Aim: To assess the effect of moderate procedural sedation and opioid analgesia in the incidence of radial artery spasm during trans-radial coronary interventions.
Methodology: A Prospective randomized controlled study conducted in the department of Cardiology in a tertiary care hospital in South India. The study included patients undergoing diagnostic coronary angiography and percutaneous coronary intervention (PCI) with trans-radial access. Patients were randomized to either administration of sedation and analgesia (Treatment group) or no procedural sedative/analgesic (Control group). In the treatment group, Inj. Fentanyl 0.5 mcg/kg and Inj. Midazolam 1 mg slow intravenous over 2 minutes were administered at the beginning of the procedure. The incidence of spasm was the primary end point. Visual Analogue Scale (VAS) was used to assess the patient discomfort. The pain score was assessed immediately and 6 hours post-procedure. Statistical analysis was done using SPSS software and Pearson Chi square test to compare the treatment and control groups.
Results: A total 400 patients were enrolled in the study. Among the 29 patients with spasm, 21 were from the “No treatment” group whereas only 8 patients were from the “Treatment group”. i.e., 10.5% patients from the “No treatment” group had spasm while only 4% of patients from the “Treatment group” had spasm which is statistically significant (p = 0.021). The predisposing factors for the incidence of radial artery spasm were systemic hypertension, dyslipidemia, and previous history of radial artery catheterization.
Conclusion: Administration of opioid analgesia and benzodiazepines combination before the procedure significantly reduced the incidence of radial artery spasm.
Trans-radial, Coronary intervention, Radial artery spasm, Opioid analgesia, Sedation
The trans-radial approach for coronary interventions has emerged as a widely accepted alternative globally to the traditional femoral approach [1]. It is accepted based on evidence that trans-radial interventions are associated with decreased vascular complications and in-hospital stay for patients [2,3]. Also, in certain group of patients like patients with acute coronary syndromes, trans-radial approach is found to have been associated with better procedural outcomes [4,5].
Among all the coronary interventions, only 1.3% of the procedures are performed through trans-radial access. There are considerable benefits with reduction in patient discomfort, early mobilization of the patient following the procedure, reduced procedure cost etc.
Majority of the complications and difficulties during trans-radial intervention is related to the spasm of the radial artery triggered by the sheath or catheter insertion into the radial artery.
It is in this context we proposed our study to evaluate the role of moderate procedural sedation with opioid analgesia and benzodiazepines in preventing radial artery spasm.
To assess the effect of moderate procedural sedation and opioid analgesia in the incidence of radial artery spasm during trans-radial interventions.
This is a prospective randomized controlled study conducted after getting approval from the Institutional Human Ethics Committee. The study was conducted in the department of Cardiology, in a tertiary care hospital in South India. All patients included in the study were explained in detail about the study and its purpose. Informed consent was obtained from the patients before the procedure.
All prospectively recruited patients undergoing diagnostic coronary angiography and PCI with trans-radial access in the department of Cardiology.
Patients with history of acute coronary syndrome (ACS) within the past two weeks, cardiogenic shock, end stage renal disease, severe hepatic impairment (Child-Pugh class C), patients with chronic opioid or benzodiazepine use, patients with known peripheral artery disease of upper limbs and patients with a history of hypersensitivity to opioids or benzodiazepines.
Patients were randomized in the ratio of 1:1 to either administration of sedation and analgesia (Treatment group) or no procedural sedative/analgesic treatment (Control group). In the treatment group, Inj. Fentanyl 0.5 mcg/kg and Inj. Midazolam 1 mg slow intravenous over 2 minutes were administered at the beginning of the procedure (during preparation of the access site). One additional dose was allowed 45 to 60 min after the first one. Respiration and oxygen saturation were constantly monitored.
The right radial artery was cannulated as a default following a local infiltration of anaesthetic agent (subcutaneous lidocaine solution 2 mg). After radial sheath was placed, the routine cocktail of Inj. Nitroglycerine 100 mcg + Inj. Diltiazem/Inj. Verapamil 5 mg IV and Inj. Heparin 40 units/kg IV bolus was administered through the sheath to patients in both the groups. Post-procedure haemostasis was attained by applying dynaplast compression bandage.
Visual Analogue Scale (VAS) was used to assess the patient’s discomfort. The pain score was assessed immediately after the procedure and 6 hours post-procedure.
The incidence of spasm was considered as the primary end point. Spasm was confirmed arteriographically as severe narrowing/constriction of the radial artery lumen. The secondary end points were TIMI (Thrombolysis In Myocardial Infarction trial) major bleeding during stay in the hospital, any complications intra-procedure, allergic reactions, 30 day mortality and morbidity.
Statistical analysis was done using SPSS software. Descriptive statistics were expressed as numbers and percentages. Pearson Chi square test was done to compare the significance between treatment and control groups. P value < 0.05 was considered statistically significant.
According to our study, the primary end point of incidence of radial artery spasm was found to be significantly lesser among patients in the “Treatment group” when compared to the patients in “No treatment” group. A total of 29 patients among 400 patients enrolled in the study had radial artery spasm. Among the 29 patients with spasm, 21 were from the “No treatment” group whereas only 8 patients were from the “Treatment group”. i.e., 10.5% patients from the “No treatment” group had spasm while only 4% of patients from the “Treatment group” had spasm which is statistically significant (p = 0.021). This indicates that spasm occurred significantly less in patients who received the opioid analgesia and benzodiazepines combination before undergoing the procedure (Table 1).
Table 1: Overall incidence of spasm. View Table 1
While analyzing the impact of the other variables of the patient population on the primary end point (Incidence of radial artery spasm), we found that out of the 29 cases of spasm 16 (55%) patients were females which was statistically significant with P value 0.008. This showed that predominantly female patients had spasm.
Out of the 29 patients who had spasm, 25 (86%) were hypertensives which was statistically significant with p < 0.05. According to our study shows that hypertensives were significantly more susceptible for developing spasm during radial interventions than non-hypertensives (Table 2 and Figure 1).
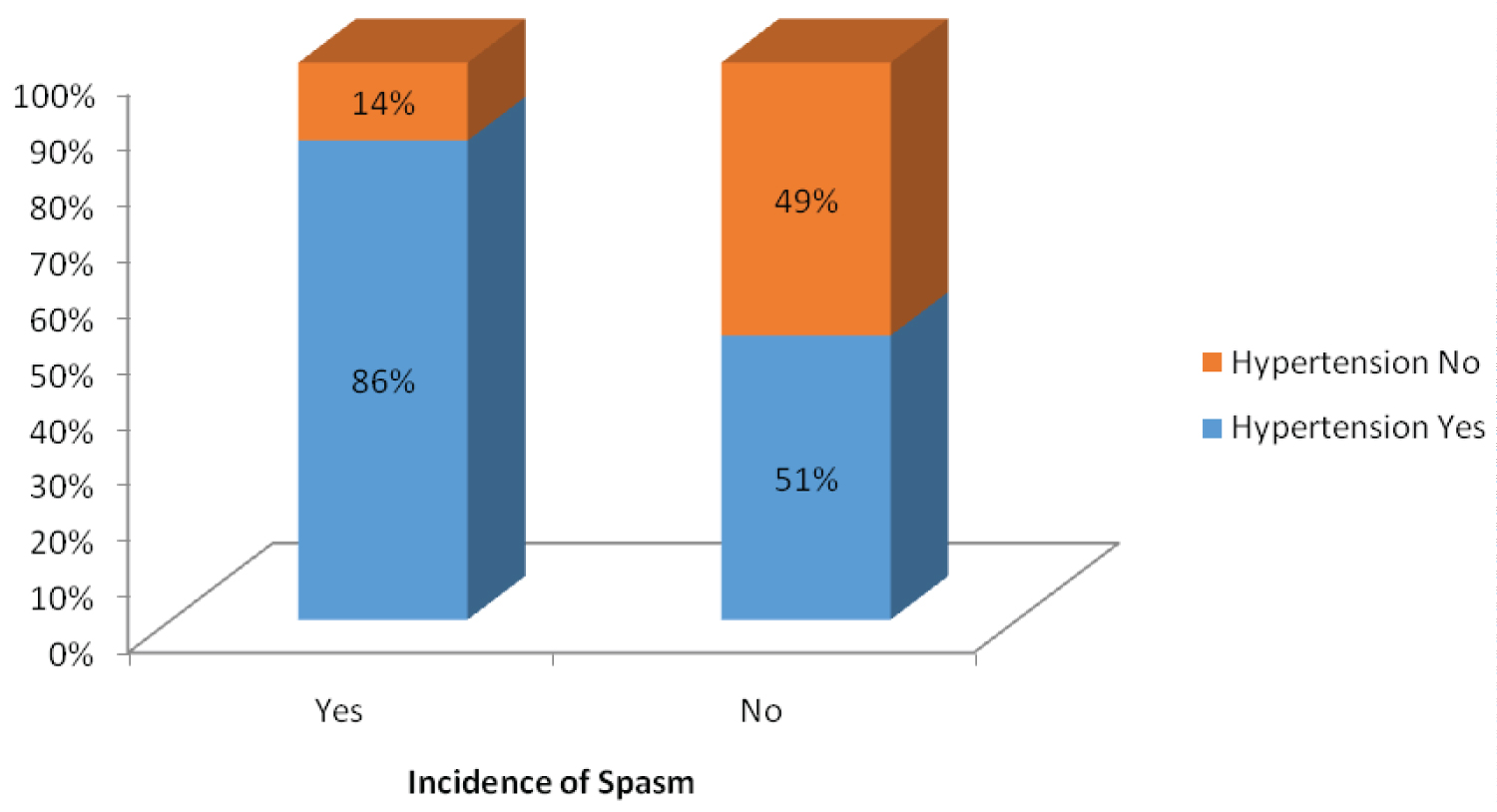 Figure 1: Incidence of spasm in hypertensives.
View Figure 1
Figure 1: Incidence of spasm in hypertensives.
View Figure 1
Table 2: Incidence of spasm in hypertensives. View Table 2
Similarly, out of the 29 patients who had spasm during procedure, 20 (69%) patients had dyslipidemia which was statistically significant at p < 0.05. This shows that dyslipidemia could be a factor that can predispose to developing spasm during radial interventions (Table 3 and Figure 2).
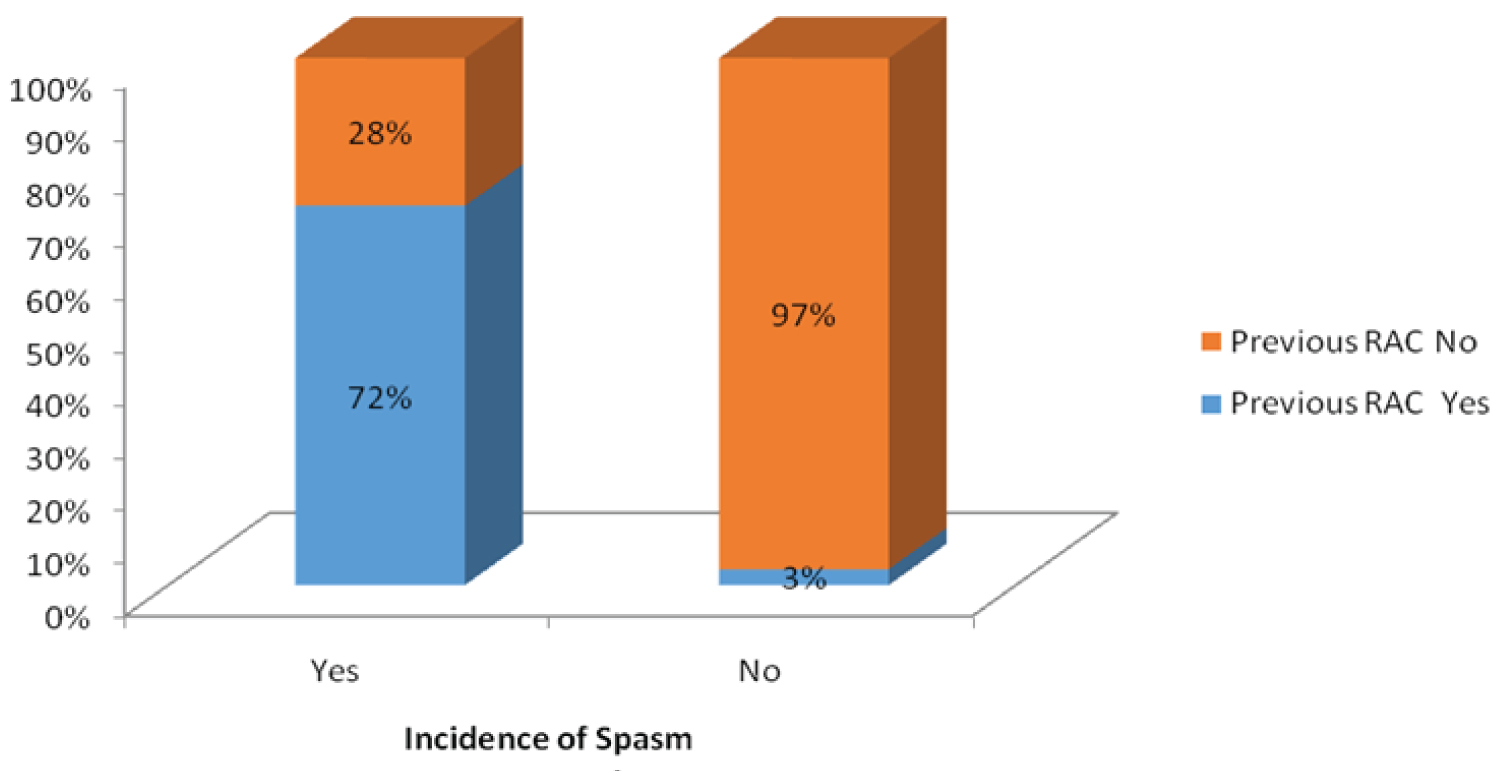 Figure 2: Incidence of spasm in patients who had previous radial artery catheterization.
View Figure 2
Figure 2: Incidence of spasm in patients who had previous radial artery catheterization.
View Figure 2
Table 3: Incidence of spasm in patients who had previous radial artery catheterization. View Table 3
Association of other variables like type II Diabetes, peripheral artery disease, renal dysfunction and smoking were found to be statistically insignificant in predisposing to spasm.
Another important factor which was very concerned regarding doing radial interventions is the amount of pain perceived by the patient due to the procedure. For this, a visual analogue scale (VAS) scoring system was used in which patients describe/quantify the pain perceived by them as a score between 0 to 10 with 0 meaning that there was no pain and 10 corresponding to extreme pain.
We divided the patients who perceived pain into three categories - Those who had a pain score of 1 to 3 as Mild discomfort, 3 to 6 as moderate discomfort and more than 6 as severe discomfort. And we took the VAS scoring from patients at three time periods - before procedure, immediate post-procedure and 6 hours post-procedure.
Significant number of patients from the “Treatment group” had only Mild discomfort during the immediate post-procedure period. However, most of the patients from both the “Treatment group” as well as the “No Treatment” had only mild discomfort or no pain at all at the 6 hours post-procedure period. Thus, according to our study, we noticed that administration of moderate procedural sedation with benzodiazepines and opioid analgesia considerably reduced the immediate post-procedure pain/discomfort for the patients (Table 4).
Table 4: Difference in the immediate post-procedure pain score (visual analogue scale). View Table 4
Access site cross-over, i.e., needing to change the approach to the procedure from radial route to elsewhere (viz. the other radial artery, brachial or femoral routes) was seen more commonly with patients in “No Treatment” group. The most common reason behind access site cross-over being radial artery spasm.
A total of 12 patients in the entire study population had access site cross-over among which 10 (5%) patients were from the “No Treatment” group whereas only 2 (1%) patients were from the “Treatment Group”. This showed that there were a statistically significant number of patients from the “No Treatment” group who needed access site cross-over predominantly due to radial artery spasm. Other reasons for access site cross-over were difficult anatomy of the radial artery and/or the coronary sinuses, increased tortuosity in the course of the artery etc.
The increased tendency of the radial arteries to go into spasm may be attributed to the characteristic morphology of its vessel wall which has a marked muscle mass which is significantly more than the other arteries and the high density of alpha - adrenergic receptors in the radial artery [6,7].
It is estimated about 15 to 30 % of trans-radial interventions lead to this complication [8]. One other major concern about radial artery spasm is that it may lead to perforation of the vessel.
Some of the major advantages of the trans-radial approach are lower rates of access related complications, early mobilization of the patients, shorter in-hospital stays, less patient discomfort over-all [3,4,9,10].
Increased incidence of access site cross-over has been reported during trans-radial access due to radial artery spasm. Hence preventive measures are being carried out to avoid the radial artery spasm, the common ones being the administration of the routine vasodilator cocktail [11-14] of Inj. NTG + Inj. Verapamil/Inj. Diltiazem after insertion of the radial sheath [15,16].
The combination of opioid and benzodiazepines help prevent radial artery spasm in more than one mechanism, namely their sedative and analgesic effect and direct vasodilatory effects. This has been studied in detail and published by Gursoy, et al. [17,18].
Our study has shown that the use of Moderate Procedural Sedation prior to radial interventions causes statistically significant reduction in the incidence of radial artery spasm. Apart from this, we also observed that the incidence of spasm is more common among female patients when compared to males.
According to our study, the other variables which were found to be predisposing to the incidence of radial artery spasm among people undergoing radial interventions are systemic hypertension, dyslipidemia and previous history of radial artery catheterization for any reason.
A similar randomized open label prospective study carried out in Greece reported incidence of spasm in 2.6% of patients in the treatment group, whereas it was reported in 8.3% of patients in the no-treatment group which was similar to the current study.
Other predisposing factors for the development of spasm were female sex and smoking according to this study. Spasm more frequently occurred in patients who underwent combined coronary angiogram and percutaneous trans-catheter coronary angioplasty procedure (PTCA).
According to a meta-analysis, the success rate for PCI through trans-radial approach was found to be similar to that of the femoral route. There was significantly less puncture site complications in patients undergoing trans-radial intervention when compared to femoral interventions [19].
Caroline Birgy, et al. studied the effect of inhalational sedation and opioid analgesia on pain and spasm of radial artery during coronary angiograms in trans-radial approach. They observed that inhalational sedation with a mixture of nitrous oxide and oxygen was equally safe and effective as opioid analgesia [20].
From the current study it was evident that routine administration of low dose opioid analgesia and procedural sedation can significantly bring down the incidence of radial artery spasm and thereby avoiding the deadly complications related to radial artery spasm.
The population who was at relatively more risk for development of radial artery spasm were females, hypertensives, dyslipidemics and patients who had undergone previous radial artery catheterizations.
Apart from reducing the incidence of spasm, the regime of procedural sedation and analgesia also reduced the immediate post-procedure pain experienced by the patient.
It was observed from the current study that it is beneficial to use opioid analgesia and benzodiazepine sedation prior to procedure to reduce the incidence of radial artery spasm during trans-radial coronary interventions. It was also evident that hypertensives, patients with dyslipidemia and a history of previous radial artery catheterization were more prone for spasm. Hence the practice of giving opioid analgesia and moderate sedation prior to trans-radial coronary interventions could be considered for the benefit of the patient.
The authors thank all the Cath lab technicians and staff nurses who have supported and assisted the coronary interventions.
The authors did not have any conflict of interest.
This research was not funded by any funding agency.