This study sought to evaluate the clinical outcome in cardiac resynchronization therapy (CRT) patients with residual moderate-to-severe functional mitral regurgitation (FMR) who underwent percutaneous treatment with the Mitraclip System or were managed with medical therapy alone.
Significant FMR can persist in 20-25% of patients after CRT and its management can be a challenge, due to the advanced heart failure (HF) and a variety of concomitant comorbidities.
From a single center, two different groups of patients with CRT (MitraClip and no-MitraClip group) were compared. Clinical follow-up was scheduled at 30-day, 12 months and 24 months in all patients. The primary endpoint was the composite of all-cause death or HF hospitalizations at 24-month follow-up.
Forty patients (56%) were treated with the Mitraclip System (MitraClip group) and 31 patients (44%) only with medical therapy (no-MitraClip group). MitraClip group presented higher surgical risk than no-MitraClip group, as older age, chronic kidney disease, higher NYHA functional class and lower left ventricular ejection fraction. At 24-month no differences in all-cause mortality were detected between the two groups (Kaplan-Meier curves log-rank p = 0.947), although the MitraClip group presented lower rate of HF hospitalizations than the no-MitraClip group (log-rank p = 0.048). After adjustment for confounding factors, time to HF hospitalization or death was significantly delayed in MitraClip group (hazard ratio: 0.38; p-value 0.018).
In CRT patients, the treatment of moderate-to-severe FMR with the Mitraclip System - if compared to medical therapy alone - is a safe and effective approach in reducing cardiac symptoms and the rate of hospitalizations for HF.
From a single center, 71 patients with CRT and residual moderate-to-severe functional mitral regurgitation were treated with Mitraclip or with medical therapy alone.
At 24-month MitraClip patients presented lower rate of hospitalizations for heart failure (HF) than patients treated with only medical therapy. After adjustment for confounding factors, time to HF or death was significantly delayed in MitraClip group.
Heart failure, Functional mitral regurgitation, Cardiac resynchronization therapy, Mitraclip
Cardiac resynchronization therapy (CRT) is a recommended therapy for selected patients with systolic heart failure (HF) and intraventricular conduction delay [1]. Moderate-to-severe functional mitral regurgitation (FMR) occurs in approximately one-third of patients with HF referred to CRT and, although CRT therapy has been established as a treatment option in this cohort, significant FMR may persist or getting worse in approximately half of patients [2,3]. Over time, the increasing severity of FMR could be associated with adverse left ventricular remodeling and unfavorable outcome [4]. Furthermore, due to the advanced HF and a variety of concomitant comorbidities, surgical approach to FMR is often denied and patients non-responders to CRT can be managed with medical therapy alone or with less invasive percutaneous approaches [5,6].
Percutaneous mitral valve repair with the Mitraclip system (Abbott Vascular, Santa Clara, CA) has emerged as a feasible alternative to surgery for the treatment of symptomatic moderate-to-severe FMR [7]. The EVEREST trial and different registries showed safety, efficacy and favorable outcome of the MitraClip in selected patients. Recently, two different randomized trials studied the outcome of the MitraClip versus medical therapy alone in FMR, getting controversial results in light of the very different population recruited [8,9]. Particularly the American COAPT trial showed that transcatheter mitral valve repair compared to medical therapy alone in FMR obtained a lower rate of hospitalization for HF and all-cause mortality within 24 months of follow-up.
The treatment of moderate-to-severe FMR in CRT non-responders is feasible and reasonably effective in reducing cardiac symptoms and determining favorable cardiac remodeling, but previous studies in this field are limited by the lack of a control group and do not provide sustained information on long-term outcome of these patients [10,11].
Based on this issue, this study sought to evaluate the long-term outcome (i.e. 24-month) of CRT patients with moderate-to-severe FMR who underwent percutaneous treatment with the Mitraclip System or were managed with medical therapy alone.
We retrospectively analyzed patients who were referred to our Institution (Ferrarotto Hospital, Policlinico-Vittorio Emanuele, Catania, Italy) from June 2000 to May 2017 for the management of reduced ejection fraction HF. The institutional review board approval was given under the condition that the patients' data were collected in an aggregate and anonymized form.
In keeping with the ESC guidelines, patients underwent CRT if they had 1) New York Heart Association (NYHA) functional class III or IV despite optimal medical therapy, 2) Left ventricular ejection fraction (LVEF) ≤ 35%, and 3) QRS duration ≥ 130 ms, with left bundle branch block morphology [1]. Among patients with CRT, we retrospectively selected those with moderate-to-severe residual FMR, who represent the population of the present study. All patients were prescribed guideline-directed medical therapy, including maximum-tolerated doses of beta-blockers, angiotensin converting enzyme inhibitors or angiotensin receptor blockers, spironolactone and furosemide where appropriate. Clinical outcomes were then compared between patients who underwent Mitraclip therapy and those who were managed with medical therapy alone.
Clinical endpoints were defined according to the Mitral Valve Academic Research Consortium (MVARC) criteria [12]. The primary outcome of interest was the composite of all-cause death or cardiac hospitalizations for HF at 24-month follow-up. Secondary outcomes were all-cause death, re-hospitalization for HF and NYHA class at 24-month. Echocardiographic endpoints were assessed at 12-month, including parameters as LVEF, left ventricle end-diastolic and end-systolic volume, systolic pulmonary artery pressure and tricuspid regurgitation.
Follow-up data were obtained by scheduled clinical visits, echocardiographic assessment, and/or telephone calls at 30-day, 12-month and 24-month after the Mitraclip for the MitraClip group. The no-MitraClip group was studied in the same time window, as scheduled from the protocol of our Institute for patients with CRT. At each visit, the NYHA functional class was assessed. A standard echocardiographic examination was performed by two experienced echocardiographers, with FMR quantification as recommended by ASE/EAE guidelines [13,14].
Categorical and dichotomous variables are presented as counts and percentages and were compared by chi-square or Fisher's exact tests, as appropriate. Continuous variables are presented as mean ± standard deviation or median (interquartile range [IQR]) based on their distribution. Unpaired Student's t-tests were used to compare continuous parameters following a normal distribution, while Mann-Whitney U tests were used to compare continuous variables with skewed distribution. Categorical and dichotomous variables are presented as counts and percentages and were compared by chi-square or Fisher's exact tests, as appropriate. A p value of 0.05 was set for significance.
A paired sample T-Test was used to evaluate clinical and echocardiographic outcomes in alive patients from baseline to follow up at 12-month.
Survival curves were obtained using the Kaplan Meier method, and were compared using the log-rank test. Multivariable Cox regression survival analyses were used to identify the relationship between the study population and the occurrence of adverse events (i.e. death or hospitalization) during the follow-up. For the multivariate Cox analysis, covariates entered in the model were considered for potential prognostic impact, on an epidemiological basis; these covariates included chronic kidney disease, NYHA class, male sex. For all tests, a two-tailed p-value ≤ 0.05 was considered statistically significant. All data were processed using the Statistical Package for the Social Sciences version 21 (SPSS v21, Inc., Chicago, Illinois).
Of 71 patients with residual moderate-to-severe FMR in the study period, 40 (56.4%) patients were treated with the Mitraclip System (MitraClip group) and 31 (43.6%) patients were treated with medical therapy alone (no-MitraClip group) (Figure 1). Reasons for not performing the Mitraclip procedure in the 31 no-Mitraclip patients included: Refusal of the patient (n = 16; 51.6%), unfavorable anatomy (n = 8; 25.8%), high risk of peri-procedural infection due to previous history of infection or vegetation on leads (n = 3; 9.7%) or death before the procedure (n = 4; 12.9%).
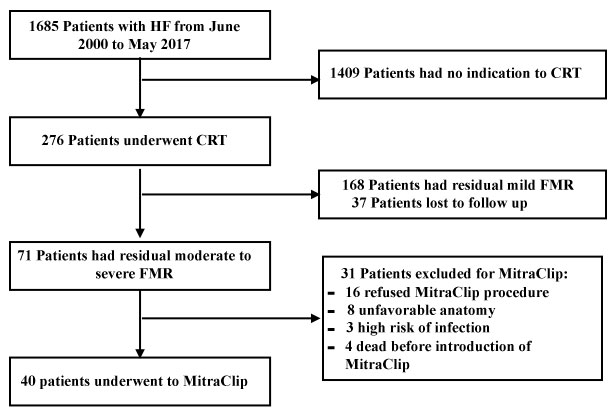 Figure 1: Flow Chart showing the patients included in the study. HF: Heart Failure; CRT: Cardiac Resynchronization Therapy; FMR: Functional Mitral Regurgitation.
View Figure 1
Figure 1: Flow Chart showing the patients included in the study. HF: Heart Failure; CRT: Cardiac Resynchronization Therapy; FMR: Functional Mitral Regurgitation.
View Figure 1
Baseline demographic characteristics of the study population and the MitraClip and no-MitraClip groups are summarized in Table 1. The majority of patients were male (69%) and the median age was 70 years (IQR 64-76). Forty-seven patients (66%) had idiopathic dilated cardiomyopathy and 36 (51%) presented chronic kidney disease. The median NYHA Class was III (IQR II-III) and only 9 (13%) patients were classified as CRT-responders. Criteria of CRT non-response were 1) No decrease of NYHA functional class; 2) Lack of an improvement of the left ventricular end-systolic volume of at least 10% after at least six months from the implantation of the device [15]. The median LVEF was 28% (IQR 24-35%). When comparing the two groups, the median patient age (MitraClip group 71.5 vs. no-MitraClip group 69 years, p-value 0.042) and the surgical risk score (STS mortality and morbidity, EuroSCORE II) were higher in the MitraClip group, as well as the proportion of male patients (MitraClip group 80% vs. no-MitraClip group 55%, p-value 0.023), chronic kidney disease (MitraClip 65% vs. no-MitraClip 32%, p-value 0.006), advanced NYHA class (III-IV) (MitraClip group 77.5% vs. no-MitraClip group 22.5%, p-value 0.000). In MitraClip group, LVEF was lower (MitraClip 25% vs. no-MitraClip group 30%, p-value 0.016) and left ventricle end-diastolic and end-systolic volumes were significantly larger than the no-MitraClip group. Patients in the no-MitraClip group significantly showed a higher prevalence of idiopathic dilated cardiomyopathy (n = 25; 80.6%).
Table 1: Baseline demographic characteristics of the overall population. View Table 1
Peri-procedural and in hospital outcomes after the MitraClip are shown in Table 2. MVARC technical success was reported in 37 patients (92.5%). The mean number of the implanted clips was 2 (IQR 1-2). Three peri-procedural complications were described: An episode of ventricular tachycardia interrupted by the intervention of the CRT-D; a laceration of the posterior leaflet of the mitral valve during the grasping maneuvers with consequent device failure; an iatrogenic fistula creation between the left atrium and the pulmonary artery, which was managed with a percutaneous occluder device. No in-hospital deaths were reported and the median length of stay was 4 days (IQR 2-6 days).
Table 2: Procedural outcomes and in-hospital outcomes after MitraClip System. View Table 2
30-day follow-up data were available for the overall population (100%). Death did not occur in anyone of the patients during the first month of follow-up. Conversely, hospitalizations for HF occurred in 6 patients (overall 8.4%; 2 patients in the MitraClip group and 4 in no-MitraClip group). No differences were noted in the NYHA class between the two groups (p-value 0.127; Figure 2). Moreover, no overstated modifications on LVEF were noticed during the follow-up, if compared to baseline (MitraClip group median LVEF 25% versus no-MitraClip group median LVEF 30%, p-value 0.033).
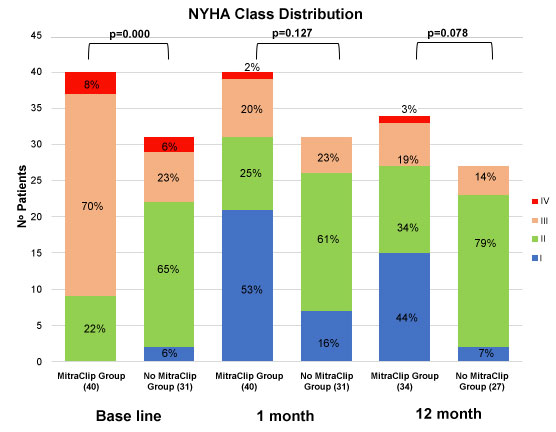 Figure 2: NYHA class distribution in the MitraClip Group and in the no-MitraClip Group at baseline, 30-day and 12-month of follow-up.
View Figure 2
Figure 2: NYHA class distribution in the MitraClip Group and in the no-MitraClip Group at baseline, 30-day and 12-month of follow-up.
View Figure 2
Data from 61 patients alive (86%) were available at 12-month follow-up. As shown in Table 3, there was no statistically significant difference in mortality between the two groups of study: 6 patients (15%) in MitraClip group vs. 4 patients (12.9%) in no-MitraClip group (p-value 0.801). Hospitalizations for HF occurred in 23% of MitraClip patients vs. 32% of no-MitraClip patients (p-value 0.36). Furthermore, there were no differences in term of NHYA class between MitraClip and no-MitraClip patients (p-value 0.078), although, in MitraClip group, paired evaluation in 34 patients alive at 12-month follow-up showed a significant improvement of NHYA class from baseline to 12-month (p-value ≤ 0.001), as shown in Table 4.
Table 3: Follow-up at 30 days and 12-month. View Table 3
Paired echocardiographic assessment in patients with complete echocardiographic data available at 12-month follow-up showed that LVEF, left ventricle end-diastolic volume and left ventricle end-systolic volume did not significantly differ from baseline to 12-month follow up (Table 4).
Table 4: Paired sample T-Test between 34 patients alive in MitraClip group and 27 alive in no-MitraClip group at 12-month follow up: Clinical and echocardiographic outcome. View Table 4
Kaplan-Meier freedom from all-cause death is depicted in Figure 3A. As shown, no differences between the two groups of study at 24-month were recorded (log rank p-value 0.825). Figure 3B confirms that the no-MitraClip group presented an increased risk of hospitalizations for HF (log rank p-value 0.048). Moreover, there was not significant difference regarding the primary endpoint at 24-month (Figure 3C; p-value 0.32ss5).
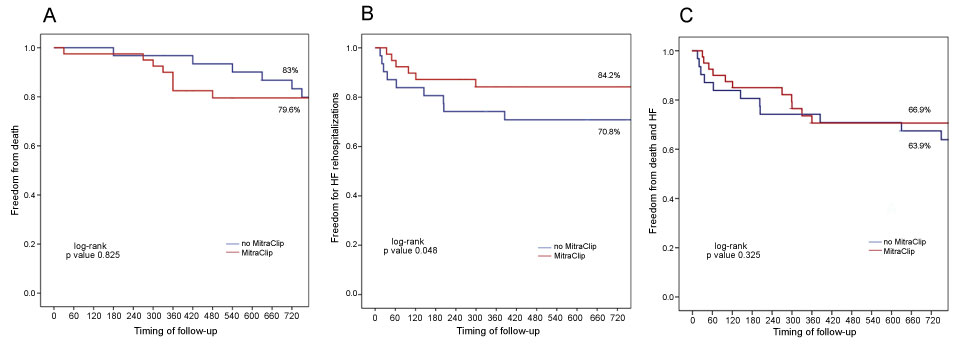 Figure 3: Kaplan Maier curves: A) 24-month freedom from all-cause death; B) 24-month freedom from HF hospitalizations; C) 24-month freedom from the composite of death and HF (primary endpoint). HF: Heart Failure.
View Figure 3
Figure 3: Kaplan Maier curves: A) 24-month freedom from all-cause death; B) 24-month freedom from HF hospitalizations; C) 24-month freedom from the composite of death and HF (primary endpoint). HF: Heart Failure.
View Figure 3
After adjustment for predefined covariates (including chronic kidney disease, NYHA class and male sex), the incidence of hospital stay for HF or death was significantly delayed in MitraClip group (HR: 0.38; p-value 0.018), confirming that chronic kidney disease, NYHA class and male sex were all independent predictors of long-term outcomes (Figure 4).
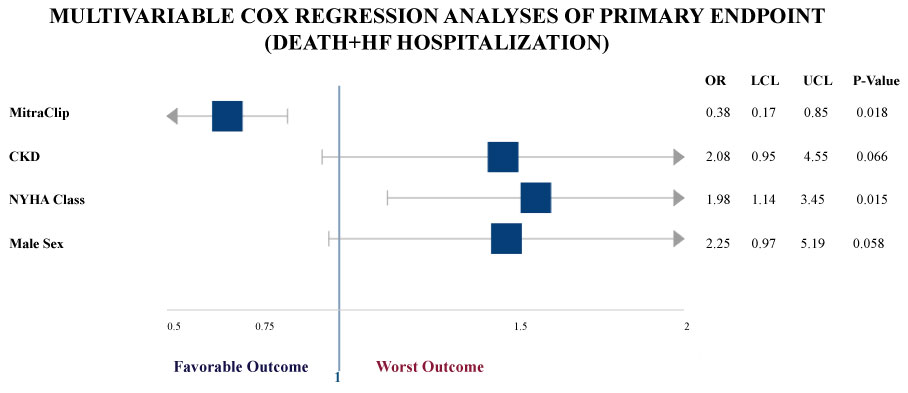 Figure 4: Forest Plot of the multivariable Cox regression analysis identifying covariates of prognostic impact for primary endpoint (composite of death and heart failure hospitalizations), on an epidemiological basis. CKD: Chronic Kidney Disease; OR: Odds Ratio; LCL: Lower Confidence Limit; UCL: Upper Confidence Limit.
View Figure 4
Figure 4: Forest Plot of the multivariable Cox regression analysis identifying covariates of prognostic impact for primary endpoint (composite of death and heart failure hospitalizations), on an epidemiological basis. CKD: Chronic Kidney Disease; OR: Odds Ratio; LCL: Lower Confidence Limit; UCL: Upper Confidence Limit.
View Figure 4
The present study aimed to evaluate the long-term outcome (i.e. 24-month) of symptomatic patients with CRT with residual moderate-to-severe FMR who were treated with the MitraClip system or managed with medical therapy alone in a single-center experience. The main finding of this analysis showed that patients treated with the MitraClip System presented lower rate of adverse events (i.e. hospitalization for HF) during a limited period of follow-up, if compared to no-MitraClip patients. Moreover, at 12-month follow-up, the MitraClip group presented a significant improvement of NYHA functional class from baseline. After statistical adjustment for the main epidemiological factors that impact on prognosis, the MitraClip therapy resulted a protective factor against the primary endpoint.
Patients with severely reduced LVEF and FMR are the main focuses of this analysis. FMR is a condition extremely frequent in patients with impaired LVEF, due to the adverse left ventricle remodeling and consequent tenting forces on mitral valve, which are responsible for insufficiency [16,17]. Higher degree of FMR after CRT is a strong predictor of all-cause death and hospitalization for HF at 3 years [18].
In this context it has been demonstrated that MitraClip System in CRT non-responders is a feasible and safe approach and it has showed to increase LVEF, reducing left ventricular volumes [10], with favorable remodeling at mid-term follow-up [11], and to reduce NT-pro BNP levels and tricuspid regurgitation pressure gradient in HF conditions [10]. Two recent trial compared transcatheter mitral-valve repair with medical therapy alone in symptomatic patients with HF with opposite results: In the COAPT study the transcatheter mitral-valve repair compared to medical therapy resulted in a lower rate of all-cause deaths and HF hospitalization within 24 months of follow-up, while MITRA-FR investigators showed no differences in death and HF hospitalization between the two group at one year [8,9].
Based on these evidences, in our analysis, we sought to evaluate the impact of MitraClip versus medical therapy alone on the outcome of a cohort of patients previously treated with CRT and with residual moderate-to-severe FMR in a real-world setting. As per protocol of our Institute and according to the current guidelines, all the CRT patients recruited retrospectively for this study received the maximum tolerated dose of medical therapy for HF. Apart from the patients who died before the introduction of the MitraClip at our Institute and were managed only with medical therapy, all the patients were proposed for the MitraClip procedure and this intervention was denied just in case of absolute or relative contraindications or refusal of the patient.
From this initial analysis, we interestingly noticed that, at baseline, the MitraClip group did not typically present the favorable demographic characteristics of the CRT responder population. Indeed, in the MitraClip group we can register a higher prevalence of men with history of ischemic cardiomyopathy, whereas female sex and non-ischemic cardiomyopathy generally showed an increased responsiveness to CRT. If we also add that the MitraClip group presents a higher surgical risk profile according to the comorbidities presented and advanced symptoms in terms of higher NYHA class, it's interesting to notice that the MitraClip group showed a more favorable outcome in term of hospitalizations for HF during the follow-up, if compared to the no-MitraClip group, although no differences in primary endpoint and all-cause mortality were detected between the two groups at 24-month.
As regards the peri-procedural outcome of the MitraClip group, all the clips were deployed with low rate of complications (7.5%) and the technical success in these patients was in line with the results of the GRASP registry, which were previously published [20]. All the procedural complications were promptly managed and no in-hospital deaths were reported. The device time in the MitraClip group (i.e. median 49 minutes, IQR 29-75) was similar to the updated device time of the overall population of the GRASP registry (i.e. median 51 minutes, IQR 30-75), showing that the presence of an electronic device such as CRT does not impact on the technical aspect of the procedure itself. Another interesting point is that the MitraClip group required a larger number of clips (i.e. median 2) if compared to the overall population of the GRASP registry (i.e. median 1) [20]. A possible explanation of this finding could be that, patients with larger ventricle volumes, more sever annular dilatation and increased tethering forces leading to malcoaptation of the scallops require more clips to get a satisfactory result, if compared to FMR with better left ventricle function or degenerative mitral regurgitation.
Despite the small number of patients recruited in this study, our results from real clinical practice confirm the feasibility and effectiveness of the MitraClip procedure in a cohort of high-risk patients with severe left ventricle dysfunction, suggesting that when appropriate, according to the anatomical and clinical features, this procedure should be routinely proposed.
The favorable results of the MitraClip in term of improvement of NYHA functional class and MR reduction remained sustained during the 30-day and 12-month follow-up, and the difference in term of left ventricle volumes and left ventricle dysfunction, that were statistically significant between MitraClip group and no-MitraClip group before the MitraClip procedure, were smoothed. The incidence of death at 30-day and 12-month was low and not statistically significant between the two groups of study. During the follow-up, the MitraClip group presented a significant improvement in NYHA functional class and a mild, but not significant, favorable left ventricle reverse remodeling, with a leveling in the echocardiographic differences between the two study groups from baseline to the 12-month follow-up. Reverse left ventricle remodeling after CRT and MitraClip has been described in literature [10, 11] and this event seems to be related to a better outcome during the follow-up.
Another critical result is that the MitraClip group, if compared to no-MitraClip group, showed a lower rate of hospitalizations for HF in a 24-month Kaplan-Meier analysis and the Cox Proportional-Hazards Model strengthened this evidence, showing that MitraClip was protective against the primary composite endpoint.
These results are in line with studies that show that MitraClip helps to reduce the hospitalizations rate for HF and improve quality of life [8,20,21]. Frequent hospitalizations are associated with a worse long-term outcome and significant increase in HF-related health costs. Furthermore, it was observed that at every hospital readmission, the quality of life of patients declines [22].
Of course, several limitations should be considered inherent to our study, by the virtue of its observational nature. This single-center study included a small number of patients and there are significantly baseline difference between the two groups compared. So the results should not be generalized and further, larger multicenter studies are needed to confirm these exploratory results.
In CRT patients, the treatment of moderate-to-severe FMR with the Mitraclip System - if compared to medical therapy alone - is a feasible, safe and reasonably effective approach in reducing cardiac symptoms and the rate of hospitalizations for HF.
Carmelo Grasso is a proctor physician for Abbott Vascular.
Davide Capodanno received consulting and speaker's honoraria from Abbott Vascular.
Corrado Tamburino received speaker's honoraria from Abbott Vascular.
All other authors have no conflicts of interest to declare.