Atelectasis is a common problem in the critical care setting and when it causes acute life-threatening hypoxemia it is necessary its re-expansion. Ultrasonography is capable to diagnose atelectasis at the bedside and accurately assesses lung aeration changes after reexpansion maneuver. We describe a case in which a male patient receiving mechanical ventilation developed acute hypoxemia due atelectasis, being applied recruitment maneuver guided by ultrasonography combined with lateral decubitus positioning to reexpansion of collapsed region.
The loss partial or total of lung volume is named atelectasis. In the critical care setting, atelectasis is a common problem and when it causes acute life-threatening hypoxemia it is necessary its re-expansion.
Ultrasonography is capable to diagnose atelectasis at the bedside. This condition appears sonographically as a subpleural echo-poor region or one with tissue-like echotexture [1]. Additional sonographic signs may help to differentiate this one from other causes of lung consolidation such as abolition of lung sliding with a lung pulse, and static air bronchogram. The dynamic demonstration of the absence of lung expansion is the advantage of lung ultrasound in comparison with radiography and computed tomography [2]. In addition to its role in the diagnosis, lung ultrasound accurately assesses lung aeration changes following positive end-expiratory pressure (PEEP) [3].
In this case, acute hypoxemia occurred in patient admitted to intensive care unit (ICU) due to coronavirus disease and receiving mechanical ventilation. Bedside lung ultrasonography was very useful to obtain the diagnosis, to evaluate the patient response to therapy and to guide fine-tune the ventilator.
A 56-year-old male patient with history of epilepsy was admitted to the ICU due to severe pneumonia resulting from infection with the SARS-CoV-2 coronavirus. He evolved with acute hypoxemic respiratory failure and was intubated 2 days after his admission.
After 12 days of mechanical ventilation, he had a sudden drop in peripheral arterial oxygen saturation. The patient was sedated, well adapted to the ventilator and hemodynamically stable. Blood gas analysis revealed PaO2/FiO2 ratio of 140. A chest X-ray was performed which showed opacification of the left hemithorax with erasure of the contours of the cardiac area and the left phrenic dome.
Thoracic ultrasound was performed at the bedside and visualized volumetric reduction of the pulmonary segment above left diaphragm and the presence of tissue pattern with hyperechoic punctiform images and no change in its characteristics during respiratory incursions, besides abolished lung sliding and cardiac vibrations visible at the pleural line, corresponding to a left lower lobe atelectasis. Arterial vessels within consolidations were visualized by means Color Doppler ultrasound indicanting intrapulmonary shunt.
We decided to adopt Open Lung Approach strategy guided by ultrasonography combined with lateral decubitus positioning (affected lung positioned superiorly) to re-expansion of collapsed region.
After bolus dose of cisatracurium, PEEP was increased from 8 to 20 cmH2O. A curvilinear probe located at posterior axillary line showed the disappearance of the tissue-like pattern and the appearance of lung sliding with A lines indicating reversal of atelectasis (Figure 1). This PEEP level was maintained for 4 minutes and no hemodynamic instability occurred during this recruitment phase.
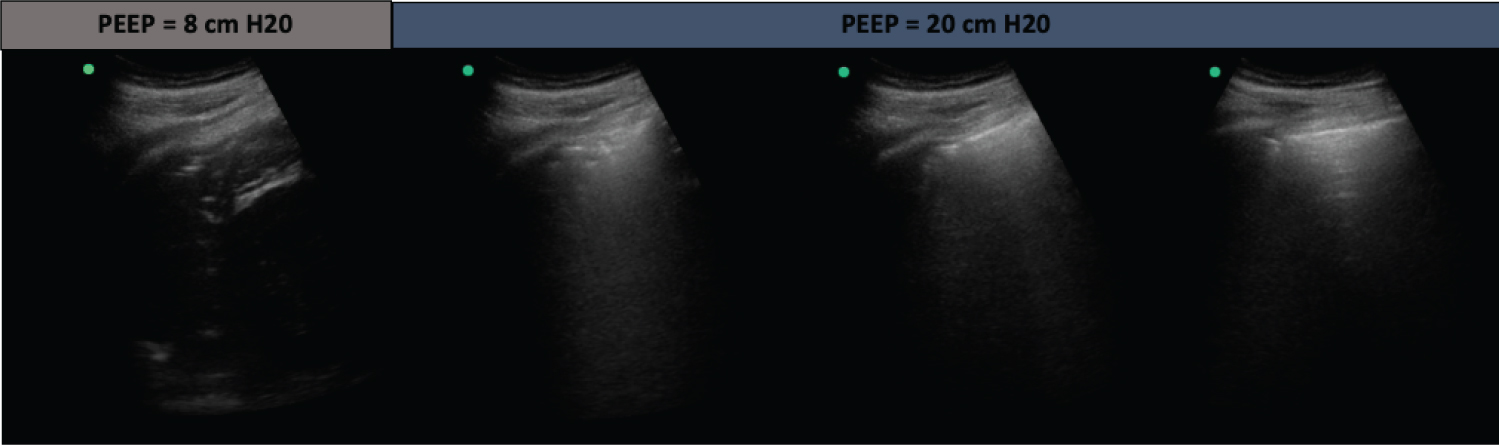 Figure 1: Lung ultrasound images of recruitment maneuver. After increase of PEEP from 8 to 20 cm H2O, the tissue-like pattern disappears and progressive lung reaeration is observed. Reaeration follows the sequential pattern: Consolidation (complete de-aeration) → B lines (penetration of gas within the lung region) → normal lung image (normal aeration).
View Figure 1
Figure 1: Lung ultrasound images of recruitment maneuver. After increase of PEEP from 8 to 20 cm H2O, the tissue-like pattern disappears and progressive lung reaeration is observed. Reaeration follows the sequential pattern: Consolidation (complete de-aeration) → B lines (penetration of gas within the lung region) → normal lung image (normal aeration).
View Figure 1
Once the reaeration has been achieved, decremental PEEP titration was performed that consisted of decrease of PEEP from 20 to 10 cmH2O in 2 cmH2O steps each one lasting two minutes (Figure 2). The PEEP of 12 cmH2O was chosen because it preserved normal lung aeration, in addition to generation greater compliance of the respiratory system and lower driving pressure.
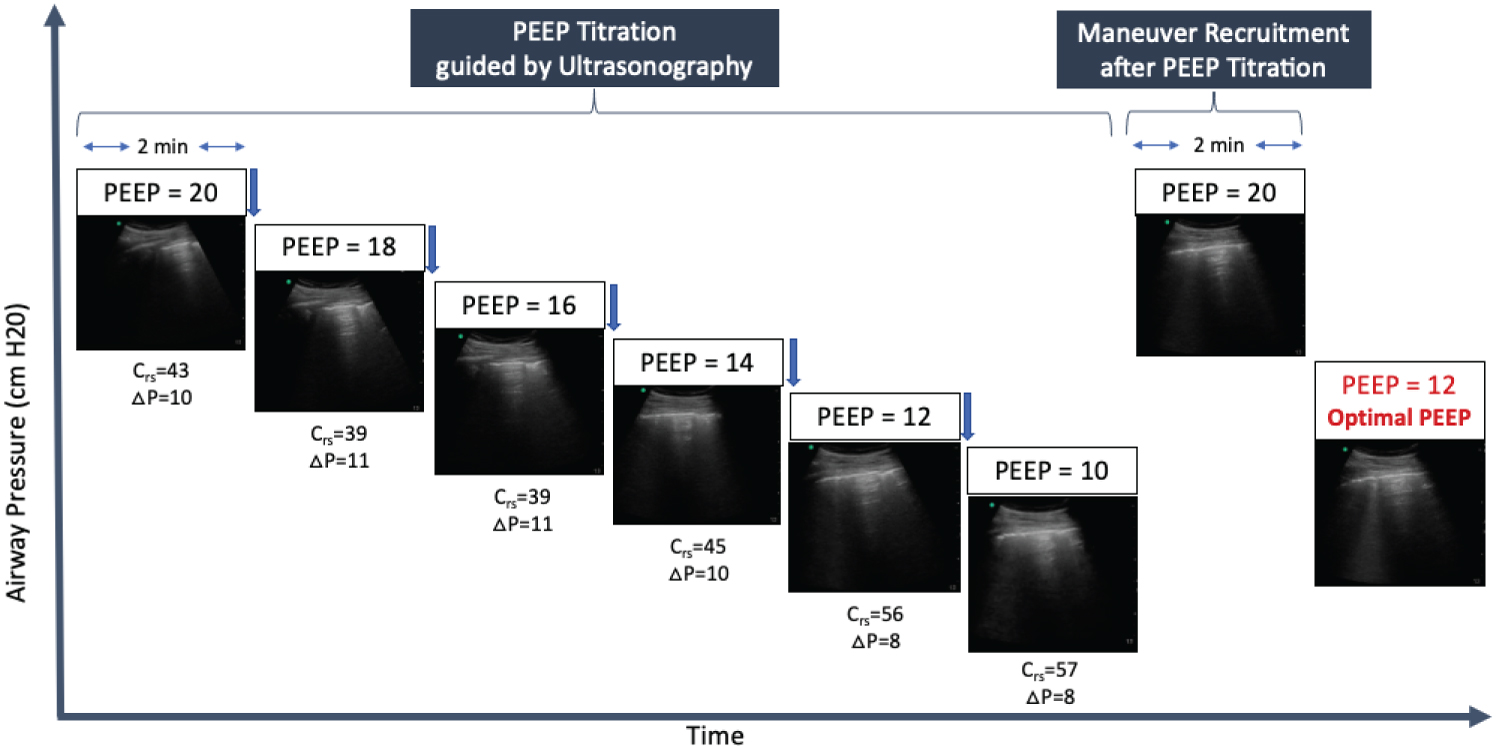 Figure 2: Lung ultrasound images of PEEP titration. PEEP was decreased from 20 to 10 cmH2O in cmH2O steps each one lasting two minutes. Optimal PEEP is the minimum PEEP level associated with normal lung aeration, best compliance of respiratory system (Crs) and lower driving pressure (ΔP). A new recruitment maneuver was performed after an optimal PEEP is identified.
View Figure 2
Figure 2: Lung ultrasound images of PEEP titration. PEEP was decreased from 20 to 10 cmH2O in cmH2O steps each one lasting two minutes. Optimal PEEP is the minimum PEEP level associated with normal lung aeration, best compliance of respiratory system (Crs) and lower driving pressure (ΔP). A new recruitment maneuver was performed after an optimal PEEP is identified.
View Figure 2
After lung recruitment and PEEP titration, the PaO2/FiO2 ratio increased to 190 and a new chest radiograph showed evident pulmonary reexpansion (Figure 3).
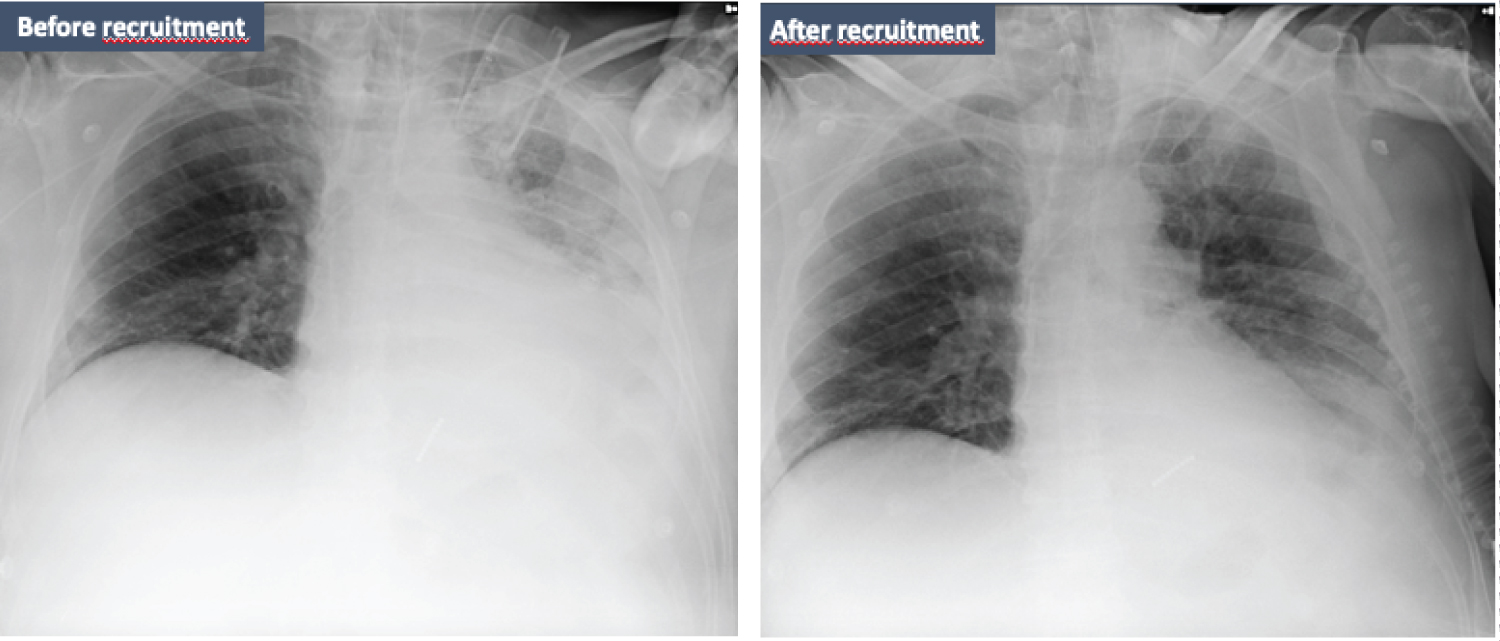 Figure 3: Representative chest radiographs that show the evolution of the case. Initially, chest radiography revealed opacification of the lower half of the left lung fields with mild homolateral mediastinal displacement. After recruitment maneuver guided by ultrasonography during lateral decubitus, the pulmonary reexpansion is evident.
View Figure 3
Figure 3: Representative chest radiographs that show the evolution of the case. Initially, chest radiography revealed opacification of the lower half of the left lung fields with mild homolateral mediastinal displacement. After recruitment maneuver guided by ultrasonography during lateral decubitus, the pulmonary reexpansion is evident.
View Figure 3
On the 17th day of mechanical ventilation, the patient was extubated, and he was discharged from the hospital 40 days after admission.
Acute hypoxemia during mechanical ventilation is a result of the mismatch between ventilation and perfusion [4] and atelectasis is a common cause of acute hypoxemia in the setting of critical care [5]. Atelectasis is defined as collapse of alveoli with loss of aeration [6]. The pathophysiological effects of loss of lung volume are decreased compliance, impaired gas exchange and increased pulmonary vascular resistance [7]. In addition, atelectasis may be associated with activation of lung inflammation [8,9] and with increase of strain and stress aggravating or generating lung injury [6].
Ventilatory support in unilateral lung injury, as atelectasis, is a special challenge. It should improve lung aeration and reorient blood flow without overdistending contralateral lung. A ventilatory strategy to be applied in this scenario is to position the patient with the “good lung down” and to perform alveolar recruitment aiming pulmonary re-expansion [10].
In patients with unilateral lung injury that were turned from a supine to a lateral decubitus position with the injured lung in the nondependent position, gas exchange improves because of changes in the patterns of ventilation-perfusion distribution [11]. As pulmonary blood flow is almost entirely determined by the forces of gravity [12], the redistribution of blood flow to the healthy dependent lung result in a better V/Q. A potential complication of lateral positioning is the de-recruitment of the dependent lung due to lung and heart weight [13]. Other possible complication of lateral decubitus is the hyperinflation of injured lung, specifically atelectatic lung, in the nondependent position as consequence of gravitationally drived distribution of ventilation.
The lung with atelectasis is less compliant and behaves like a solid resisting a deformation. The role of lung recruitment can promote a homogeneous distribution of tidal ventilation [14] and should set adequate PEEP to maintain open lung and avoiding cyclic collapse. The use of ultrasound can help to identify improvement in lung aeration during lung recruitment maneuver and PEEP titration [4]. As lung density increases lung aeration decreases and vice-versa. There is re-opening of nonaerated lung region after applying PEEP when the ultrasound tissue pattern characteristic of lung consolidation is replaced by the visualization of the pleural line with preserved lung sliding and presence of horizontal A-line.
Once there was a positive response to the alveolar recruitment maneuver, next step is to identify PEEP level capable of avoiding new collapse. During this phase of decremental PEEP titration, the probe is kept in the same position as before and the reduction of PEEP is interrupted when normal lung aeration images transform into a B1-B2 pattern and consolidation pattern [15].
Although the ultrasonography allow to personalize the maneuver recruitment and the PEEP titration, this tool cannot detect over distension resulting from an increase in intrathoracic pressures [16]. At the bedside, the compliance of the respiratory system (Crs) helps to monitor the overinflation because Crs is directly related to the size of the lung participating in ventilation [17], i.e., Crs tends to increase with recruitment but decreases once over-inflation begins.
Lung ultrasound is an image method that can be used to individualize ventilatory management of unilateral lung injury because it allows to monitor lung aeration changes following applying PEEP.
Not applicable.
RSN, VBS and LCPB contributed to the case. RSN, GCTA and KGI contributed to discussion, general review, editing and figure generation. All authors read and approved the final manuscript.
No funding was received for this case series.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The patients consented to participate in the case report.