Heart failure (HF) is a common complication in patients with hypertension who may present as HF with preserved ejection fraction (HFpEF) or HF with reduced ejection fraction (HFrEF). These categories have different clinical presentations and may require special attention to diagnose, especially when the presentation is HFpEF. The aim of this study was to assess the prevalence, types and clinical presentation of HF among hypertensive patients being followed-up at a tertiary hospital in Tanzania.
We included all known and newly diagnosed hypertensive adults (≥ 18 years) referred for echocardiogram examination at the Muhimbili National Hospital - Mloganzila, between June and December 2019. A detailed cardiovascular history, physical, laboratory and echocardiogram examination was performed in all patients. HF was diagnosed according to the Framingham criteria and was further categorized as HFpEF (EF ≥ 50%) or HFrEF (EF < 50%), according to the echocardiography findings. Patients from these two groups were then compared in terms of demographic, clinical, laboratory and echocardiographic characteristics. The chi-square and Student's t test was used to compare categorical and continuous data respectively. A p-value of < 0.05 indicated a statistically significant difference.
Out of 633 hypertensive patients seen during the study period, 346 (54.7%) fulfilled the inclusion criteria and were enrolled. Mean ± SD age was 58.3 ± 12.4 years, and 60.4% were women. Mean ± SD systolic and diastolic BP was 152 ± 23 and 91 ± 15, respectively. A total of 102 (29.5%) patients were found to have HF. Three quarters of HF patients (74.5%) had HFpEF and the remaining (25.5%) had HFrEF. In comparison, patients with HFpEF were more likely to be outpatients, older, obese, and with higher mean BP and more concentric left ventricular hypertrophy when compared to those with HFrEF, all p < 0.05.
The prevalence of HF among hypertensive patients seen at a tertiary hospital in Tanzania is 29.5%, majority of them having HFpEF. HFpEF differs from HFrEF in terms of BP levels, obesity status and some echocardiographic parameters. These factors need to be carefully examined when HF is suspected in otherwise less symptomatic patients.
Heart failure, Hypertension, Heart failure with preserved ejection fraction, Heart failure with reduced ejection fraction, Diastology, Echocardiogram, Sub Saharan Africa, Tanzania
Heart failure (HF) is a global pandemic that affects approximately 64.3 million people worldwide [1], representing an important cause of morbidity and mortality [2]. The age-standardized prevalence rates of HF is increasing, and is accompanied with an increase in mortality and years lived with disability, especially in low and middle income countries (LMIC) [1]. The increasing HF burden is especially significant in sub Saharan Africa (SSA), including Tanzania, which is experiencing a change in epidemiology of diseases from communicable to non-communicable diseases [3]. Hypertension is by far the most common underlying cause contributing to the increase of HF burden in SSA [4], being present in 14.9% to 29.8% of the adult population [5,6], and in up to 50% of those aged ≥ 55 years [5]. Furthermore, hypertension in SSA is more severe and results in early end-organ damage, including HF, chronic kidney disease and stroke [7].
Regardless of the type, a diagnosis of HF carries a significant morbidity and mortality risk [8,9], and efforts should be made to diagnose HF earlier than later. With the aid of echocardiogram, HF has been classified into two major categories: HF with preserved ejection fraction (HFpEF) and HF with reduced ejection fraction (HFrEF) [10]. Among patients with hypertension, studies have found HFpEF to be more common, mainly due to diastolic dysfunction of the hypertrophied left ventricle [11,12]. HFpEF needs careful attention to diagnose, as traditionally HF was defined as a presence of reduced ejection fraction on echocardiogram. Ascertaining the proportion of hypertensive patients with HFpEF is important as it will increase awareness among clinicians of this otherwise obscured disease [13]. However, only few studies have reported on the types of HF among hypertensive patients in SSA [8,14,15], and most of previous studies did not systematically look for HF symptoms therefore may have missed those with mild to moderate symptoms. Furthermore, no previous study in Tanzania has reported on the types of HF among exclusively hypertensive patients. This study was therefore set out to determine the prevalence, types and clinical characteristics of HF in a population of hypertensives attending a tertiary hospital in Tanzania.
A structured questionnaire was used to collect patients' socio-demographic and clinical data. Information collected included gender, age of the patient, area of residence, cardiovascular risk factors, symptoms of HF, etc. A thorough physical examination was done and cardiovascular signs like ankle edema, upper quadrant abdominal tenderness, chest rales, S3 gallop, and jugular venous pulse were looked for and recorded whether present or not. The Framingham criteria was used to assess for the presence of HF among patients [16].
Blood pressure (BP) was measured according to guidelines [17], using a standard automated BP machine (Heuer Company, from USA). Hypertension was defined as systolic BP of ≥ 140 mmHg and/or diastolic BP of ≥ 90 mmHg, or known hypertensive on medications, and was categorized as grade 1 (140-159/90-99 mmHg), grade 2 (160-179/100-109 mmHg) and grade 3 (≥ 180/≥ 110 mmHg) according to European Society of Cardiology guidelines [17]. Height, weight, waist and hip circumferences were measured following standard guidelines.
For each patient, a 10 ml of venous blood was collected and analyzed for cholesterol, glucose, creatinine, urea nitrogen and hemoglobin levels. High triglyceride levels were defined when serum triglyceride was > 1.69 mmol/l, raised LDL-C was defined when serum LDL-C was > 3.34 mmol/l, high total cholesterol was defined when serum total cholesterol was > 5.2 mmol/l and low HDL-C was defined when serum HDL-C was < 1.04 mmol/l, according to the Muhimbili National Hospital's laboratory reference values. Estimated glomerular filtration rate (eGFR) was calculated from CKD-EPI equations [18] and renal dysfunction was considered to be present when a patient had eGFR of less than 60 ml/min/1.73 m2. Anemia was defined as hemoglobin of less than 13 g/dl in men and 12 g/dl in women according to the World Health Organization [19].
Echocardiograms were performed using a General Electric (GE) Vivid S3 echocardiogram machine equipped with a 3.5 MHZ transducer, and the protocol followed the American Society of Echocardiology recommendations [20]. Left ventricular (LV) hypertrophy (LVH) was considered present when LV mass (LVM) indexed to body surface area (LVMI) was > 95 g/m2 in women and > 115 g/m2 in men. LVEF was determined using M-mode guided parasternal long-axis images of the left ventricle and was taken as a measure of LV systolic function. EF of < 50% was considered as systolic dysfunction [20]. LV filling was obtained by determining peak early velocity (E) at the level of the mitral leaflets' tips, and the medial early diastolic mitral annular velocity (E′) was measured by spectral tissue Doppler imaging in apical four-chamber views. The ratio of E to E′ velocity (E/E′ ratio) was taken as an estimation of LV filling pressure and diastolic dysfunction was considered present when the E/E' was ≥ 15 [21].
Patients with HF as per Framingham criteria were further categorized as HFrEF (when EF < 50%) or HFpEF (EF ≥ 50%) [10]. The diagnosis of HFpEF required the following conditions to be satisfied: (i) Positive diagnosis of HF as per Framingham criterion; (ii) LV EF ≥ 50%; (iii) LV diastolic dysfunction, i.e. E/E' ≥ 15. The diagnosis of HFrEF was reached when the following conditions were satisfied (i) Positive diagnosis of HF as per Framingham criterion and (ii) Reduced LV systolic function on echocardiogram (i.e. LV ejection < 50%) [10].
All questionnaires were scanned for completeness and coded before being entered into the dataset. Statistical package of Social Science for Windows (SPSS) version 21 was used for statistical analysis. Continuous variables were expressed as the mean ± SD, and categorical variables as n (%). The χ2 or Fisher's exact test was used to compare categorical variables, as appropriate. Student's t test was used to compare the mean values. For statistical tests a two-tailed p-value < 0.05 was considered significant.
This study was conducted in accordance with the Helsinki Declaration of studies on human subjects. Ethical approval to conduct the study was obtained from the Directorate of Research and Publications of the Muhimbili University of Health and Allied Sciences. All patients had to sign an informed consent form before any data was collected.
Three hundred and forty six (54.7%) out of 633 hypertensive patients that were screened fulfilled the inclusion and exclusion criteria and were enrolled. Of those excluded, 88 did not give consent, 12 were pregnant, 16 were admitted in the Intensive Care Unit and 171 were referred more than once. Table 1 shows the socio-demographic and clinical characteristics of the study participants. The mean age of the total studied population was 58.3 years (range 28-89 years). Majority (88.1%) of participants were from outpatient clinics. Obesity was present in 30.6% of the participants. The mean ± SD systolic and diastolic blood pressure in the total population was 152 ± 23 mmHg and 91 ± 15 mmHg respectively, and those with stage 3 hypertension were 18.2%. Anemia was present in 31.3% of the total population, and 24.5% had renal dysfunction.
Table 1: Demographic, clinical and laboratory characteristics of the study population. View Table 1
Figure 1 shows the drugs used by study patients, while the symptoms and signs of HF experienced by study patients are shown in Table 2. Antihypertensives receptor blockers were the most used antihypertensive (39%), followed by calcium channel blockers (34.7%), thiazide diuretics (25.7%) and beta blockers (9.5%).
Table 2: Symptoms and signs of HF among study patients. View Table 2
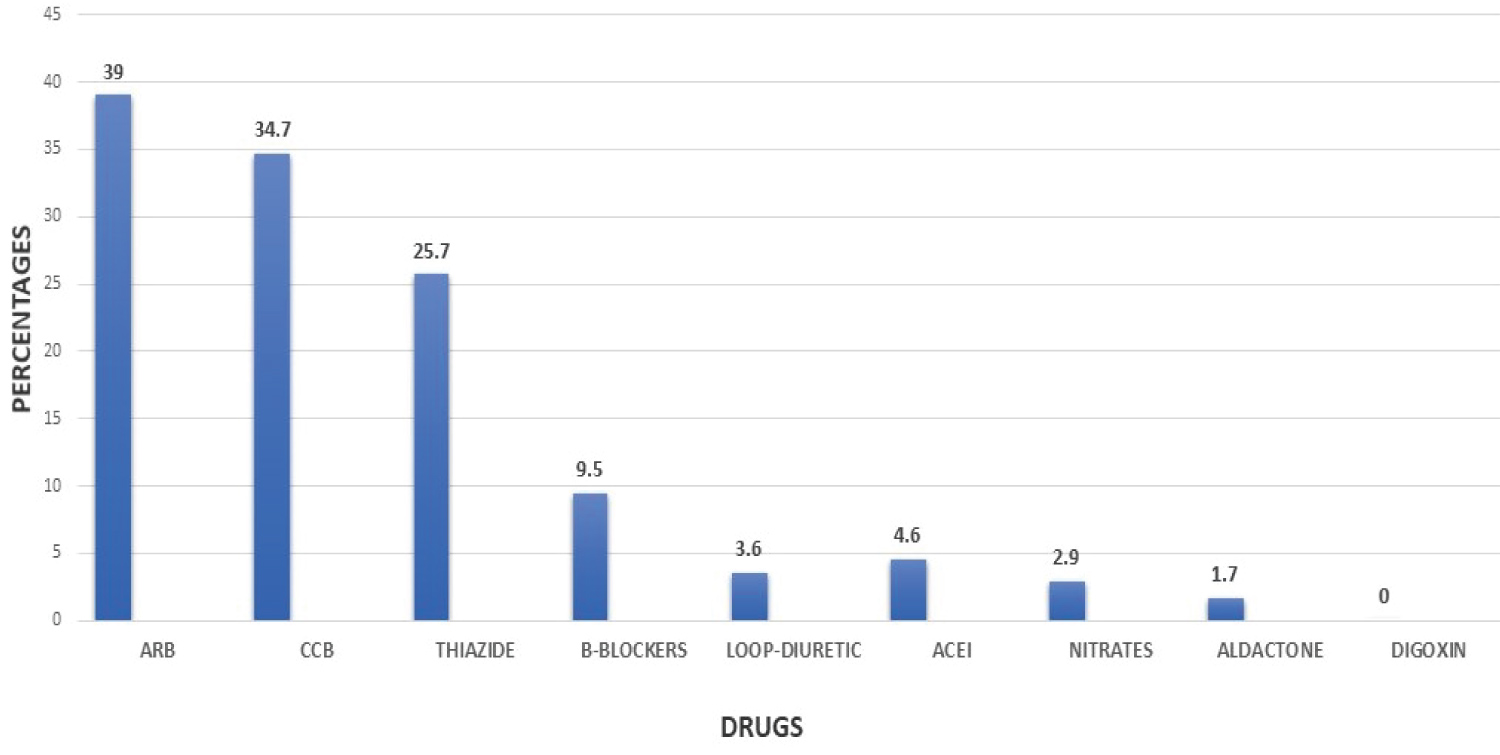 Figure 1: Types of drugs used by hypertensive patients.
Figure 1: Types of drugs used by hypertensive patients.
ARB: Angiotensin Receptor Blocker; CCB: Calcium Channel Blocker; ACEI: Angiotensin Converting Enzyme Inhibitor
View Figure 1
Echocardiogram findings of the study patients are shown in Table 3. As seen in the table, more than half (52.9%) of the total studied had LVH, 9.5% had LV systolic dysfunction, and 20.5% had LV diastolic dysfunction.
Table 3: Echocardiographic findings of the study population. View Table 3
One hundred and eight out of the 346 studied population fulfilled the Framingham criteria for HF. Among the 108 patients who met clinical criteria for HF, 26 had EF < 50%, while 82 had EF ≥ 50% in echocardiogram. Of the 82 participants with clinical HF and EF ≥ 50%, 6 did not meet the echocardiographic definition of diastolic dysfunction and therefore they did not have HF, leaving 102/346 (29.5%) as the true prevalence of HF in this population. Among 102 patients with HF, 76 (74.5%) had HFpEF and the remaining 26 (25.5%) had HFrEF (Figure 2).
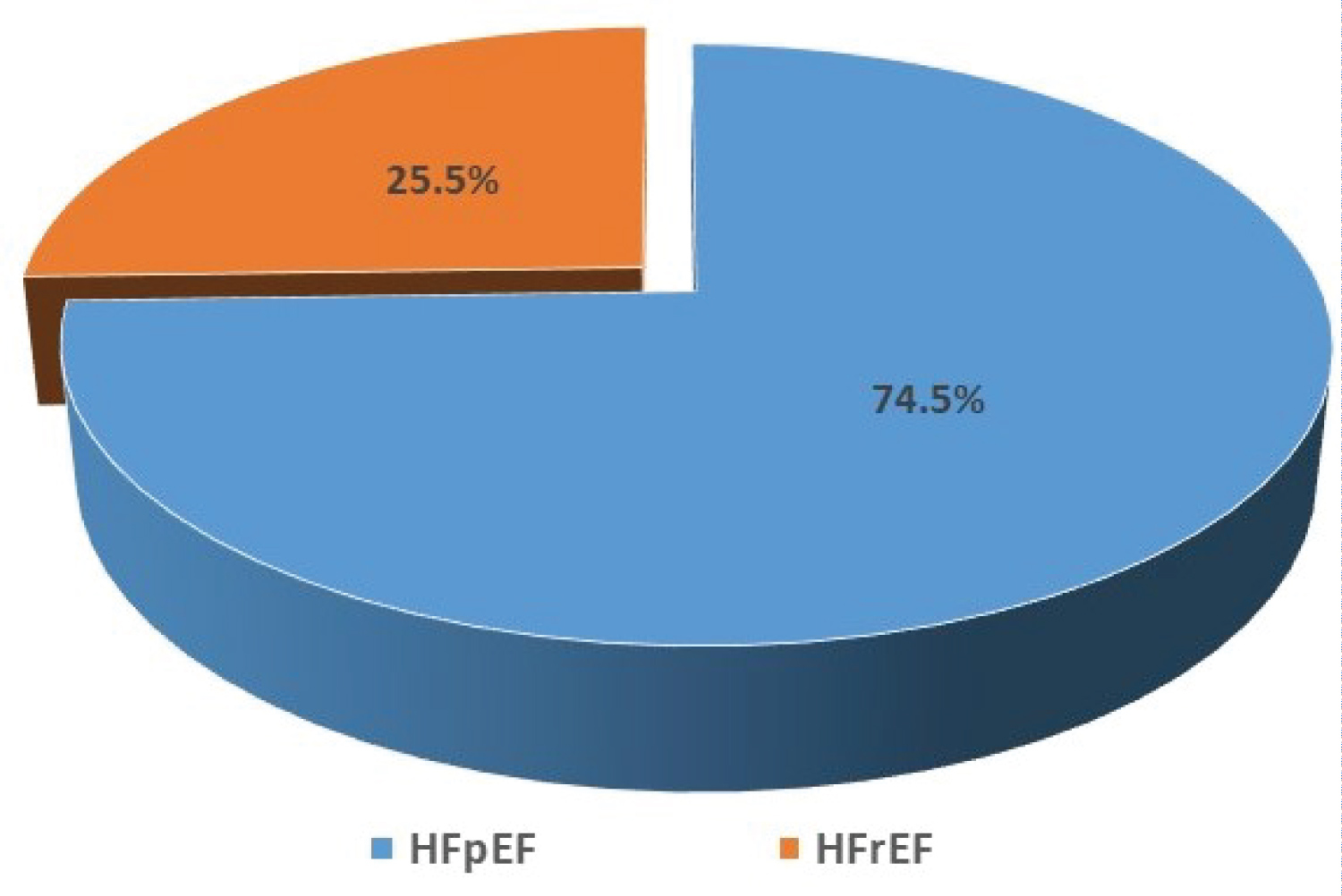 Figure 2: Distribution of HFpEF and HFrEF among hypertensive patients with HF.
View Figure 2
Figure 2: Distribution of HFpEF and HFrEF among hypertensive patients with HF.
View Figure 2
Patients with HFpEF were more likely to be outpatients and showed a trend of being older than patients with HFrEF. In terms of symptoms and signs, patients with HFpEF were less likely to have paroxysmal nocturnal dyspnoea, shifted apex beat, gallop rhythm and basal crepitations, all p < 0.05 (Table 4). In terms of echocardiographic findings, patients with HFpEF were having significantly more concentric LV geometry, while those found to have HFrEF had significantly higher left atrial volume index as well as left ventricle internal diameter, indicating larger LV dimensions all p < 0.05 (Table 4).
Table 4: Average range ratio of high frequency and low frequency in female group. View Table 4
HF is a common complication of hypertension, and its burden may be higher in SSA due to the increased hypertension prevalence [5,6], late hospital presentation [3] and limited ability to diagnose the early disease [1]. In this cross-sectional study of hypertensive patients attending a referral hospital in Tanzania, we highlight 3 important findings that add to the current knowledge of hypertensive heart disease in the region. First, the prevalence of HF among hypertensive patients seen at a referral hospital in Tanzania is 29.5%; second, majority of hypertensive patients with HF have HFpEF; and third, hypertensive patients with HFpEF differ from those with HFrEF in a number of demographic and clinical characteristics.
The prevalence of HF found in this study is in keeping with the findings from a meta-analysis of 23 blood pressure-lowering clinical trials involving 193,424 hypertensives, in whom HF occurred in 28.9% [22]. The present findings also echo our understanding that hypertension is the most common underlying risk factor for HF in SSA accounting up to 45% of HF cases [4]. In population studies, hypertension confers a 2-3 folds increased hazard to HF development [23], indicating very strong links between hypertension and HF. The mechanism of HF in hypertension has been termed to involve chronic pressure overload that leads to the development of left ventricular hypertrophy and fibrotic changes that lead to progressive diastolic dysfunction and failure, while another subset of patients progresses to systolic dysfunction in the presence of chronic volume and pressure overload [24].
Our finding that majority of patients with hypertensive HF have HFpEF is similar to many previous studies that studied hypertensive-only HF cohorts [25-27], and underscores the importance of diastolic HF in this population. However, Ogah, et al. found a 35% proportion of HFpEF in a hypertensive HF registry in Nigeria contrary to the current findings [15]. The difference between ours and the study by Ogah is likely due to the differences in the study population, as HF registry tend to include patients with end stage hypertensive heart disease, where those with diastolic dysfunction progress to have LV dilatation and eventual systolic dysfunction at the end of the hypertensive heart disease spectrum [24]. Nevertheless, active search for HF among hypertensive patients is recommended [21] as most of the patients with HFpEF could have been missed if only ejection fraction was used to categorize HF. Of note, the diagnosis of HFpEF is tricky and it requires thorough assessment of diastolic function to determine presence of increased LV filling pressures [13]. Our definition of diastolic dysfunction as E/E' of ≥ 15 indicate marked raise in LV filling pressures, and therefore true diastolic dysfunction. Of note, these patients had similar proportion of dyspnea which is the hallmark of HF, similar to patients with HFrEF (Table 4). As suggested by guidelines, patients with diastolic HF require similar medications and follow-up as for those with HFrEF [25].
In this study, hypertensive patients found to have HFpEF were more likely to be older adults (≥ 55 years), obese and with higher mean systolic BP when compared to those with HFrEF. These findings are similar to current knowledge of this subset of HF patients [8,12,27], and our findings confirms this observation also among native Tanzanian hypertensives. However, other risk factors including diabetes mellitus and female gender did not show significant associations as previously reported [8,28-30], most likely due to the fact that the current study was not powered to detect these associations, and only trends could be seen. Not surprisingly, clinical signs of shifted apex beat, gallop rhythm, basal crepitations which signify more volume overload were more frequently seen in HFrEF when compared to the group found to have HFpEF, in keeping with previous studies in literature [26].
As expected, patients with HFpEF had more concentric LV geometry on echocardiogram, which is the underlying cause of diastolic dysfunction in hypertensive patients [31]. Of note, while the mean LA volume was high in both groups, those with HFrEF had higher volumes, indicating that patients with HFrEF are at the end spectrum of hypertensive HF, and they are likely to have passed the LV diastolic dysfunction before progressing to HFrEF [32]. This is also confirmed by the higher mean E/E' in the HFrEF group. In short, patients with HFrEF also have diastolic dysfunction while patients with HFpEF have diastolic dysfunction without systolic dysfunction, confirming the notion that diastolic and systolic HF are not independent or separate entities, rather HF is a single continuous disease spectrum and systolic and diastolic HF are phenotypes at two extremes; as advocated by the single syndrome hypothesis of HF [32].
The strength of this study include its prospective nature which allowed for objective and thorough assessment of clinical and echocardiographic parameters, therefore likely to have captured most of hypertensive patients with HF. We did not systematically determine biomarkers of HF like NT-Pro BNP levels in this study, therefore it is possible that some of the HF symptoms could have been due to other conditions like chronic obstructive pulmonary disease. However, the use of the Framingham criteria together with echocardiogram must have offset most of these biases.
In conclusion, the prevalence of HF among hypertensive patients being followed-up at a tertiary hospital in Tanzania is high, and the majority of patients with HF present as HFpEF. We recommend active screening for HF especially in the obese, elderly and uncontrolled hypertensive patients, as they may present with HFpEF which can pass unnoticed.
The authors report no conflicts of interest.
Not applicable.
The authors declare that they have no competing interests.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
GN and PC conceived the research idea. GN recruited patients and did data entry. GN and PC performed echocardiogram, analyzed and interpret data. Both authors drafted the manuscript, have read and approved the final manuscript.
We extend our gratitude to all the study participants for their cooperation offered during this study. Special thanks to Doctor Emmanuel Matulo, Sr. Rose and Sr. Sophia whose work on data collection, recruitment and disposal of patients cannot go unmentioned.