Acute chest pain, Esophageal perforation, Boerhaave syndrome
Chest pain is one of the most common symptoms for which adults seek medical care, making chest pain the second most common complaint [1]. A central goal in the emergency department is to determine whether acute chest pain is a life-threatening condition for the patient [1,2]. Acute onset of chest may also be seen with disorders such as aortic aneurysm dissection, myocardial infarction, spontaneous pneumothorax, pneumonia, pancreatitis, peptic ulcer perforation, or esophageal perforation [2].
A male ages 40-50 years-old presented to the emergency department with chest pain with radiation for upper abdominal and left flank. As a personal history, of anxiety, in treatment with diazepam and duloxetine. There is no previous relevant history of gastrointestinal disease, and he did not have any preexisting disease and allergic history. His symptoms began suddenly after vomiting and he complained an intense pain (the pain score was 9 out of 10 based on the verbal rating scale). He also reported nausea, diaphoresis, and had no symptoms of severe acute respiratory syndrome. On admission, physical examination showed pale and sweaty skin, his initial vital signs were a blood pressure of 112/73 mmHg, heart rate of 135 beats per minute, respiratory rate of 25 breaths per minute, temperature of 36.2 °C, oxygen saturation 98% on room air. During the initial clinical examination, he was pale and sweaty and very complaining in the retrosternal and left lumbar region. Apart from the above signs, he had no other remarkable findings on systemic examination. A metabolic acidosis with high anion gap (pH 7.37, pCO 2 29 mmHg, pO 2 102 mmHg, bicarbonate 16.8 mmol/L, saturation 98.7%, anion gap of 14 mEq/L, lactate 1.4 mmol/L) was present on his initial blood gas. The initial chest X-ray showed no acute abnormalities Figure 1, most notably no pneumothorax or pneumomediastinum and 12-lead electrocardiogram showed a normal sinus rhythm. The patient's laboratory studies revealed a mild leukocytosis (14 10^3/uL) and C-reactive protein was below 1 mg/L. His renal and electrolyte profile was normal (creatinine of 1.5 mg/dl). There was no abnormal finding by the levels of cardiac biomarkers, pancreatic lipase and amylase, or D-dimer. To clarify the clinical case, a CT was performed, which showed left pneumothorax, anterior pneumomediastinum and indistinct esophageal wall with pneumomediastinum at just above the gastro-oesophageal junction, suggestive of esophageal rupture Figure 2 and Figure 3. General surgery was consulted and due to history of the present illness two sets of blood culture were collected and broad-spectrum antibiotics and antifungals with piperacillin/tazobactam and fluconazole were initiated, as well as analgesia and prokinetics. Faced with the diagnosis of with esophageal rupture, the patient was transferred to a referral center and submitted to surgical repair with placement of an esophageal prosthesis with clinical improvement. He was discharged home on the 12 th postoperative day. After one month’s follow-up consultation, the patient is well with no impairments.
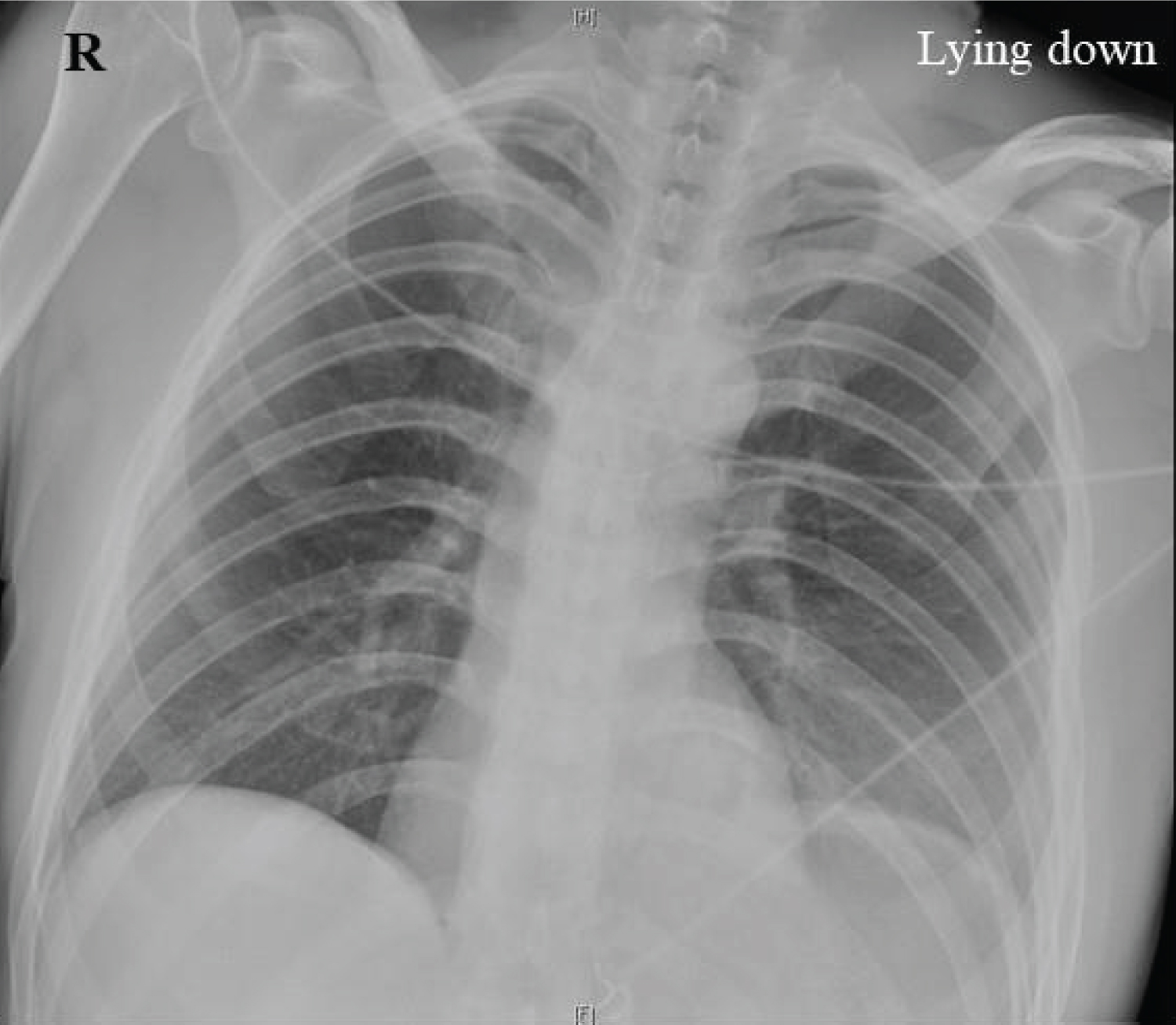 Figure 1: Frontal chest radiograph.
View Figure 1
Figure 1: Frontal chest radiograph.
View Figure 1
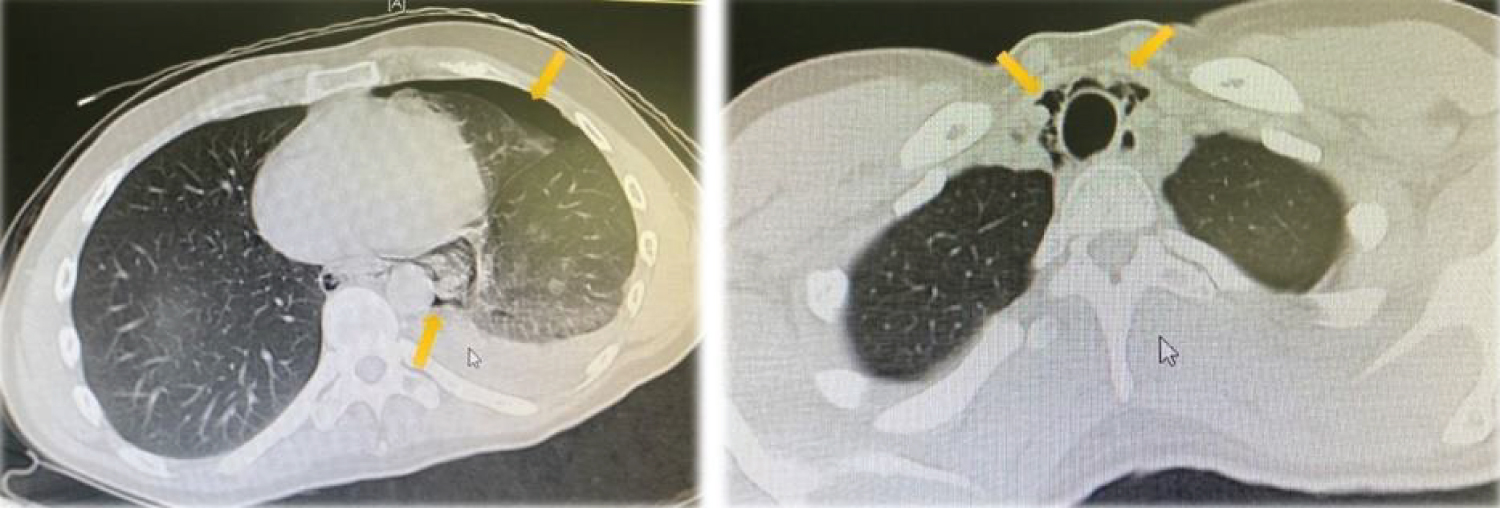 Figure 2: Axial view of CT chest with evidence of left pneumothorax and pneumomediastinum (yellow arrows).
View Figure 2
Figure 2: Axial view of CT chest with evidence of left pneumothorax and pneumomediastinum (yellow arrows).
View Figure 2
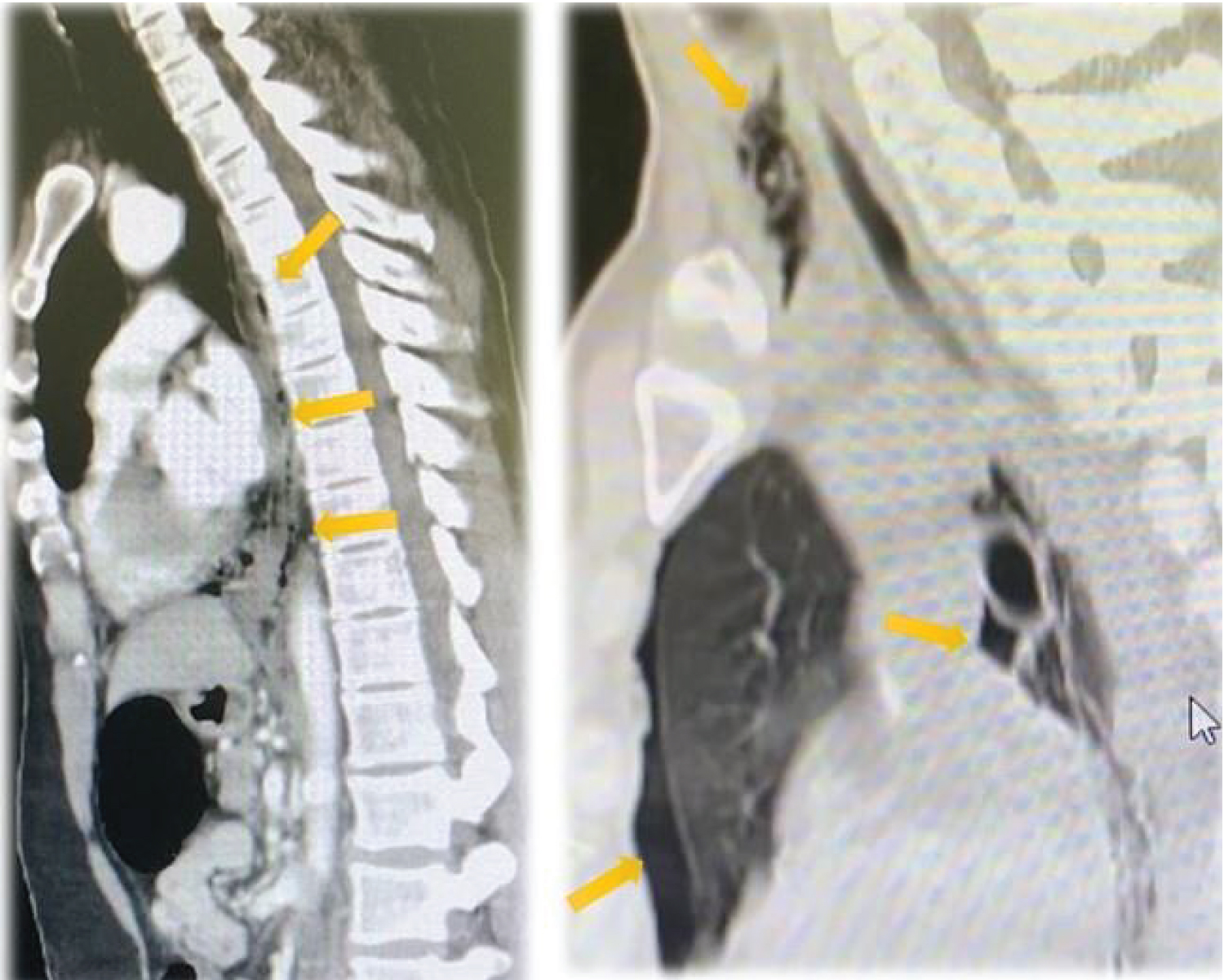 Figure 3: Sagittal view of CT chest showed extra-luminal free air in the mediastinum (yellow arrows) and left-sided pneumothorax.
View Figure 3
Figure 3: Sagittal view of CT chest showed extra-luminal free air in the mediastinum (yellow arrows) and left-sided pneumothorax.
View Figure 3
Spontaneous esophageal rupture occurs from a sudden increase in intraluminal pressure due to violent vomiting or retching [3]. The perforation is usually in the distal esophagus on the left side and is known for a high mortality rate of up to 40% [3]. Patients often present with excruciating retrosternal chest pain due to an intrathoracic esophageal perforation following forceful vomiting [4]. The classic Mackler triad of chest pain, vomiting, and subcutaneous emphysema is present in about 5% of case and the physical findings are usually nonspecific [4]. Physical exam findings may include abnormal vitals (diaphoresis, tachycardia, tachypnea, fever), decreased breath sounds on the perforated side, mediastinal emphysema, and Hamman's sign (mediastinal “crackling” accompanying every heartbeat) in left lateral decubitus position [5]. Laboratory tests provide little help in the diagnosis; however, they can exclude more common conditions in the differential diagnosis, including pancreatitis, myocardial infarction, and aortic aneurysm dissection [6]. On the other hand, imaging is of high importance in diagnosing Boerhaave syndrome. Chest radiography could show a pleural effusion (left more common than right), pneumothorax, pneumomediastinum, pneumoperitoneum, or subcutaneous air, although a normal radiograph cannot exclude esophageal rupture [6]. Therefore, a high index of suspicion is required to make a timely diagnosis and ensure rapid imaging to guide further interventions.
The authors have no potential conflicts to disclose.
All the authors made a substantial contribution to the manuscript.