A 75-year-old female with unstable angina who was found to have anomalous left anterior descending coronary artery originating from the right coronary artery close to the ostium presented with recurrent major bleeding while on dual antiplatelet therapy with aspirin and clopidogrel following percutaneous coronary intervention despite treatment with proton pump inhibitor and blood transfusion. When aspirin was discontinued the bleeding episodes subsided for 5 months which was followed by return of the patient with non ST segment elevation myocardial infarction with tight stenosis of the same artery proximal to the previous stent. A successful repeat percutaneous coronary intervention was performed with ticagrelor monotherapy without any bleeding or ischemic episodes for more than one year.
MI: Myocardial Infarction; LAD: Left Anterior Descending; RCA: Right Coronary Artery; ACS: Acute Coronary Syndrome; PCI: Percutaneous Coronary Intervention; TIMI: Thrombolysis in Myocardial Infarction; UGI: Upper Gastrointestinal; CABG: Coronary Artery Bypass Grafting; DAPT: Dual Antiplatelet Therapy
Coronary artery anomalies have been discovered as incidental findings during angiography, surgery and autopsy as component of complex congenital malformations of the heart or may be an isolated defect [1]. Anomalous origin and course of the coronary arteries may remain asymptomatic, or may cause chest pain, sudden death, cardiomyopathy, syncope, dyspnea, ventricular fibrillation and MI [2]. The determination of variations in the course and origin of the major coronary arteries is important in coronary surgery and angiography. Evidences derived from angiographies performed for suspected obstructive disease determined that coronary anomalies affect about 1% of the general population [3]. Abnormal origin of left anterior descending (LAD) coronary artery from the right coronary artery (RCA) is a rare anomaly in coronary angiogramswhile its occurrence is in 4% of the patients with tetralogy of Fallot [4,5].
Among patients who have an acute coronary syndrome (ACS) or who have undergone percutaneous coronary intervention (PCI), the risk of thrombotic events is lower with dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 receptor inhibitor than with aspirin alone [6]. Post-PCI bleeding has been shown to be associated with a substantial and durable risk of death, approximating or even exceeding that associated with MI [7]. Avoidance of aspirin therapy may allow for more prolonged use of potent P2Y12 inhibitors curtailing aspirin-related bleeding risk, particularly with respect to gastrointestinal toxicity.
Presence of LAD coronary artery emerging from RCA is classified among the rare coronary anomalies and successful PCI with long lasting result using a single antiplatelet agent is exceptional. I herein report a 75-year-old diabetic and hypertensive female who presented to Gesund Cardiac and Medical Center, Addis Ababa, Ethiopia, before one year with typical angina triggered by minor activities of one month duration whose coronary angiography showed normal circumflex coronary artery, anomalous LAD originating from the RCA adjacent to the ostium and long segment 95% stenosis of mid RCA (Figure 1) with recurrent major bleeding on DAPT who was successfully managed with ticagrelor monotherapy following PCI.
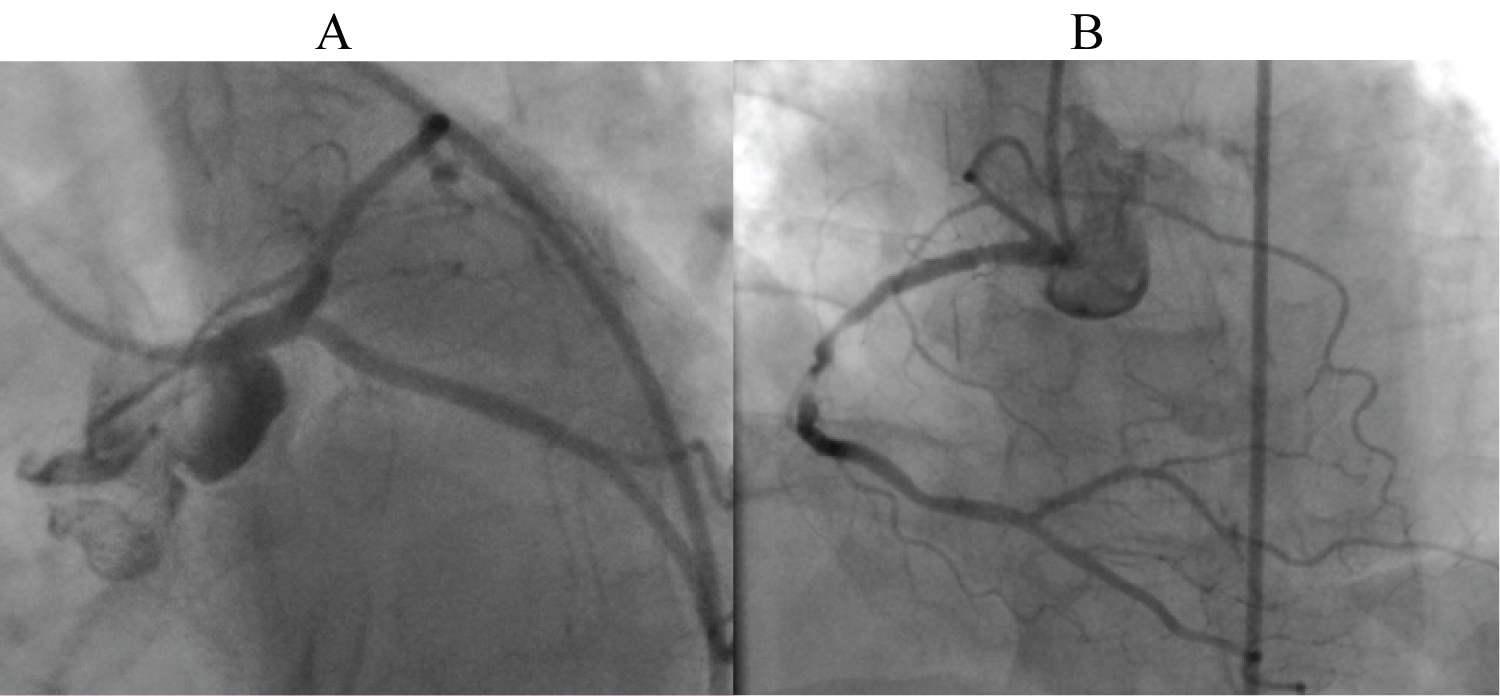 Figure 1: A) left coronary artery without LAD territory; B) Dominant RCA with long segment tight stenosis and LAD originating from proximal RCA.
View Figure 1
Figure 1: A) left coronary artery without LAD territory; B) Dominant RCA with long segment tight stenosis and LAD originating from proximal RCA.
View Figure 1
During her initial presentation, cautious PCI was done using resolute integrity stent (zotarolimus eluting) resulting in thrombolysis in myocardial infarction (TIMI) III flow and she was continued with aspirin 81 mg/day, clopidogrel 75 mg/day, atorvastatin 40 mg/day, metoprolol succinate 25 mg/day and pantoprazole 40 mg/day. After two weeks, she came back with profound fatigue, dyspnea, pallor, tarry stool, and hemoglobin of 8 g%. Upper gastrointestinal (UGI) endoscopy, done after stabilization of the patient with 2 units of whole blood, revealed erosive gastritis which was managed with intravenous proton pump inhibitor.
Despite this, the patient had to present for 3 other episodes of UGI bleeding over 4 months and she was managed similarly. After the 4th episode of bleeding, aspirin was desperately discontinued while the remaining medications were maintained. This was followed by 5 months of clinical stability without bleeding, fatigue or chest pain. Nine months after the initial presentation, she developed chest pain at rest with T-wave inversions involving the inferior leads plus elevated troponin congruent with acute MI. A repeat coronary angiography showed a new discrete 90% stenosis of the proximal RCA distal to the origin of the anomalous LAD with fully patent previously stented segment. This time again, PCI was done with successful result using the same type of stent while ticagrelor was utilized as the sole antiplatelet agent (Figure 2). She is comfortable up until now without chest pain or any bleeding episode for over one year.
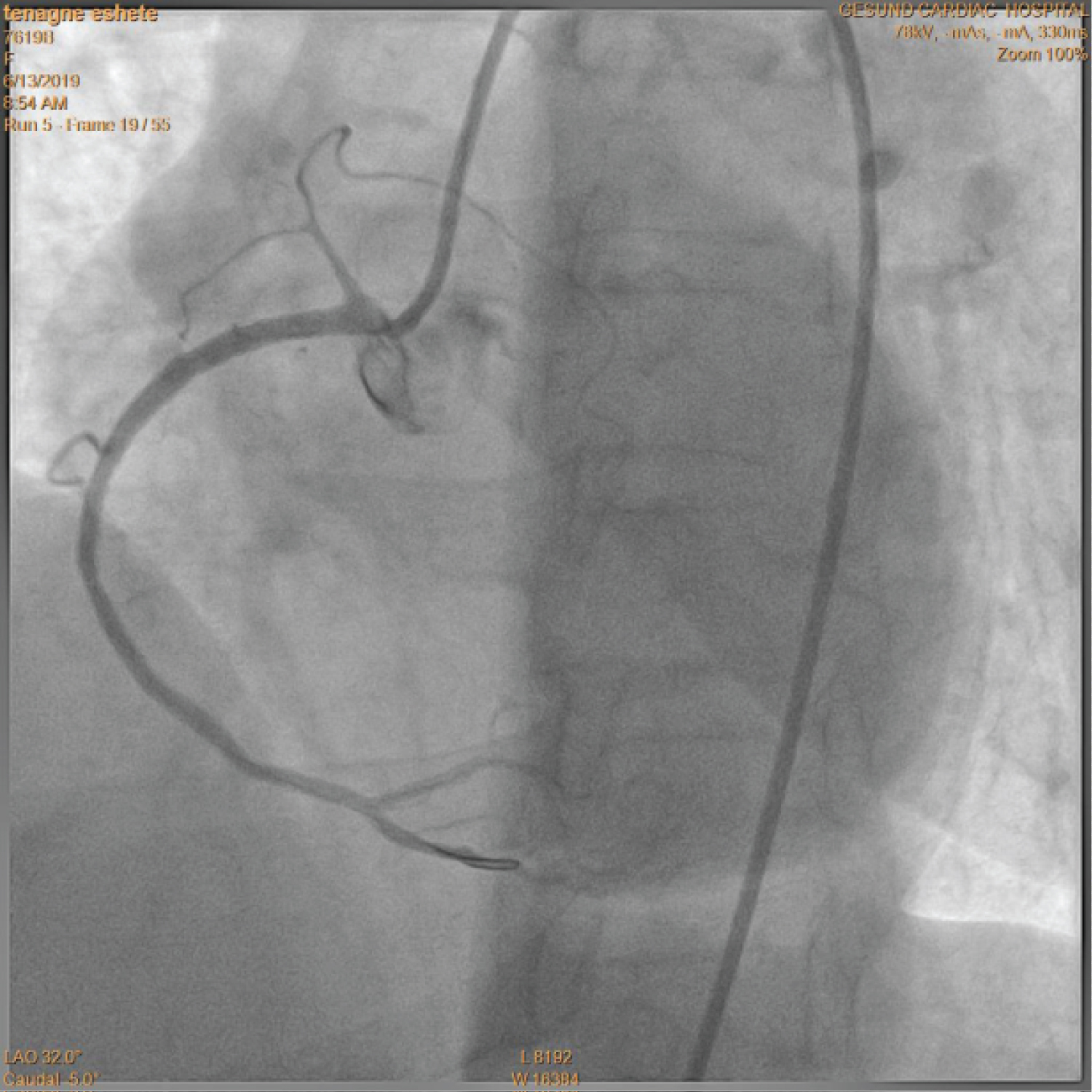 Figure 2: Final result after the repeat PCI on the proximal RCA.
View Figure 2
Figure 2: Final result after the repeat PCI on the proximal RCA.
View Figure 2
Abnormal origin of LAD coronary artery from the RCA is a very rare anomaly in coronary angiograms [4]. In this patient, the origin of LAD was very close to the RCA ostium which required immense care in the course of PCI to circumvent complications. During the second episode of ACS with intense chest pain and troponin positivity, to avoid the GI toxicity of aspirin, coronary artery bypass grafting (CABG) was considered, but she was deemed high surgical risk because of the debilitating effect of the recurrent bleeding. Performance of PCI with a single antiplatelet agent, ticagrelor, has proven successful in this elderly patient at high risk for bleeding as well as thrombotic complications.
Among patients who have undergone PCI, the risk of thrombotic events is lower with dual antiplatelet therapy with aspirin and a P2Y12 receptor inhibitor than with aspirin alone [6]. In the Ticagrelor vs. Clopidogrel in Patients with Acute Coronary Syndromes (PLATO) trial, ticagrelor, a reversible and direct-acting oral antagonist of the adenosine diphosphate (ADP) receptor P2Y12, which provides faster, greater, and more consistent P2Y12 inhibition than clopidogrel, was shown to reduce the rate of death from vascular causes, MI, or stroke without an increase in the rate of overall major bleeding when added to aspirin replacing clopidogrel [8]. Despite these remarkable achievements, post-PCI bleeding due to DAPT has been associated with a substantial risk of death, approximating or even exceeding that associated with MI [9].
Reducing the duration of aspirin therapy may allow for more prolonged use of potent P2Y12 inhibitors while avoiding aspirin-related bleeding risk, particularly with respect to GI toxicity. In the Ticagrelor with or without Aspirin in High-Risk Patients after PCI (TWILIGHT) trial ticagrelor monotherapy was superior to ticagrelor plus aspirin to lower the incidence of clinically relevant bleeding with no higher risk of death, MI, or stroke when started after 3 months of DAPT following PCI [10]. In my steadfast observation, it was apparent that my patient would not tolerate dual antiplatelet therapy for 3 months. Given the broad study population in the PLATO trial and the aforementioned study showing the benefit of ticagrelor monotherapy, I desperately decided to do a repeat PCI with ticagrelor alone from day one, after proper counselling of the patient and her family, with gratifying result without bleeding or thrombotic events for over one year. A recent study has also reported similar results to that of TWILIGHT trial instituting ticagrelor monotherapy 3 months after PCI done in ACS patients [11].
Successful PCI was done in the presence of a rare coronary anomaly, LAD originating from the RCA close to the RCA ostium, requiring immense care in the course of the procedure to avoid complications. Performance of PCI in a high risk patient with ticagrelor monotherapy from day one has been successful to avoid DAPT, particularly aspirin related recurrent bleeding and thrombotic complications.