58-year-old male sustained sudden cardiac arrest (SCA) due to ventricular fibrillation (VF) while at work and was resuscitated with shock therapy. He had prior history of coronary artery disease with bypass, preexcitation, pulmonary hypertension, hyperlipidemia, Hodgkin's disease, hypothyroidism and squamous cell carcinoma. His EKG showed preexcitation. Echocardiogram showed moderately reduced left ventricular ejection fraction (LVEF) of 37% along with severe aortic valve stenosis (AS) with calculated valve area of 0.66 cm2, mean gradient of 6.9 mmHg and peak AV velocity of 2.09 m/s. This was consistent with low output low gradient aortic stenosis. Patient underwent coronary angiogram that revealed no acute occlusion.
Cardiac CT showed porcelain aorta with close proximity of LIMA to aorta and sternum. Patient underwent dual-chamber implantable cardioverter defibrillator (ICD) placement for secondary prevention. During the procedure patient was noted to have one-to-one AV conduction with continued preexcitation with atrial pacing up to 180 bpm. He was treated with amiodarone and underwent transcatheter aortic valve replacement (TAVR).
Sudden cardiac arrest, Aortic stenosis, Preexcitation
SCA: Sudden Cardiac Arrest; VF: Ventricular Fibrillation; LVEF: Left Ventricular Ejection Fraction; AS: Aortic Valve Stenosis; ICD: Implantable Cardioverter Defibrillator; TAVR: Transcatheter Aortic Valve Replacement; LIMA: Left Internal Mammary Artery
Aortic stenosis as well as preexcitation can lead to sudden cardiac arrest. This is a unique case of a 58-year-old man who presented with sudden cardiac arrest in the presence of both severe aortic stenosis as well as preexcitation.
A 58-year-old male collapsed suddenly while working at the baggage line in the airport. Initial rhythm was ventricular fibrillation and 2 shocks were delivered at the site with return of spontaneous circulation. He was given amiodarone and was brought to the hospital.
Patient had history of coronary artery disease along with coronary artery bypass grafting, preexcitation, pulmonary hypertension, hyperlipidemia, Hodgkin's disease treated with chemotherapy as well as radiation, hypothyroidism and squamous cell skin cancer that was resected. There was no family history of sudden cardiac death or any other significant cardiac disease. Patient worked as an airline baggage handler and did not have any prior history of tobacco or alcohol use.
He was on aspirin 81 mg daily, metoprolol tartrate 50 mg twice a day, simvastatin 20 mg daily, ranolazine 1000 mg daily, furosemide 20 mg daily, potassium chloride 20 mEq daily and levothyroxine 100 mcg daily.
At the time of presentation to the hospital, his vital signs were stable. His cardiovascular examination revealed 1/6 systolic ejection murmur in right upper sternal border.
Basic metabolic profile as well as complete blood count did not reveal any significant abnormalities. Troponins were negative.
EKG at the time of presentation showed sinus rhythm with no significant ischemic changes (Figure 1A). On day 2 of admission, ECG was repeated that showed sinus rhythm with presence of preexcitation (Figure 1B).
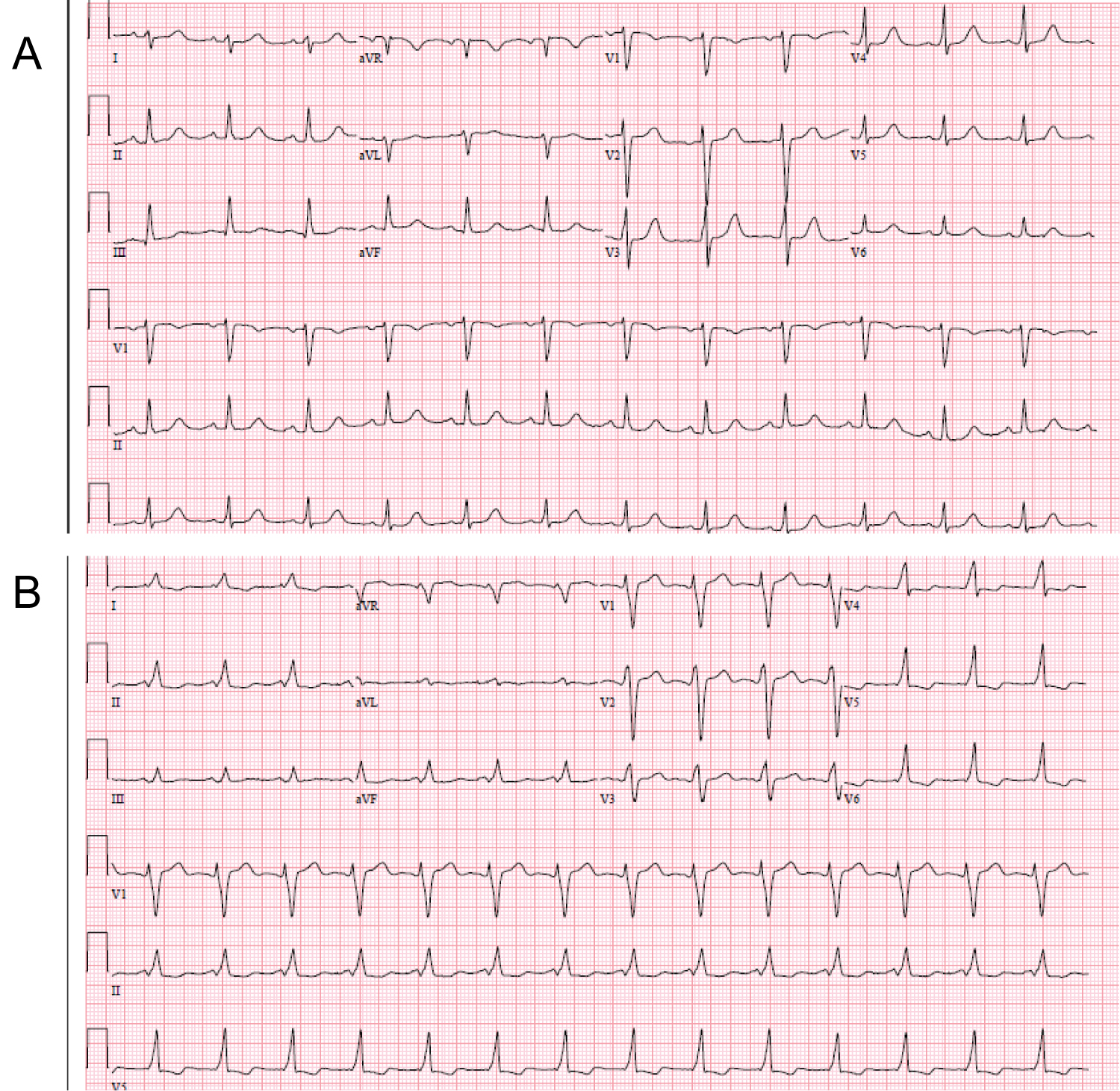 Figure 1: A) Baseline ECG at the time of presentation; B) ECG on day 2 showing preexcitation.
View Figure 1
Figure 1: A) Baseline ECG at the time of presentation; B) ECG on day 2 showing preexcitation.
View Figure 1
Echocardiogram showed global hypokinesis with moderately reduced LVEF of 37% along with stage II diastolic dysfunction. Patient was noted to have thickened calcified aortic valve and severe AS with calculated aortic valve area of 0.66 cm2, mean aortic valve gradient of 6.9 mmHg and peak velocity across aortic valve of 2.09 m/s. He was noted to have mitral annular calcification with thickened mitral valve without stenosis and mild mitral regurgitation. Patient was taken for cardiac catheterization that revealed severe native three-vessel disease, two patent grafts from left internal mammary artery (LIMA) to left anterior descending artery and saphenous venous graft to right coronary artery. Saphenous venous graft to left circumflex was completed occluded at the origin.
The two major differentials of sudden cardiac death after the above investigations were severe aortic stenosis and WPW syndrome.
After a multidisciplinary case conference, it was recommended that patient should undergo aortic valve replacement. Patient underwent cardiac CT that showed near porcelain ascending aorta (Figure 2). It also revealed close proximity of LIMA to aorta and sternum. Treatment options for this patient at this time were either TAVR vs. apical aortic conduit placement. Patient underwent implantation of dual-chamber ICD for secondary prophylaxis of sudden cardiac death. During this procedure, atrial pacing was performed up to 180 bpm that showed one to one AV conduction with continued preexcitation. Patient was started on amiodarone to avoid recurrence of ventricular arrhythmias. Thereafter, he underwent TAVR with 26 mm sapient transcatheter aortic valve.
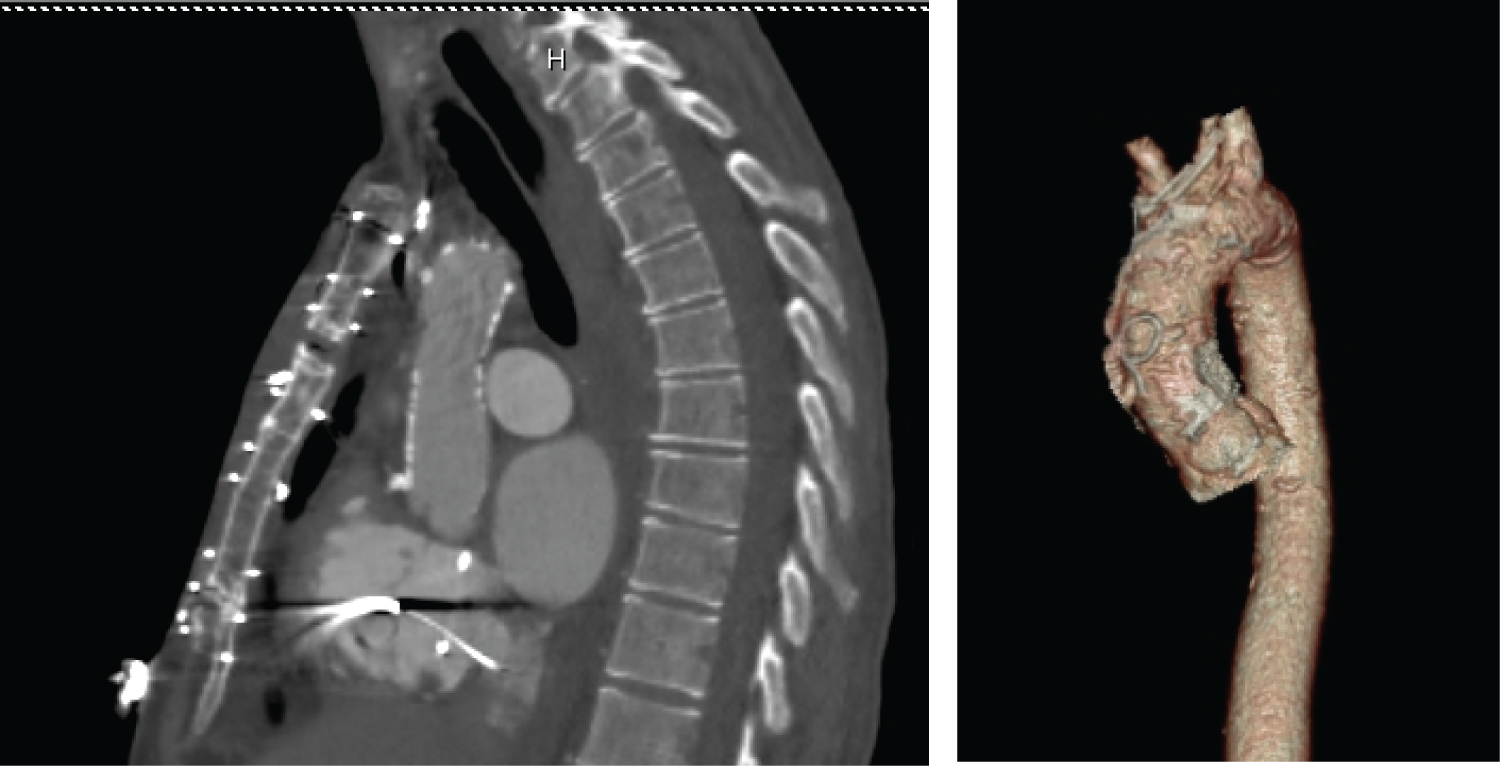 Figure 2: Cardiac CT demonstrating near porcelain aorta.
View Figure 2
Figure 2: Cardiac CT demonstrating near porcelain aorta.
View Figure 2
Patient had a prolonged hospitalization for almost a month after TAVR. He had recurrent pleural effusions requiring chest tube placement. He was noted to have a few episodes of non-sustained ventricular tachycardia and was maintained on amiodarone. He continued to struggle with heart failure and underwent mitral valve replacement after 2 months of previous hospitalization.
One year after his initial presentation, patient experienced erosion of ICD and underwent extraction of the device. He was discharged with a LifeVest and was brought after a month for implantation of another ICD with single right ventricular lead placement through right subclavian approach. The lead was tunneled through the chest wall and the defibrillator can was placed in the abdominal wall (Figure 3).
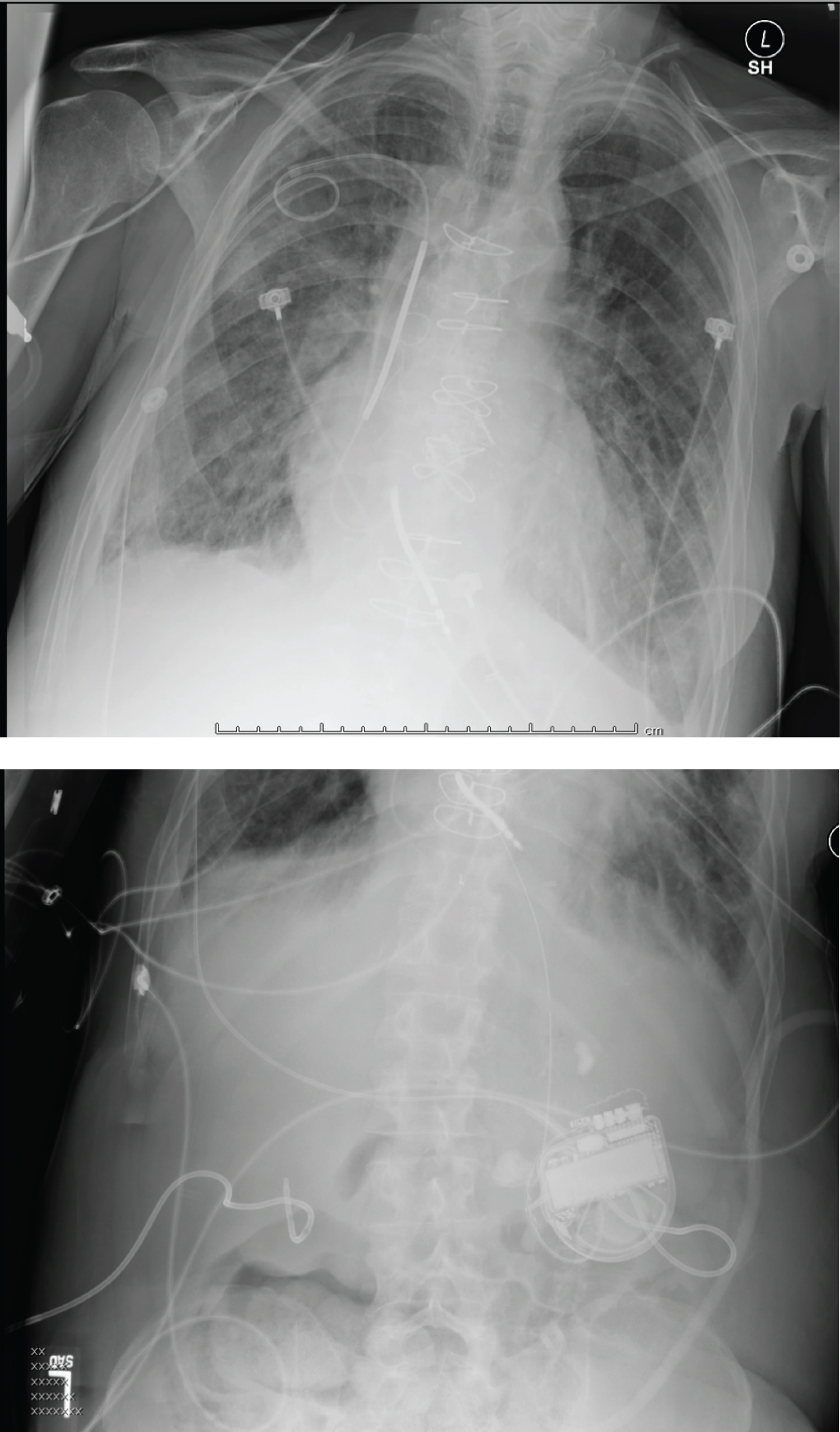 Figure 3: Right ventricular lead implanted through right subclavian approach with generator in abdominal cavity.
View Figure 3
Figure 3: Right ventricular lead implanted through right subclavian approach with generator in abdominal cavity.
View Figure 3
After 4-1/2 years of follow-up, patient developed metastatic bladder cancer and passed away with multiorgan failure. During this time, he did not have any sustained ventricular arrhythmias or received ICD shocks. No ablation was performed for his accessory bypass tract as there was no recurrence of ventricular arrhythmia.
Sudden cardiac death is defined as sudden unexpected death either within 1 hour of symptom onset (event witnessed) or within 24 hours of having been observed alive and symptom-free (unwitnessed). Sudden cardiac death accounts for 5.6% of annual mortality [1].
Major causes of sudden cardiac death among all ages in order of incidence are coronary artery disease, congestive heart failure/cardiomyopathy, aortic stenosis, congenital heart disease and seizure disorder.
In our case, underlying cause of ventricular fibrillation could have been aortic stenosis or WPW syndrome.
Incidence of sudden cardiac death and aortic stenosis varies from 0 to 5% in asymptomatic patients and 8 to 34% in symptomatic patients [2].
Pellika, et al. studied 622 patients with isolated asymptomatic aortic stenosis with peak systolic velocity of greater than equal to 4 m/s that did not undergo surgery at the initial evaluation. They followed these patients with a mean follow-up of 5.4 years ± 4 years. 57% of the patients were referred for aortic valve surgery. Sudden death without preceding symptoms occurred in 11 (4.1%) of 270 unoperated patients. They concluded that sudden death occurs in approximately 1 %/year of asymptomatic patients with severe aortic stenosis [3].
The underlying mechanism of sudden cardiac death and aortic stenosis are following: 1) Abnormal Bezold-Jarisch reflex: Aortic stenosis leads to activation of left ventricular baroreceptors that cause hypotension and bradycardia leading to sudden cardiac death. In addition, these factors also contribute to decrease coronary blood supply resulting in myocardial ischemia and further leading to malignant tachycardia and sudden cardiac death. 2) Left ventricular hypertrophy: This leads to increased myocardial oxygen consumption and reduced coronary blood flow reserve. 3) Atrioventricular conduction disturbances: This results from contiguity between valvular-perivalvular calcification in his-Purkinje system.
Mechanical explanation of ventricular arrhythmias and aortic stenosis: Aortic stenosis leads to systolic pressure overload which causes myocardial hypertrophy in leads to structural remodeling with increased collagen, abnormal electrophysiological properties, decreased myocardial perfusion due to reduced coronary vasodilator reserve further leading to myocardial ischemia, myocardial death and scar formation.
Electrophysiological mechanism of ventricular arrhythmia and aortic stenosis: This is resultant from reentry, stress-induced arrhythmia as well as triggered activity [4].
Our patient had low output low gradient aortic stenosis which is defined as aortic stenosis with calculated valve area of less than 1 cm2 and presence of left ventricular dysfunction with left ventricular ejection fraction of less than 40% along with low cardiac output and low transaortic mean gradient of less than 30 mmHg. Modified dobutamine stress test can help differentiate true aortic stenosis from severe aortic stenosis and is also a predictor of worse outcome if there is no change in cardiac output.
Rosenhek, et al. studied 128 consecutive patients with asymptomatic severe aortic stenosis and followed them over a mean. Of 22 ± 18 months. We found that moderate to severe valvular calcification and rapid increase in aortic jet velocity were poor prognostic indicators in these patients [5].
Sudden cardiac death in WPW syndrome occurs in setting of atrial fibrillation conducting through the accessory bypass tract leading to ventricular fibrillation. The risk of sudden cardiac death in symptomatic patients with WPW syndrome is estimated to be around 0.25%/year or 3 to 4% over her lifetime [6]. Factors that suggest an increased risk of sudden death in patients with WPW syndrome are minimal RR interval of less than 250 ms during atrial fibrillation, history of symptomatic tachycardia, multiple accessory pathways and Epstein anomaly [7]. Implantation of ICD is indicated for patients with cardiac arrest due to ventricular fibrillation or ventricular tachycardia not due to transient or reversible cause [8].
• Aortic stenosis is the third leading cause of sudden cardiac death.
• Incidence of sudden cardiac death in patients with asymptomatic aortic stenosis is 0 to 5%.
• Understanding mechanical and electrophysiological mechanism of ventricular arrhythmia in patients with aortic stenosis.
• The risk of sudden cardiac death (SCD) in symptomatic patients with WPW syndrome is estimated to be 0.25%/y or 3% to 4% over a lifetime
• Implantation of ICD is a Class I recommendations for patients with cardiac arrest due to ventricular fibrillation not due to transient or reversible cause.