Decompression followed by enucleation of Keratocystic odontogenic tumour (KCOT) is a recommended conserva-tive approach for large KCOT to prevent injury to the surrounding vital structures, pathological fracture of the mandible and radical resection surgery. On the other hand, this approach necessitates multiple surgical procedures and prolonged follow-up which depends on the patient's compliance and may increase the risk of infection.
A 42-year-old male presented with large right mandibular angle KCOT associated with impacted wisdom tooth. Decompression, incisional biopsy, and extraction of wisdom tooth were performed under Local anaesthesia. CBCT, 3 and 6 months post-operatively demonstrated obvious reduction of cystic cavity which allowed for enucleation of KCOT followed by Carnoy's solution application under GA with minimal complications.
Decompression of large KCOTs followed by enucleation with peripheral ostectomy or chemical therapy is viable treatment option to avoid invasive resection surgical procedure.
The keratocystic odontogenic tumour (KCOT) is a benign and locally aggressive tumour [1] derived from dental lamina [2]. Currently, enucleation and decompression are the two common treatment options [3]. Due to the prob-lems associated with radical treatment, decompression has been proposed as a more conservative treatment, despite the need for periodic follow-ups [4]. Decompression of KCOT is a simple method for stimulating new bone formation due to the reduction in cystic pressure by creating a hole that connects the cystic cavity with the oral cavity which allows cystic fluid to evacuate [5]. Therefore, decompression should be considered when KCOT enlarges and approaches vital structures or weaken the jaw.
Treatment options for KCOT should take into account a variety of criteria, including the patient's age, the size and location of the cyst, soft tissue involvement, past treatment history, and the histological variant of the lesion [6]. The objective is to select the modality of treatment that eliminates the lesion with the least possibility of morbidity and recurrence risk.
Large multinucleated KCOT that include soft tissue involvement and cortical bone perforation, as well as lesions that have already recurred after receiving conservative therapy, should be resected to the adjacent anatomic boundary [7]. On the other hand, it has been reported that decompression of large KCOT that have not yet perforated the cortical bone followed by peripheral ostectomy with or without chemical therapy has had positive results [8].
A 42-years-old male was referred to the Oral and maxillofacial surgery department at Najran general hospital (Saudi Arabia) following an accidental finding of a large right mandibular angle cystic lesion during a routine check by his dentist. He smokes a pack of cigarettes per day for the last 25 years, otherwise, he is fit, healthy and not on any regular medication. On examination, there was no facial swelling, Inferior alveolar and lingual nerves were intact bilaterally. There was no evidence of intra-oral swellings or sinus tract. Teeth at quadrant four are vital and stable with no mobility. CBCT demonstrated an inverted impacted 48 associated with a unilocular, well-demarcated radiolucent lesion, extending from 46 to the right mandibular angle with a size of 36 × 30 × 16 mm (Figure 1 and Figure 2). There was no obvious root resorption, and the inferior alveolar canal was at the Bucco-inferior border of the lesion. Aspiration revealed a keratin content of the cystic lesion.
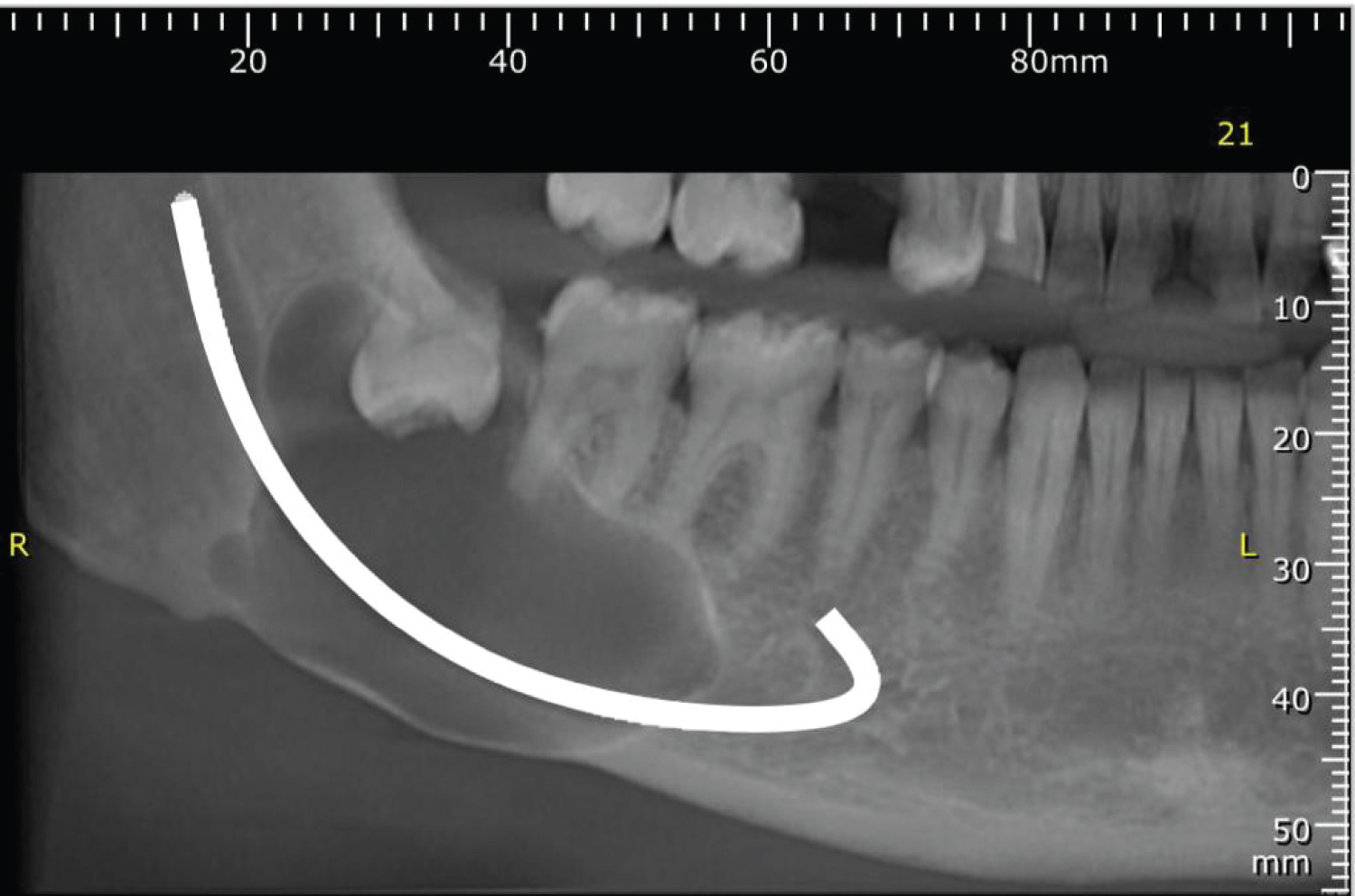 Figure 1: Preoperative CBCT.
View Figure 1
Figure 1: Preoperative CBCT.
View Figure 1
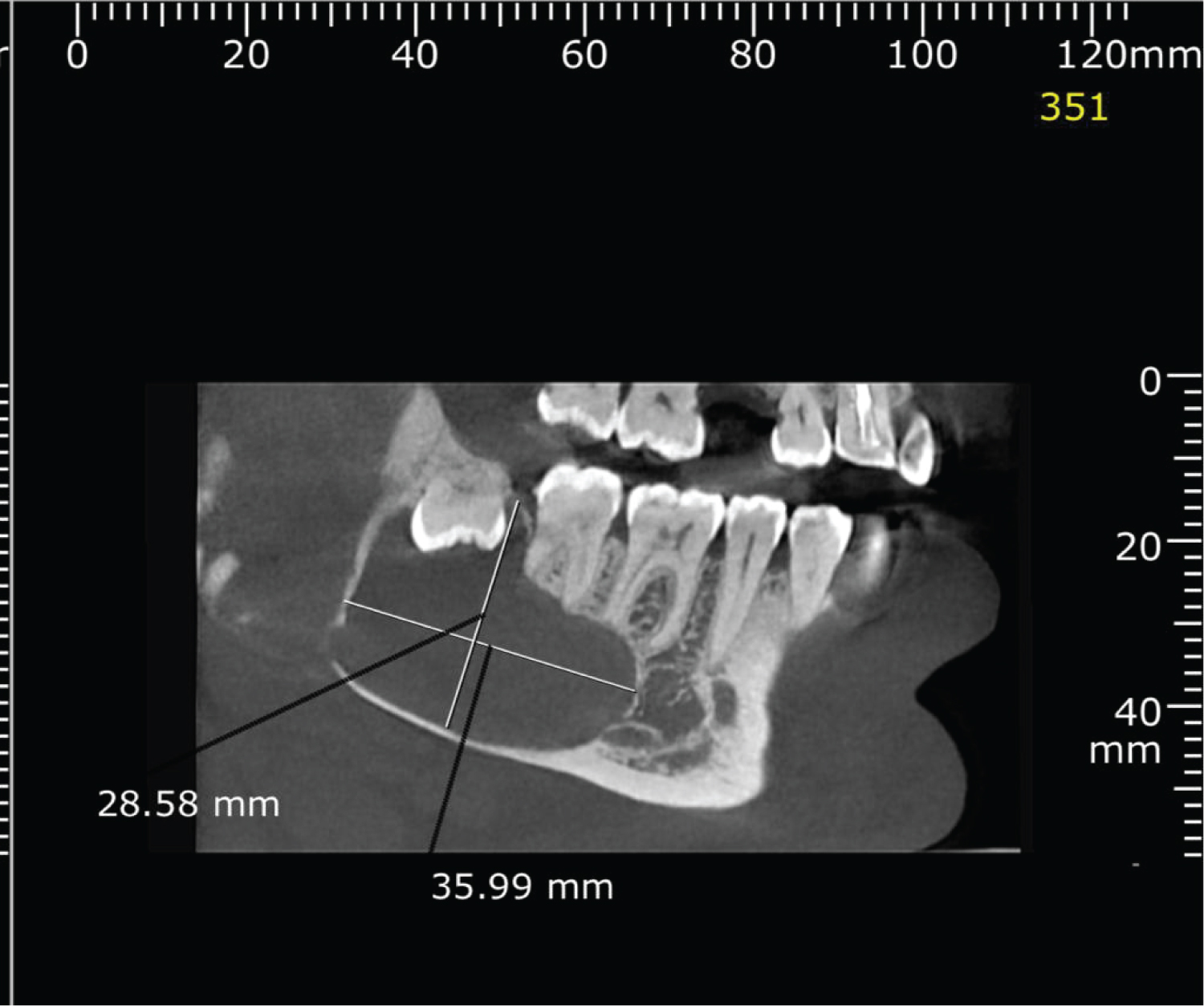 Figure 2: Preoperative CBCT.
View Figure 2
Figure 2: Preoperative CBCT.
View Figure 2
The patient consented to the extraction of 48, decompression and incisional biopsy. Surgical removal of 48, decom-pression using a nasopharyngeal airway tube (NPT) and incisional biopsy were performed under Local anaesthetic without complications. The histopathology confirmed ortho-keratinized OKC. CBCT was done 3 months postoperatively (Figure 3), demonstrating bone deposition at the periphery of the cystic lesion. The size of the lesion decreased to 30 × 23 × 13 mm. Therefore, the NPT was replaced with a shorter one. CBCT, 6 months post-operatively (Figure 4) revealed a further decrease in the lesion size to 26 × 18 × 11 mm. This was followed by the enucleation of the lesion under GA and the application of Carnoy's solution. Postoperatively, the patient complained of right lower lip paraesthesia which is completely resolved 6 weeks later. Follow-up was arranged for the patient at 3 and 6 months for further radiological imaging to assess the progress of healing of the cystic cavity and the possibility of recurrence.
 Figure 3: 3-month postoperative CBCT.
View Figure 3
Figure 3: 3-month postoperative CBCT.
View Figure 3
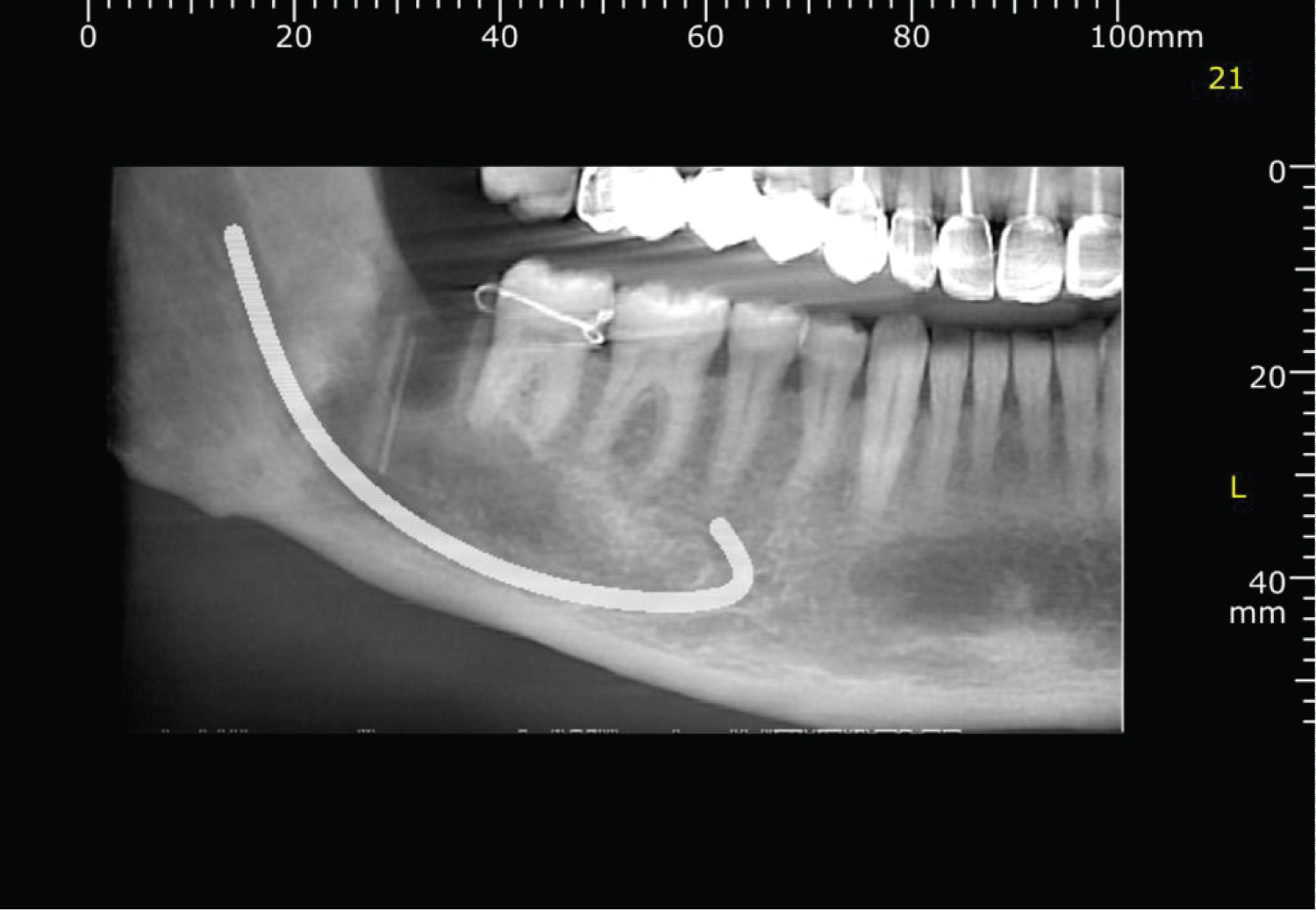 Figure 4: 6-month postoperative CBCT.
View Figure 4
Figure 4: 6-month postoperative CBCT.
View Figure 4
KCOT is a common odontogenic entity that requires specific treatment due to its aggressive behaviour and propen-sity to recur [9], with a male-to-female ratio of 2:1 and a predilection for the posterior mandible, which is involved in 65% to 83% of cases. KCOTs are most prevalent in the second, third, and fourth decades of life (54.2%) [10]. KCOT has a scalloped contour on radiographs and appears as uni or multilocular radiolucency [11].
In contrast to typical cysts, KCOT displays distinctive growth and biological behaviour, with the growth being caused by the active proliferation of the epithelial lining. The majority of commonly occurring cysts grow due to the osmotic pressure of the cystic fluid. The expansion of the buccal and lingual cortical plates is caused by this expan-sile type of growth. KCOT, on the other hand, behaves like a benign tumour that grows through extension rather than expansion. The osmotic pressure of the cystic fluid is quite low with KCOT, therefore, the extension follows the route of least resistance which is the cancellous bone, consequently, KCOT grows antero-posteriorly, with no evidence of cortical expansion in the early stages [12,13].
Jaw cysts can be treated surgically using one of three methods: enucleation, marsupialization, or decompression [14]. KCOTs have a high recurrence rate due to thin epithelium lining, daughter cysts, collagenase activity of the cyst and incomplete removal of cyst lining. Therefore, many surgical procedures have been attempted for the treat-ment of KCOTs. In the multilocular situation, a complete removal is quite difficult [15]. Some authors have sug-gested radical surgery, such as resection and the Brosch technique, to lower the high recurrence rate [16].
Resection of large KCOT can compromise function and aesthetics. Therefore, decompression and second-stage enucleation is the best choice when a cyst is large and close to critical anatomical structures in order to preserve the neighbouring teeth, the inferior alveolar canal, and the maxillary sinus. By releasing the intracystic pressure, the cyst's size is reduced, which can allow impacted teeth to erupt and the growth of new bone [6,14,17]. Due to the aforementioned benefits, the treatment protocol for a large KCOT has recently been modified to adopt this conservative approach [14,18]. The drawbacks of decompression include that it necessitates two surgical proce-dures, takes more time [8], has a higher recurrence rate than surgical resection [16], uncomfortable to patients, necessitates their compliance, and poses a danger of infection. During the decompression process, a window is maintained open by packing the cystic cavity or, more frequently, by suturing a device (tube, stent) to its periphery. This allows for the drainage of fluids out of the KCOT. In our case, decompression was accomplished via NPT. It was founded on the rationale that releasing the intramural pressure would cause the cysts to shrink through progressive bone development from the periphery [17].
Typically, resection of KCOT is indicated for lesions that have recurred following several "conservative" surgeries and in cases where the KCOT is no longer contained in the bone where there is soft tissue involvement and perfora-tion of the bony cortex, with the potential to affect critical structures including the orbit and lateral skull base [19].
In this case report, decompression of KCOT with subsequent enucleation and Carnoy's application was adopted choice of treatment to spare the patient the dramatic consequences of resection. Following decompression for 6 months of KCOT, there was a large reduction in cystic cavity size and obvious bone deposition at the mandibular lower border which allows for enucleation of KCOT and application of Carnoy's solution with minimal complica-tions.
There have been various studies on the differences in recurrence based on KCOT treatment methods. Resection is the most efficient method to avoid the recurrence of KCOT, however, this is a very invasive surgical operation. Simple enucleation was reported to have a recurrence rate of 17% to 56% in a review study of KCOT by Blanas, et al. [20]. The likelihood of a KCOT simple enucleation recurring is very high. However, there are numerous studies indicating a low recurrence rate after decompression following enucleation of OKC with peripheral ostectomy or application of Carnoy's solution (0-8.7%) [6,14].
Decompression of large KCOTs followed by enoculation with peripheral ostectomy or chemical therapy is viable treatment option to avoid invasive resection surgical procedure.
All authors disclose no conflicts.
|
Authors |
Conception and design of study/review/case series |
Acquisition of data: laboratory or clinical/literature search |
Analysis and interpretation of data collected |
Drafting of article and/or critical revision |
Final approval and guarantor of manuscript |
|
Mohamed Elseyoufi |
Yes |
Yes |
Yes |
Yes |
Yes |
|
Ayman Hasan Alrabiaa |
No |
Literature search |
No |
Drafting article |
No |
|
Peter Tsakiris |
No |
No |
No |
Critical revision |
Yes |