Patients with symptomatic systolic anterior motion (SAM) of the mitral valve and left ventricular outflow tract obstruction (LVOTO) pose significant challenges in their management. This often occurs in a setting of hypertrophic cardiomyopathy (HCM), and occurrence of SAM without HCM is uncommon. In this report, we present a case of mitral valve SAM with sigmoid septum complicated by LVOT obstruction, as well as a concomitant left atrial myxoma, which was treated with an Alfieri procedure and myxoma excision with good results.
Myxoma, SAM, LVOT obstruction
Patients with SAM are usually asymptomatic till significant LVOT obstruction occurs, for which pharmacological agents such as beta-blockers, non-dihydropyridine calcium channel blockers or disopyramide can be given to reduce obstruction and relieve symptoms. In patients who do not respond to medical therapy, surgery such as septal myomectomy or alcohol ablation to reduce LVOT obstruction or mitral valve intervention to correct SAM are options in select patients. We present a case of mitral valve SAM with sigmoid septum complicated by LVOT obstruction, as well as a concomitant left atrial myxoma, which was treated with an Alfieri procedure and myxoma excision.
A 70-year-old Chinese female with underlying hypertension, hyperlipidemia and diabetes mellitus presented to the outpatient clinic with exertional dyspnoea. There was no family history of hypertrophic cardiomyopathy or sudden cardiac death. Physical examination revealed normal sinus rhythm with a systolic murmur. Transthoracic echocardiography showed a non-dilated left ventricle with a sigmoid septum (maximal thickness of 15 mm) (Figure 1). The left ventricular ejection fraction was 60%. There was SAM of the mitral valve resulting in significant LVOTO (Figure 2 and Figure 3), with peak pressure gradient of 39 mmHg at rest, which rose to 78 mmHg with bicycle exercise (Figure 4 and Figure 5). There was also moderate to severe mitral regurgitation. The length of the anterior mitral leaflet was 2.2 centimetres, and the aorto-LV angle was measured at 121 degrees. An incidental inter-atrial septum mass on the left atrium was also noted, suggestive of an atrial myxoma. She was started on beta-blockade for symptom relief, but despite that remained very symptomatic.
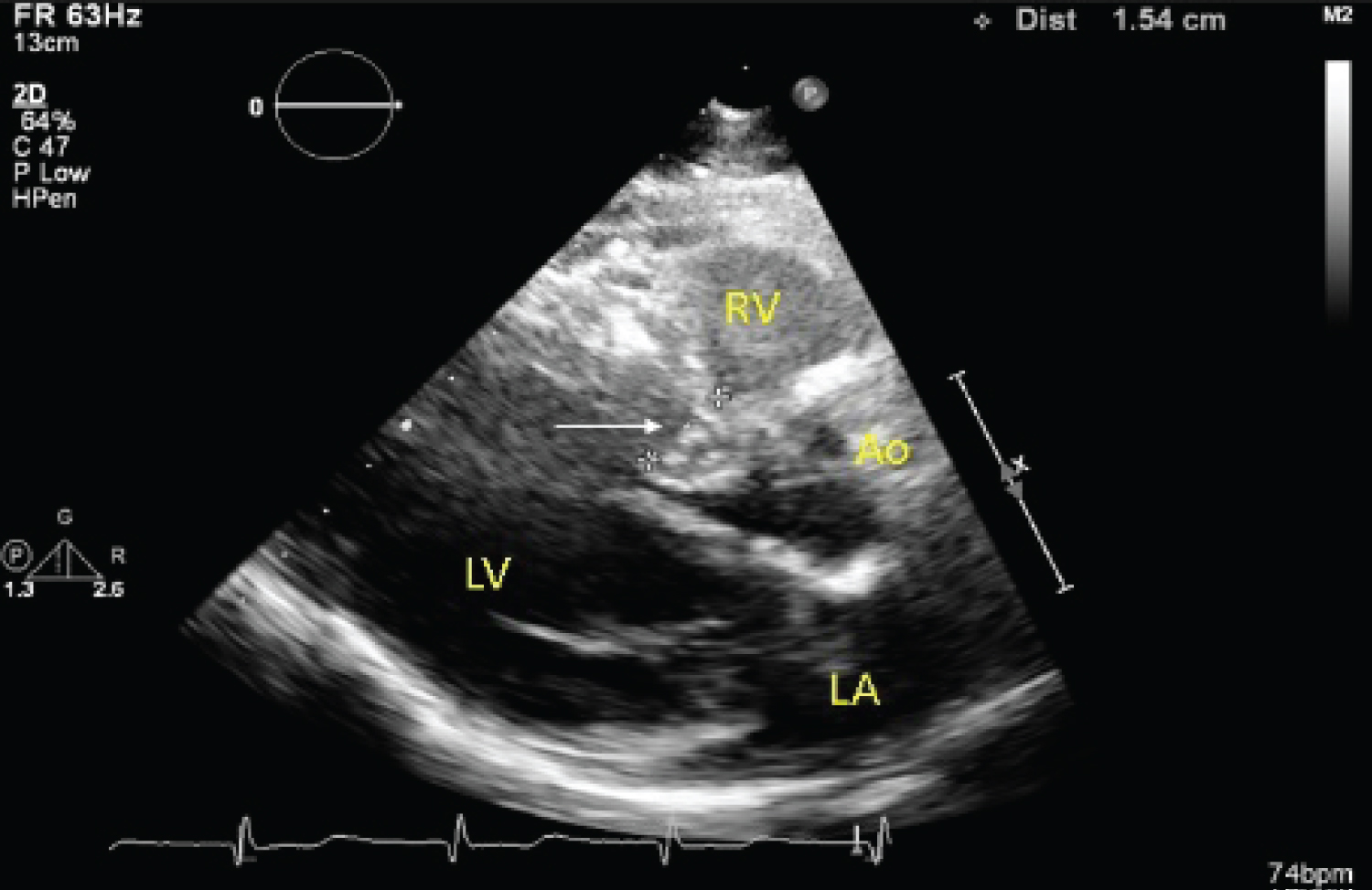 Figure 1: Sigmoid septum (white arrow) with maximal thickness of 15 mm.
Figure 1: Sigmoid septum (white arrow) with maximal thickness of 15 mm.
LA: Left Atrium; LV: Left Ventricle; AO: Aorta; RV: Right Ventricle.
View Figure 1
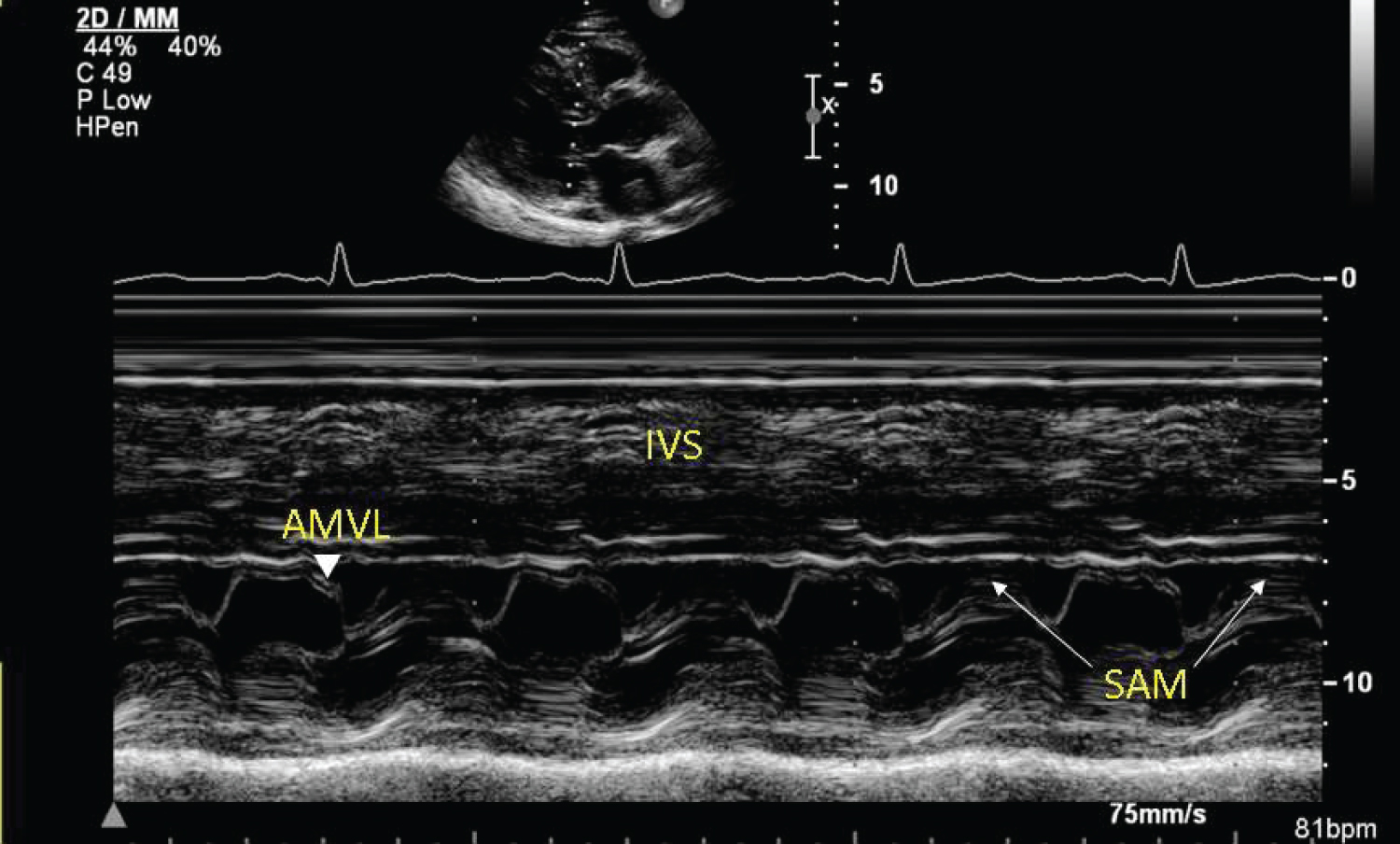 Figure 2: M-mode showing systolic anterior motion (white arrows) of the anterior mitral valve leaflet.
Figure 2: M-mode showing systolic anterior motion (white arrows) of the anterior mitral valve leaflet.
AMVL: Anterior Mitral Valve Leaflet; IVS: Inter-Ventricular Septum; SAM: Systolic Anterior Motion.
View Figure 2
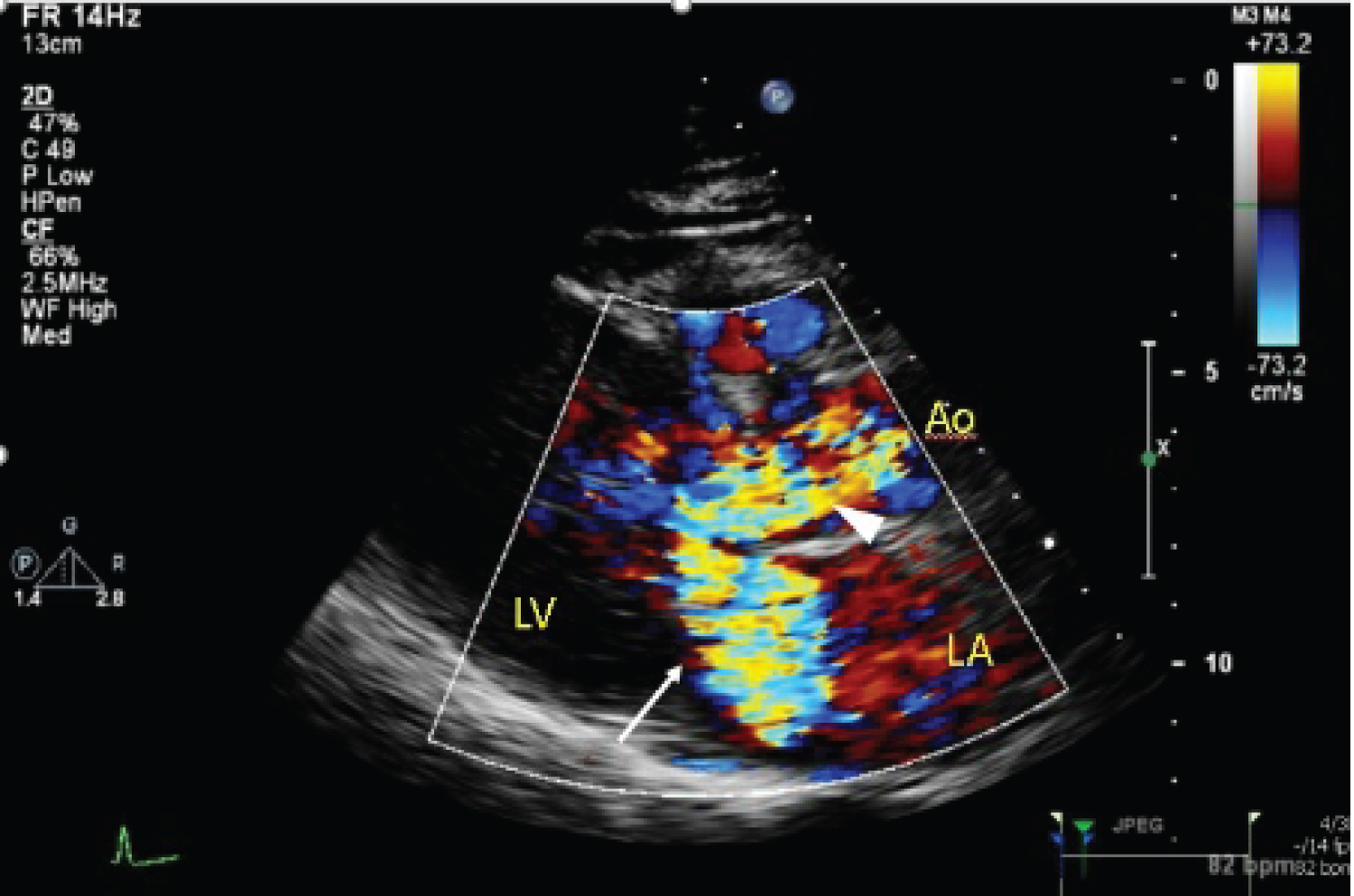 Figure 3: Colour flow (white arrowhead) showing flow acceleration through left ventricular outflow tract (LVOT), signifying obstruction. There is also significant mitral regurgitation (white arrow).
View Figure 3
Figure 3: Colour flow (white arrowhead) showing flow acceleration through left ventricular outflow tract (LVOT), signifying obstruction. There is also significant mitral regurgitation (white arrow).
View Figure 3
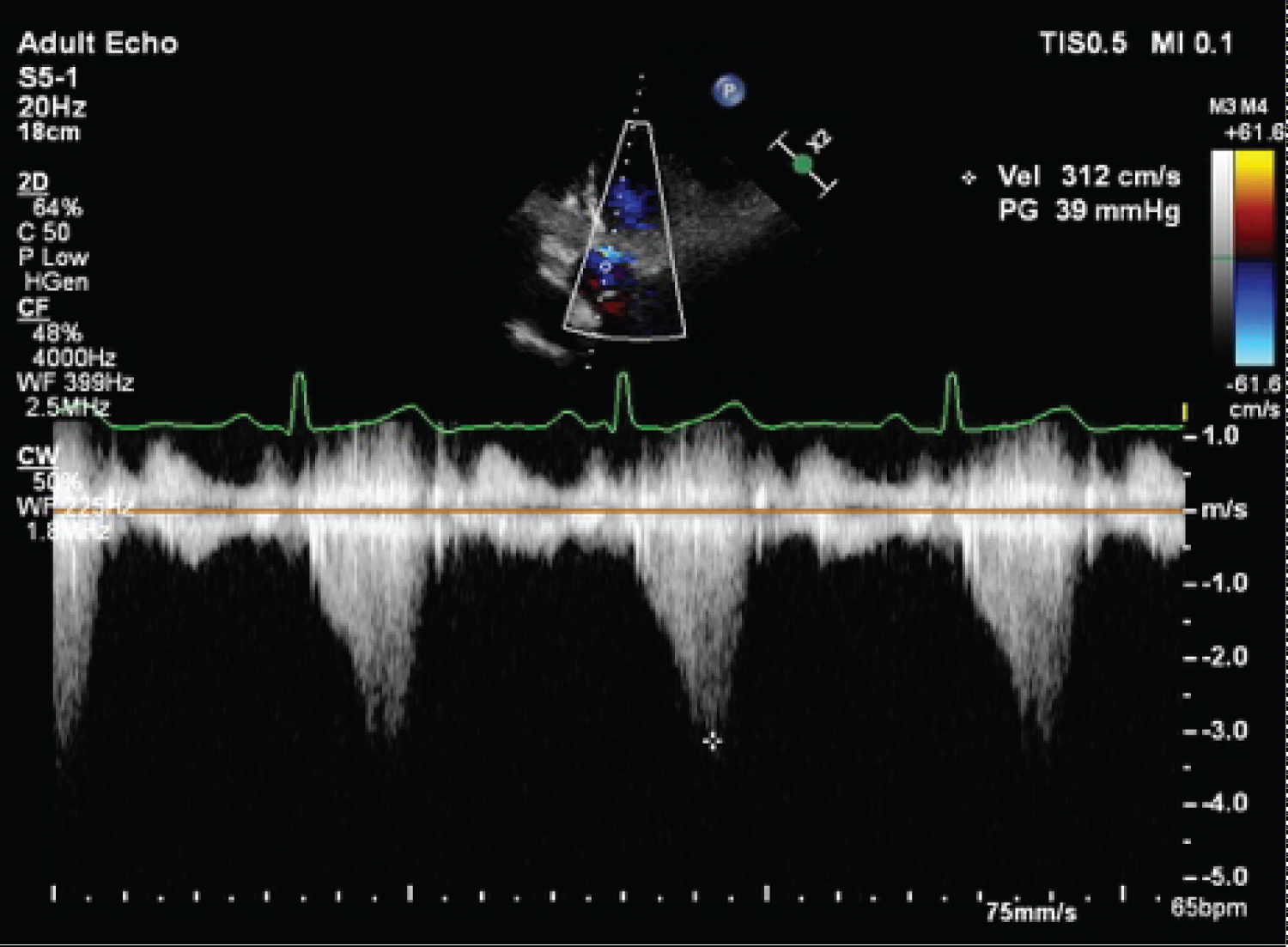 Figure 4: Peak LVOT gradient (39 mmHg) at rest.
View Figure 4
Figure 4: Peak LVOT gradient (39 mmHg) at rest.
View Figure 4
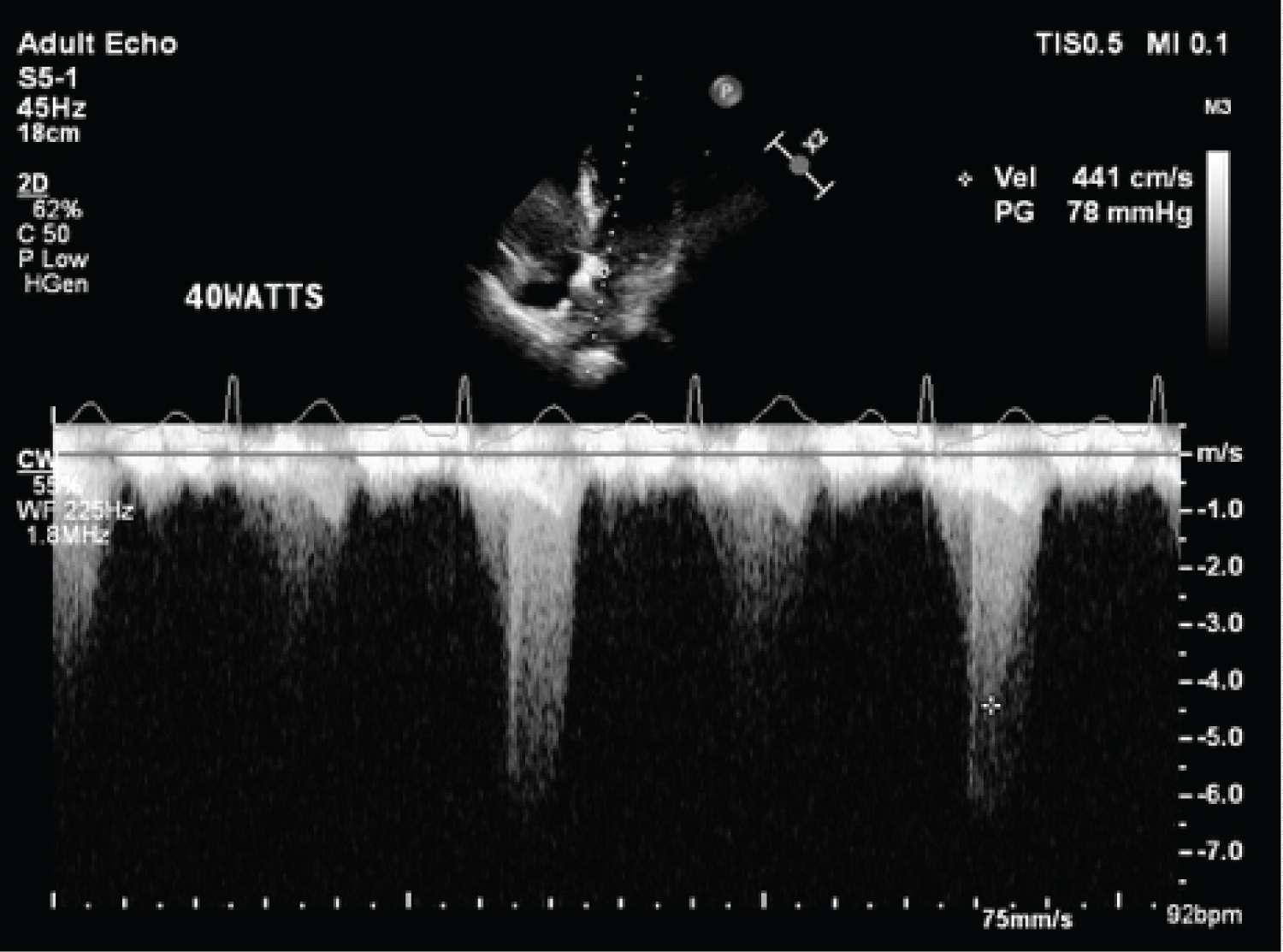 Figure 5: LVOT gradient increasing to 78 mmHg with bicycle exercise.
View Figure 5
Figure 5: LVOT gradient increasing to 78 mmHg with bicycle exercise.
View Figure 5
She had a computed tomography coronary angiogram which showed severe stenosis in the left anterior descending artery, and confirmed the presence of the previously seen left atrial mass noted on transthoracic echocardiography. A diagnostic coronary angiogram demonstrated single vessel coronary artery disease of 70-80% stenosis of the mid left anterior descending coronary artery.
Her case was discussed with the cardiothoracic surgical team, and the decision was for single-vessel coronary artery bypass with left atrial mass excision and mitral valve repair. Intra-operative trans-esophageal echocardiogram showed systolic anterior motion of the mitral valve, with resultant severe mitral regurgitation (Figure 6). The maximum resting intra-left ventricle gradient was measured at 72 mmHg. A well circumscribed mass was attached to the inferior-posterior left atrial wall, in keeping with a known left atrial myxoma. Single vessel coronary artery bypass grafting of the left internal mammary artery (LIMA) to the 2nd diagonal artery with excision of the left atrial myxoma was performed, followed by mitral valve repair with an Alfieri stitch applied from the A2 to P2 mitral leaflets (Figure 7). Immediate post-operative trans-esophageal echocardiogram showed reduction in mitral regurgitation to mild severity with reduction in systolic anterior motion of the mitral valve (Figure 8 and Figure 9). Peak pressure gradient across the left ventricular outflow tract was reduced to 27 mmHg. The patient made an uneventful recovery, and repeat transthoracic echocardiography done on post-operative day 10 showed satisfactory trans-mitral gradient of 3 mmHg with resolution of the prior systolic anterior motion of the mitral valve. There was non-significant left ventricular outflow tract gradient of 28 mmHg at rest. She was discharged the following day.
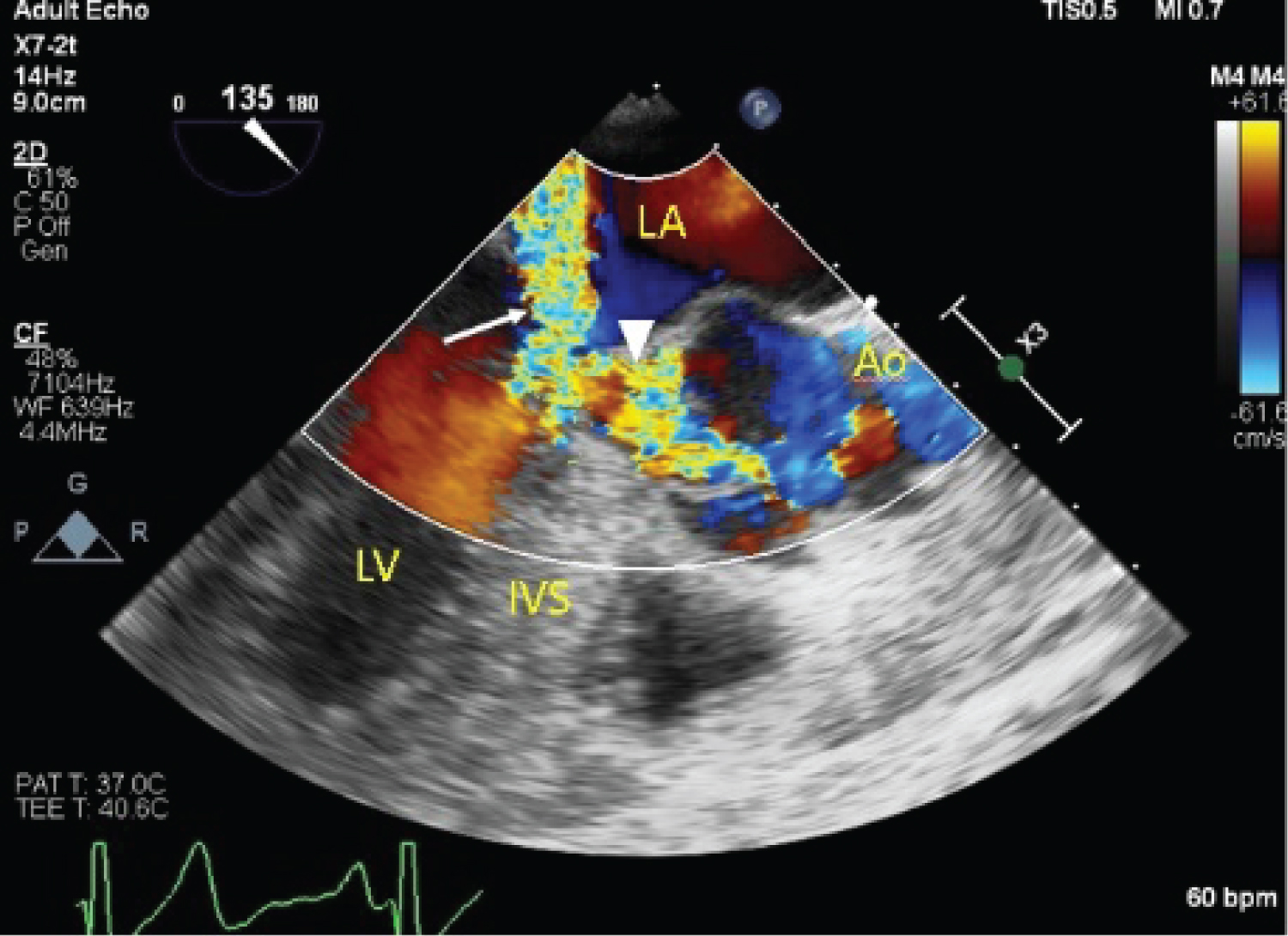 Figure 6: Intra-operative TEE showing LVOT obstruction (arrowhead) and severe mitral regurgitation (arrow).
View Figure 6
Figure 6: Intra-operative TEE showing LVOT obstruction (arrowhead) and severe mitral regurgitation (arrow).
View Figure 6
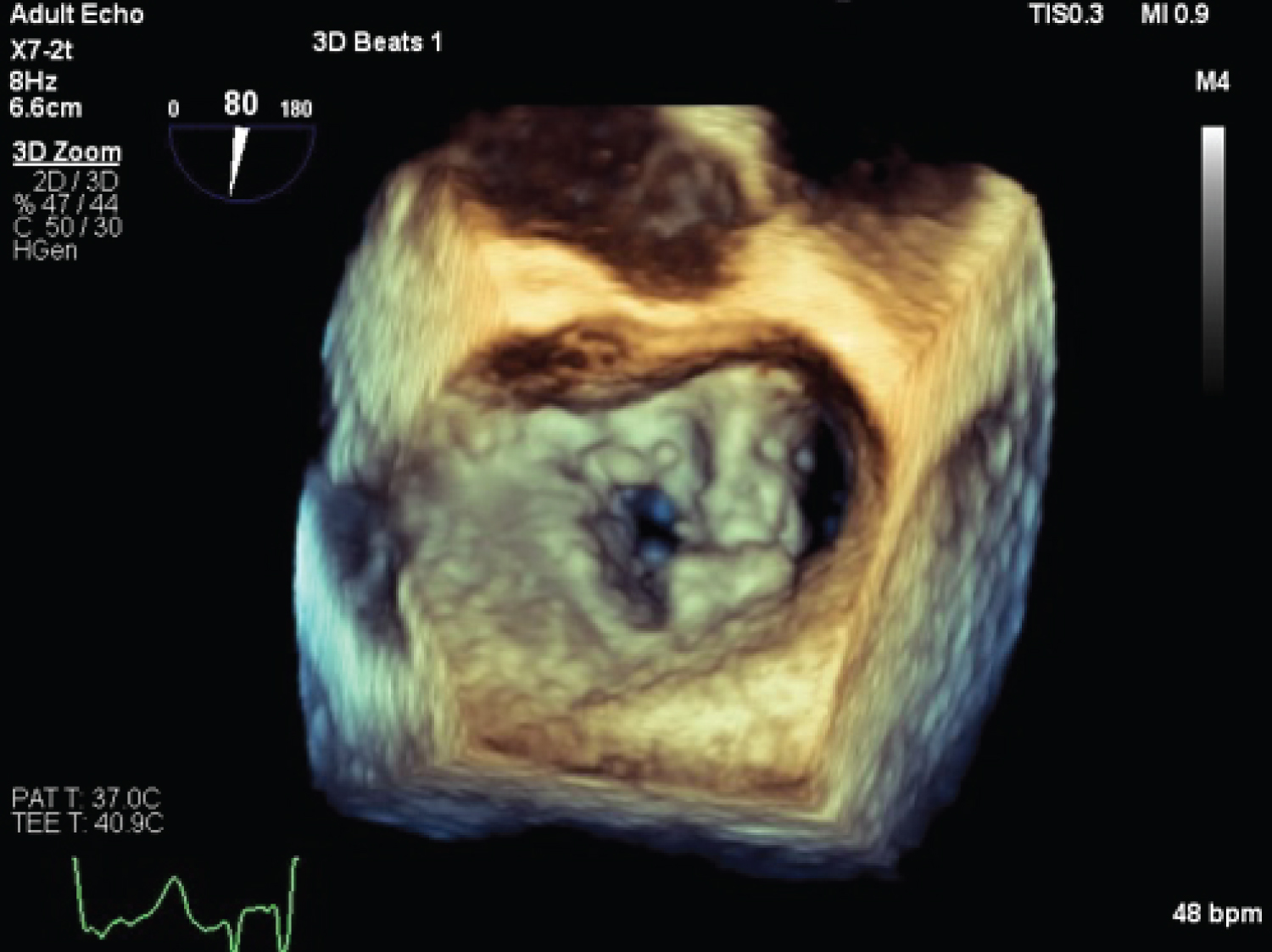 Figure 7: Post-operative 3D TEE showing the characteristic 'double orifice' appearance of the mitral valve post Alfieri stitch.
View Figure 7
Figure 7: Post-operative 3D TEE showing the characteristic 'double orifice' appearance of the mitral valve post Alfieri stitch.
View Figure 7
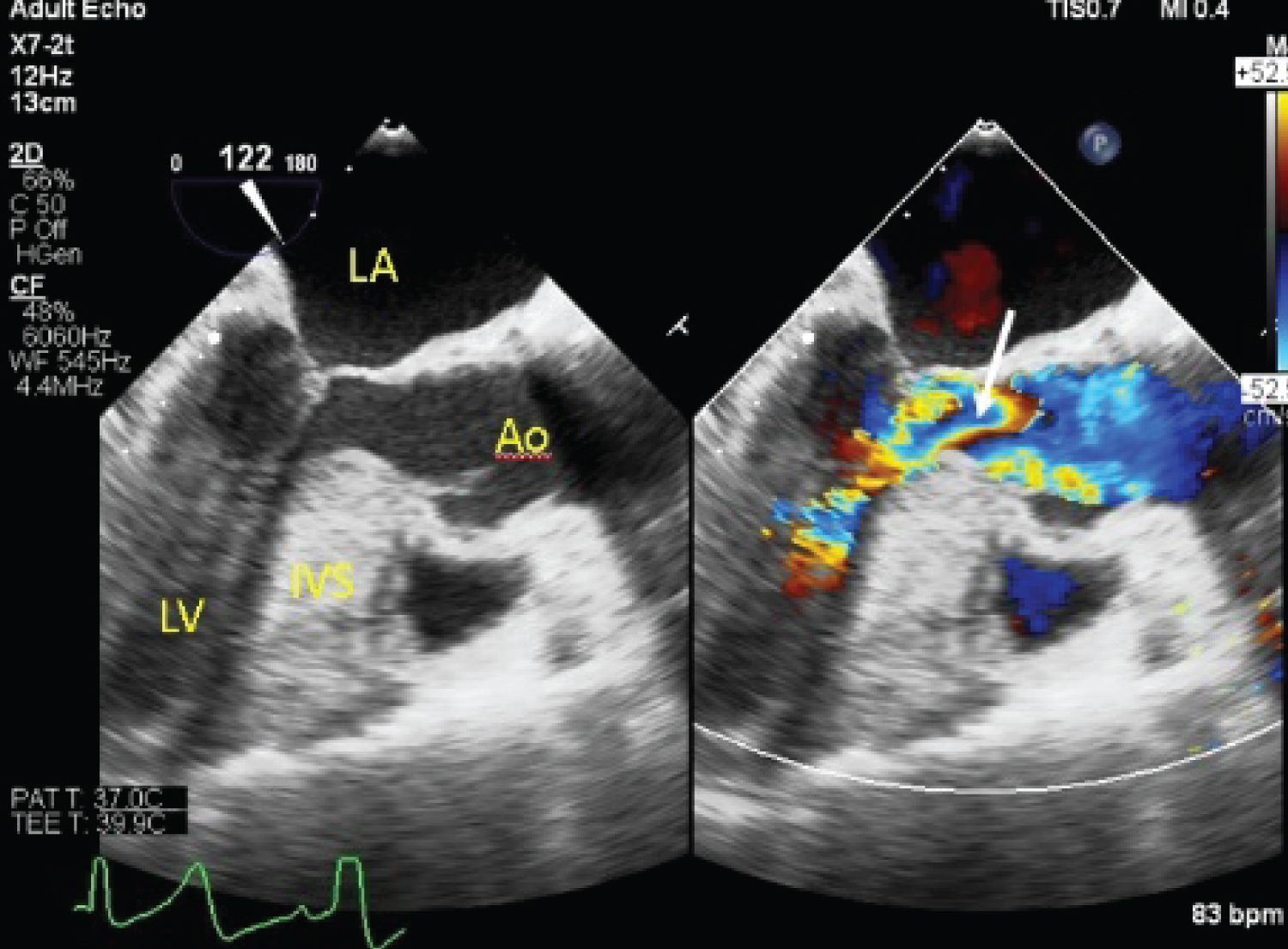 Figure 8: Post-operative TEE showing reduction in LVOT obstruction (arrow).
View Figure 8
Figure 8: Post-operative TEE showing reduction in LVOT obstruction (arrow).
View Figure 8
 Figure 9: Post-operative TEE showing reduction in mitral regurgitation severity (arrow).
View Figure 9
Figure 9: Post-operative TEE showing reduction in mitral regurgitation severity (arrow).
View Figure 9
The patient was followed up and remained well with resolution of her symptoms. A surveillance transthoracic echo done 8 months post-operatively showed similar trans-mitral gradient of 4 mmHg with residual mild-moderate mitral regurgitation with no systolic anterior motion of the mitral valve and no significant left ventricular outflow tract or mid-cavity gradient at rest.
The mechanism of systolic anterior motion (SAM) of the mitral valve is thought to be multi-factorial. Manabeetal [1] described three main mechanisms: 1) Residual anterior leaflet length beyond the coaptation point- the longer the residual length floating in the LVOT, the more significant the SAM and resultant LVOT obstruction; 2) A shortened mitral coaptation to LV septum distance leading to more ejected flow directed between the posterior mitral leaflet and the posterior LV wall, which results in displacement of the anterior leaflet towards the LVOT; and 3) Hyperdynamic LV coupled with a small LV cavity resulting in high-flow ejection velocity, which is quantitatively related with the degree and severity of SAM.
In a study by Uematsu, et al. [2] of 9180 sequential patients, the prevalence of non-HCM SAM was very low at 0.3%. They also compared HCM associated with SAM to non-HCM SAM, and found that the latter group was older and had a higher prevalence of sigmoid septum.
Our patient had a sigmoid septum which is a facet of normal aging, where the base of the interventricular septum protrudes into the left ventricular cavity, and this could have contributed to SAM and LVOTO. Although it has been previously reported that LVOT obstruction could occur in patients with a sigmoid septum and hyperkinetic conditions, our patient had a significant LVOT gradient at rest.
In patients with sigmoid septum related-SAM, treatment strategies are unclear although beta-blockade and class Ia antiarrhythmic drugs might reduce the LVOT pressure gradient. In a report of 2 cases by Ozaki, et al. [3], cibenzoline and atenolol were effective in reducing the LVOT pressure gradients in patients with sigmoid septum. For our patient, she underwent a trial of beta blockade but this proved ineffective with continued symptoms. In view of the presence of a concomitant atrial myxoma that required surgery, she underwent an Alfieri stitch of her mitral valve at the time of myxoma resection that obliterated both the SAM and LVOTO.
A study by Collis, et al. [4] demonstrated that the Alfieri procedure was effective adjunct therapy for prevention or treatment of SAM in the setting of a concomitant septal myomectomy in patients with hypertrophic obstructive cardiomyopathy. Other case studies have also reported using a modified Alfieri's stitch post mitral valve repair to treat SAM. Our case report demonstrates the effective use of an Alfieri stitch to relieve SAM and LVOT obstruction, in the same setting of surgical excision of the left atrial myxoma. For patients who are averse to open heart surgery, transcatheter mitral valve repair has been previously described to be helpful in patients with degenerative mitral regurgitation and concomitant LVOTO due to SAM of the mitral valve in the context of hypertrophic obstructive cardiomyopathy (Schafer, et al. [5], Sorajja, et al. [6]). This approach could be an alternative to the Alfieri stitch even for patients with non-HCM SAM and this was previously demonstrated in a case report from Coylewright, et al. [7].
The patient had a sigmoid septum of maximal 15 mm thickness. Although this could be due to aging as well as her underlying hypertension, we were unable to rule out existing HCM.
The Alferi stitch procedure could represent a viable option in the management of non-HCM or sigmoid septum related SAM with significant LVOTO. Selection of patients will need to be better studied before the procedure can be confidently and widely accepted. There might also be a role for MitraClip as a less invasive method of managing SAM and significant LVOTO in such patients who do not respond to medical therapy.
The authors have no conflicts of interest to declare.