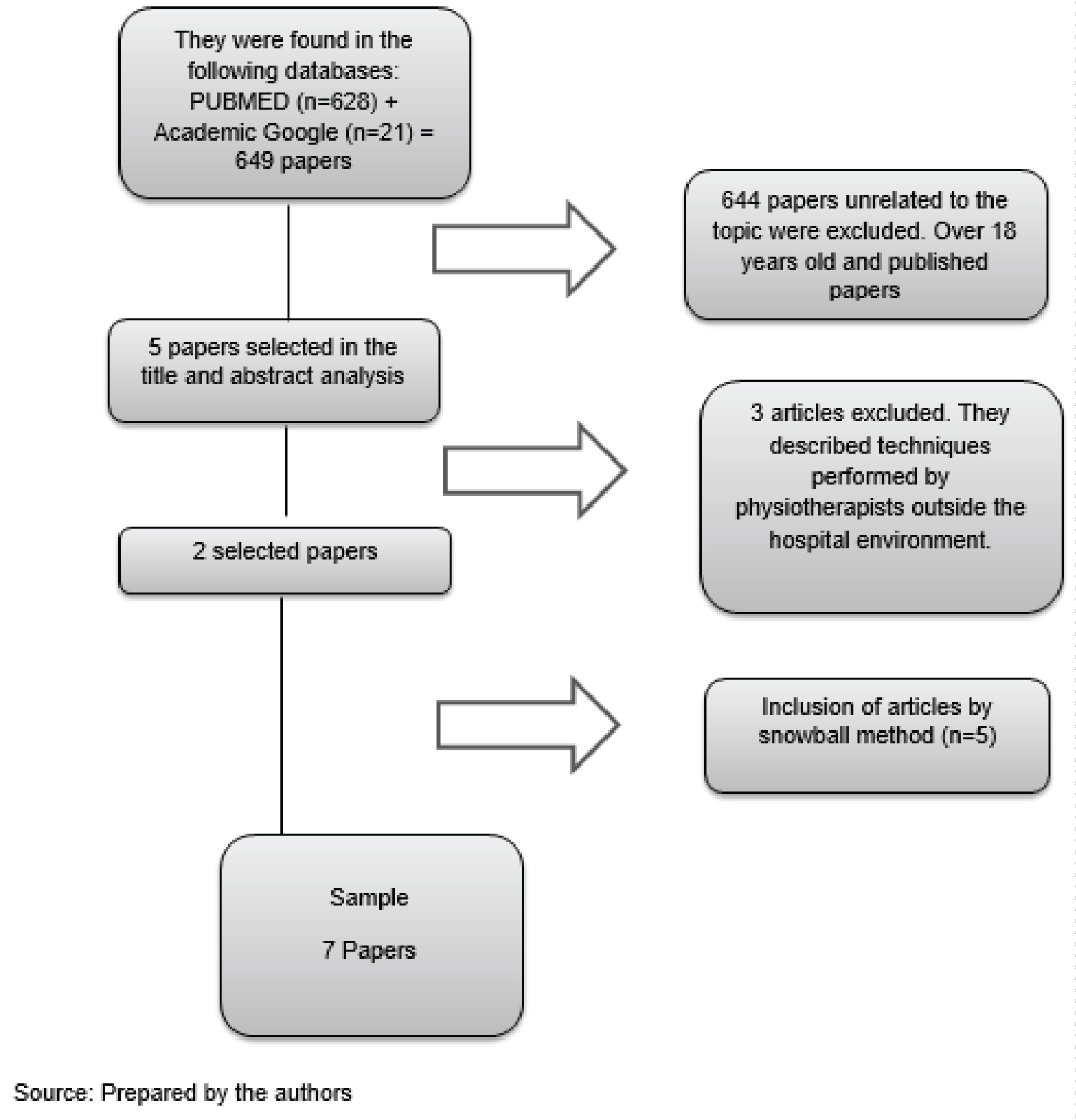 Figure 1: Study selection flowchart.
View Figure 1
Figure 1: Study selection flowchart.
View Figure 1
Table 1 below shows the characteristics of the studies included in the integrative review, with the names of the authors who prepared the studies, the place where the studies were carried out, year of publication, target audience and organizing institution.
Table 1: Characterization of selected studies. View Table 1
Table 2 shows the strategies developed in the field of Respiratory Physiotherapy aiming at mitigating and reducing physiological complications caused by Covid-19.
Table 2: Activities developed in Respiratory Physiotherapy to minimize Covid-19. View Table 2
From what was observed in the selected evidence, some important issues can be highlighted. The first is that of the patients infected by Covid-19, about 5% to 26% needed care in the Intensive Care Unit (ICU), according to Thuler and Melo [23]. And the authors complement by stating that among the complications triggered by the new coronavirus, SRAG is between 31% and 67%. A study carried out by Borges, et al. [24] highlights Covid-19's prone position in the treatment of acute respiratory failure, warning of contraindications and complications in its use in the intensive care setting. The authors observed that, in relation to intubated patients, as for PaO2/FiO2 ≤ 150 mmHg, the prone position is the prominent strategy, as it brings benefits of improving oxygenation.
In this same sense, a second question that is in line with the study highlighted by Borges, et al. [24] and that helps to understand the reflection obtained through this integrative review is: considering the decrease in lung compliance, the time under mechanical conditions , which is related to the mortality of patients observed in the studies reported, in line with the clinical management protocol for the new coronavirus issued by the Ministry of Health, it is noteworthy that a PP assigned to patients with severe SARS to improve oxygenation, with the caveat that patient safety is guaranteed. In this protocol we clearly see the operational definitions for Covid19, general characteristics for an infection, care, treatment and prevention and control measures [25].
Adding to this, it can be extracted from the literature review that of the 66 patients admitted to the Intensive Care Unit with a positive diagnosis for Covid-19, 88% were treated with invasive mechanical ventilation from March 11 to 30, 2020. 56 patients met the criteria for SARS, according to the study by Ziehr, et al. [26]. Also in this regard, the authors understand that the starting point of the initial global sample was 31 patients with a PaO2/FiO2 ratio ≤ 150 in the supine position, who were submitted to a protocol switching this position to prone every 72 hours. As a complement to the data obtained, it was observed that the position in pronation highlighted by the authors was for an average period of 18 hours in two sessions. They draw attention to the PaO2/FiO2 protocol ratio, giving strong margins for reflection and empiricity in the non-invasive respiratory treatment. The authors even make a biblical metaphor, considering that each Goliath needs a David, indicating that each problem requires a specific solution, not admitting single paths for a pandemic still under study. In the sample obtained by the authors, the previously indicated relationship required the supine position, maintaining significant results in 217 patients.
Contributing to this, a more cautious look at this discussion concerns a new research carried out by Roesthuis, et al. [18] with fourteen patients, eight men and six women, in which respiratory mechanics was evaluated indicating lower than normal lung compliance and comparing to patients with SARS, due to Covid-19. The pulmonary compliance of these patients was very low, but for those in the prone position, it was slightly lower than normal, which allows us to intertwine the information collected in the different studies analyzed in this integrative review. Even in need of further elaboration, these authors, in their study that reflects the advanced respiratory monitoring in patients with Covid-19, using high levels of positive end-expiratory pressure (PEEP), aiming to reduce injuries caused by mechanical ventilators, found that PP patients responded well, and this was due to better blood flow redistribution.
In order to reinforce the findings found, a meta-analysis that used 2,000 patients with SARS mechanically ventilated for at least 12 hours did not detect any effect on mortality when using the prone position. However, PP played an important role in SARS to redistribute pulmonary blood flow, and it is at this point that it is necessary to reinforce common links between the material obtained for this analysis, which can be considered an important pillar within respiratory physiotherapy. As a complement to this question, Robba, et al. [20], in their reference study, emphatically question the feasibility and efficacy of prolonged ventilation in the prone position for patients with Covid-19. In this study, the author and other researchers observed that the reduction of atelectasis improved oxygenation, giving rise to the outstanding relevance of the maneuver to be performed by a team trained to avoid risks in accidental extubation, among other things, reducing the possibility of infections.
It was reported in the case report of a 70-year-old patient, without previous diseases, intubated with SARS, secondary to Covid-19, that PP was instituted due to severe hypoxemia, with PaO2/FIO2 ≤ 118. After an hour in this decubitus and without changes in the ventilator parameters, the ratio rose to 263. Comparing this to the other data, it can be stated that there is connectivity between the investigations added here and compared [27].
In this sense, Carsetti, et al. [21], in a study carried out with ten SARS patients, all intubated, six of them were submitted to standard position and PP, three to PP and one only standard. The authors claim that it is safe to perform the maneuver in these patients with SARS secondary to Covid-19 and severe hypoxemia unresponsive to conventional mechanical ventilation. The authors highlighted that the prone position favors the improvement of oxygenation, and also suggest that prolonged PP of 36 hours is an operational strategy with important clinical and organizational advantages [21].
In this regard, Moghadam, et al. [28] state that the prone position was adopted in ten patients admitted to the ward, without mechanical ventilation, with a diagnosis of Covid-19 and a mean saturation of 85.6% and complaint of dyspnea, after which the adoption of the prone position, the saturation increased to 95.9% and the complaint decreased [28]. Concomitantly, Barker, et al. [29] verified in their study the relationship between intubated and non-intubated patients in terms of the prone position in CPR (cardiorespiratory resuscitation) orientation. For the authors, PP is an established and evidence-based method used in patients with SARS, with the main characteristic of coronavirus-2019 (Covid-19) being acute lung injury in patients, being recommended by intensive care in the United Kingdom.
What is observed in these surveys can be reinforced with the results of the report by Wuhan (2020) [30]. In his editorial, the author offers a comparative table, bringing a view of his experience in admissions made to the Intensive Care Unit in 2009, caused by the Influenza A (H1N1) virus and by SARS-CoV-2 (pneumonia) of 2019. In the table, it is possible to see that of the 37 ventilated patients, only 10.8% were alive and not mechanically ventilated 28 days after admission to the ICU. As for Influenza, the table highlights that the 28-day survival rate was more than doubled. In the same document, of the 52 patients with pneumonia caused by SARS-CoV-2, six on mechanical ventilation used the prone position, and for those with Influenza A (H1N1), of the 32 admitted, eight used the PP38. Comparing with the study by Relloa, et al. [31], there are clear indications that the path adopted deserves to be taken into account. What can be highlighted is a movement of continuity among those who defend the studied authors, sometimes showing that the central argument is reinforced in light of the research carried out and here compared and added.
PP is a strategy in ventilatory support used in patients with a PaO2/FiO2 ratio ≤ 150 mmHg, which characterizes the patient in severe hypoxemia. This decubitus improves oxygenation, the ventilation-perfusion ratio and makes the distribution of ventilation more uniform through lung recruitment and changes in the elasticity of the chest wall, and its use is recommended for a period > 12 hours a day [32]. In contrast to this, Lazzeri, et al. [17], in an academic study on the opinion of the Italian Association for Respiratory Physiotherapy in Patients with Covid-19 in Acute Condition, state that PP is recommended for 12 to 16 hours a day, preferably within 72 hours after endotracheal intubation, and may be repeated until a PaO2/FiO2 (P/F) ratio ≥ 150 mmHg with PEEP ≤ 10 cmH2O and FiO2 ≤ 0.60 for at least 4 hours after the supine position is obtained. This must be carried out by qualified staff.
Complementarily, Matthay, et al. [33], in a basic study that indicated treatments for Covid-19 acute and severe respiratory distress, observed that for patients with SARS secondary to Covid-19 undergoing endotracheal treatment with orotracheal intubation (IOT) the protective MV strategy with low Tidal Volume (VT) of 6 mL/kg per kilogram of predicted body weight was recommended, with plateau pressure less than 30 cmH2O, respiratory rate up to 35 breaths per minute (rpm). In the research by Matthay, et al. [33] it was also possible to verify that in a V/Q ratio of 100-150 mmHg, the expiratory pressure can be increased by 2-3 cmH2O every 15-30 minutes to raise the saturation between 88-90%, maintain a plateau pressure of less than 30 cmH2O and associate the position in pronation, when there is no contraindication.
In turn, Pérez-Nieto, et al. [34], in an important study on prone positioning combined with a high-flow nasal cannula, indicated that in patients with severe hypoxemia, PP is associated with a decrease in mortality, corroborating what Guérin, et al. [35], in a study on the use of pronation positioning in Severe Acute Respiratory Distress Syndrome (SARAG), already highlighted for almost a decade. For both, SARS treatment using PP is recommended for at least 16 hours/day and should be used when there is a V/Q ratio ≤ 150 mmHg [28]. What is observed is that the combination of the use of high flow and PP demonstrates that, in healthy individuals, there is a homogeneous distribution of expiratory pulmonary impedance due to improved oxygenation.
In addition, Wincka and Ambrosino [16], in a study with 29 patients with hypoxemic respiratory failure, breathing in room air, after PP, highlighted that there was an improvement in the PaO2/FiO2 ratio. PP associated with high flow or non-invasive mechanical ventilation (NIMV) avoided the need for orotracheal intubation in more than half of SARS patients, including those with viral pneumonia. Experiments suggest that early intervention with high flow and NIMV associated or not with PP can reduce mortality.
Based on the studies mentioned, hypotheses can be raised about the impacts on the relationship between the recommendation of time in the prone position combined with other ventilatory strategies, providing similar and comparable results within the highlighted situational universe. The theoretical discussion evidenced this at first, making room for verifications that crossed the relationship between time and other associated methods, making it possible to verify the physiological effects of the prone position in greater detail below.
PP improves oxygenation, compliance, increases pulmonary homogeneity, improves blood flow redistribution, nullifies the action of gravity, and when applied for a prolonged period (≥ 16 h) in patients with severe hypoxemic disorder and ventilation-perfusion with PaO2/FiO2 ≤ 150, is effective [18,24,36]. In order to reinforce the issue, the Brazilian Society of Anesthesiology [37] recommends the adoption of the prone position in patients with SARS due to the fact that the decubitus favors the improvement of the ventilation-perfusion relationship, to recruit gravity-dependent regions, optimizing the mechanical properties of the thorax and favoring the drainage of secretions from the bronchial tree [28,38-42].
Practice based on scientific evidence ensures quality care and offers subsidies that provide knowledge and update. In view of this need, the integrative review pointed out grounded scientific knowledge, synthesizing the research available during the search period.
Although PP has been elucidated since 2008, with the pandemic this became more evident and showed that it is effective in improving the oxygenation of patients with a PaO2/FiO2 ratio ≤ 150 mmHg, and safe to be applied, as long as the institution trains and qualifies the team involved in the maneuver process, with strict controls and monitoring of possible complications.
In addition to these recommendations, studies show that there is a need for the maneuver to be applied for at least 12 hours in a period of 72 consecutive hours. They also point out the importance of being associated with other maneuvers, such as protective mechanical ventilation with low Tidal Volume (VT) of 6 mL/kg of predicted body weight, a plateau pressure of less than 30 cmH2O, respiratory rate of up to 35 breaths per minute (rpm).
They also suggest that in a ventilation-perfusion ratio of 100-150 mmHg, it is necessary to increase the expiratory pressure by 2-3 cmH2O every 15-30 minutes to raise the saturation between 88-90% and maintain a plateau pressure of less than 30 cmH2O.
However, given the above and although the evidence points to the efficacy and safety of this maneuver in patients with SARS secondary to Covid-19, increasing the PaO2/FiO2 ratio, further research is required, with a field study, especially in light of the current scenario, seeking to ensure greater safety for patients, more efficiency, in addition to more precisely elucidating the pathophysiology of PP, as some studies indicate that it is not yet fully clarified and that there is a need to establish criteria for the case of an arrest cardiorespiratory action during the maneuver or other complications.