Kawasaki disease is an acute, self-limited vasculitis of unknown etiology that occurs predominantly in infants and young children. It is now the most common cause of acquired heart disease in children in developed countries.
The long-term sequelae of KD represent a consequence of the inflammatory damage which occur in the acute phase, particularly involving the coronary arteries. The possible vascular complications include coronary artery aneurysms (CAAs), thrombosis or stenosis, which then can lead to acute myocardial infarction or chronic ischemic disease. About 25% of untreated KDs complicate with CAAs [1], and up to 5% of those treated with IVIGs [2]. Besides, there is a portion of patients who are resistant to IVIG therapy and who are at higher risk of developing CAAs [3]. Therefore, we here describe four cases of KD developed at young age with subsequent vascular complications and a long-term follow-up. Our intent is to draw attention to this population of patients, which may come to medical attention with disastrous angiographic pictures.
Kawasaki disease, Coronary aneurysm, Follow-up
V.L., female. In medical history: Positive family history for deep vein thrombosis (DVT) (brother, age 39 years), thrombophilia (MTHFR mutation in double heterozygosity, homozygous PAI1 mutation, anti-Cardiolipin IgG positivity, factor VIII high levels, weak ENA positivity). The girl had been hospitalized at the age of four and a half months for enteritis and right bronchopneumonia: because of the high value of the ESR, the leukocytosis and the fluctuating fever, antibiotic and steroid therapy was set up, so that the picture resolved in two weeks.
At the age of three the patient was found by her mother in bed with tachycardia, pale and in a state of general malaise; shortly after, a syncopal episode occurred for which her mother decided to take the child to the hospital: thus, she was admitted to the cardiology ward for the necessary investigations. Objectively there was only moderate pallor and tachycardia, valid and rhythmic heart tones without added noises; normal responsiveness and muscle tone, no chest pain or dyspnea. Serial ECGs performed during the hospital stay persisted in transmural necrosis vectors in leads DII, DIII, aVF, V4, V5 and V6 leads as from trans-septal necrosis or myocardiopathy as a second possibility. The rise in cardiac enzymes (CPK and lactate dehydrogenase) confirmed the diagnosis of myocardial infarction. The patient was discharged after about two weeks asymptomatic and in good circulation compensation. Throughout the follow-up period, the patient remained asymptomatic, with normal home blood pressure values.
Two control coronary angiographies were performed in 1987 and 2001: The first one showed ectasias and tortuosity extended to the whole tract of the LAD without apparent lesions that critically reduced the vascular caliber; a circumflex artery free from angiographically significant stenosis, an hypoplastic RCA. The latter showed an unchanged picture. After the second coronary angiography a therapy with beta-blocker and aspirin was set up.
Subsequent echocardiographic checks were planned (about once a year) and they revealed an apical aneurysm of the left ventricle, compatible with the subsequent evolution of myocardial infarction. The aneurysm remained stable until the last echocardiographic check in July 2021, which also showed a left ventricle of normal size with apex akinesia and a slightly reduced global left ventricular function (Figure 1 and Figure 2).
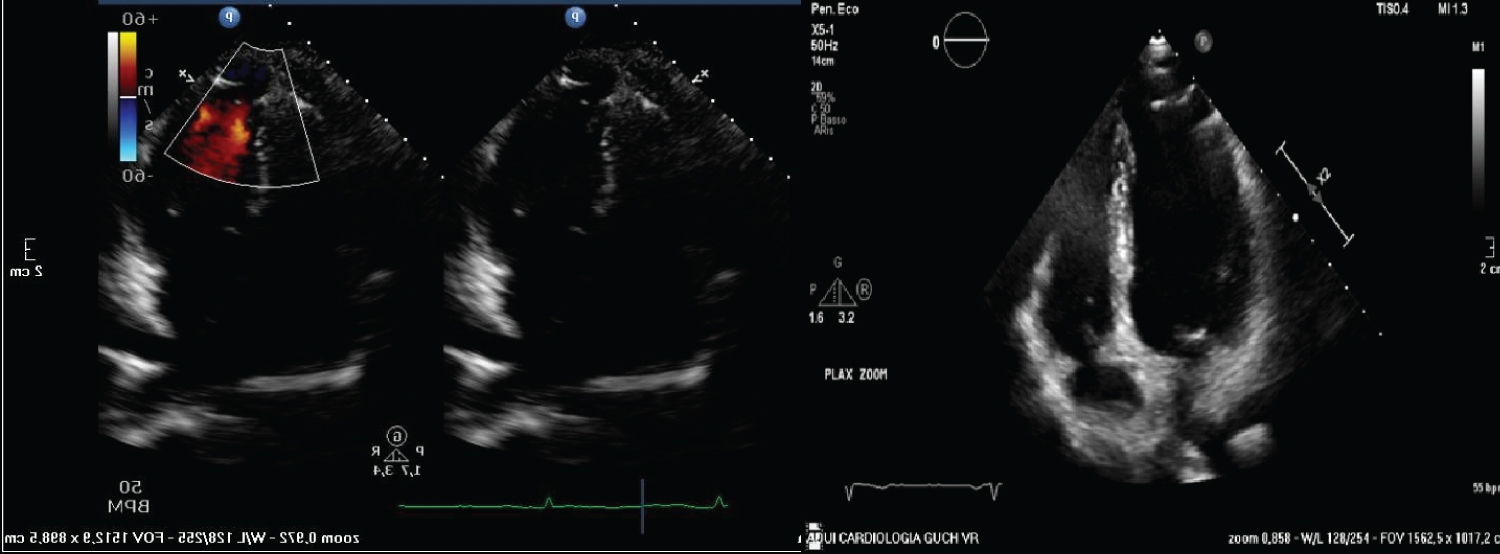 Figure 1 and 2: Echocardiographic images showing apical aneurysm of the left ventricle.
View Figure 1 and 2
Figure 1 and 2: Echocardiographic images showing apical aneurysm of the left ventricle.
View Figure 1 and 2
In December 2019 an ergometer exercise test was performed which did not detect significant changes in the ST segment suggestive for inducible ischemia at a significant heart rate. In addition to the echocardiograms, 24-Holter monitorings were scheduled (February 2017 and July 2020): They showed rare ventricular ectopic beats, often arranged in pairs.
At the last cardiological visit and echocardiographic control (August 2021) the clinical stability of the patient and the stability of the aneurysm were confirmed: It was recommended to perform a CT coronary angiogram in anticipation of the subsequent cardiological examination.
G.Z., female. Second child born at term; normal neonatal phenomena, normal weight growth and normal psychomotor development. The patient developed KD in 1990 (age 6 months): After about six hours the second dose of the oral polio vaccination cycle, hyperpyrexia appeared, for which the attending pediatrician began antibiotic therapy with amoxicillin followed by, after one day, morbilliform rash, initially limited to the trunk then spread out to the limbs. Due to the onset of the rash and the persistence of the fever despite the therapy, the girl was hospitalized after the third day from the onset of the fever. At the time of admission, in addition to the symptoms described, the girl presented hyperemia of the oropharynx and cervical adenomegaly. During the third day of hospitalization, indurative oedema of the hands and feet developed up to the ninth day. The fever persisted continuously on high values for the first ten days, then with a remitting character with bets up to 38ºC for the following 12 days. Laboratory tests performed at the entrance and during the course showed neutrophilic leukocytosis accompanied by an increase in CRP and ESR. Simultaneously with the lowering of fever, white blood cells and ESR there was also an increase in platelets, which returned to normal values around the fiftieth day of hospitalization.
The diagnosis of myocarditis, initially suspected on the basis of tachycardia disproportionate to fever (average heart rate of 200 bpm), was then confirmed by the electrocardiographic findings of negativization of the T waves in leads aVL, V2 and V3 and presence of deep Q waves in leads D2, D3 and aVF, and by chest radiographies showing the "heart significantly enlarged in all its diameters". On the 18th day, a first echocardiographic examination was performed which revealed the presence of mild to medium grade pericardial effusion and the presence of numerous aneurysms in both the common coronary trunk and the left anterior descending artery (LAD) and in the RCA. After six days, a second check: "presence of voluminous aneurysms affecting the RCA, the common trunk and the LAD, where intracoronary thrombosis is highlighted". The resolution of the pericardial effusion and intraluminal thrombosis was observed after the 32nd day from the date of admission. Starting from the 43rd day of hospitalization, the ultrasound examination showed the presence of a thickening of the wall and simultaneous reduction of the lumen of the LAD, confirming the persistence of aneurysms in the RCA. No clear anomalies of the global kinetics have ever been highlighted as well as no alterations in the valvular apparatus. The electrocardiographic findings also regressed to a complete normalization. Medical treatment initially consisted of antibiotic therapy with erythromycin in three daily doses for 9 days. From the fourth day of hospitalization (7 days after the onset of fever) aspirin 40-80 mg/kg/day was administered, lowered to 30 mg/kg/day after the first 20 days. On the tenth day (13 days after the onset of fever), IVIG therapy was started at a dose of 400 mg/kg/day for 5 consecutive days, and a second cycle was repeated after 22 days. In relation to platelets greater than one million units, anticoagulant therapy with heparin was performed for 5 days. After 59 days the girl was discharged in good general conditions, with laboratory data within the normal range. At home, therapy with aspirin and dipyridamole was continued.
A control coronary angiography was scheduled (age 22 years) (Figure 3) and detected an RCA occlusion at its origin, but showing effective hetero-coronary collateralization to the distal-middle segment; besides, the angiography showed evidence of stenosis at the proximal segment of the LAD and two aneurysms, respectively at the proximal-medium and medium segment of the artery with a satisfactory distal flow (TIMI 3).
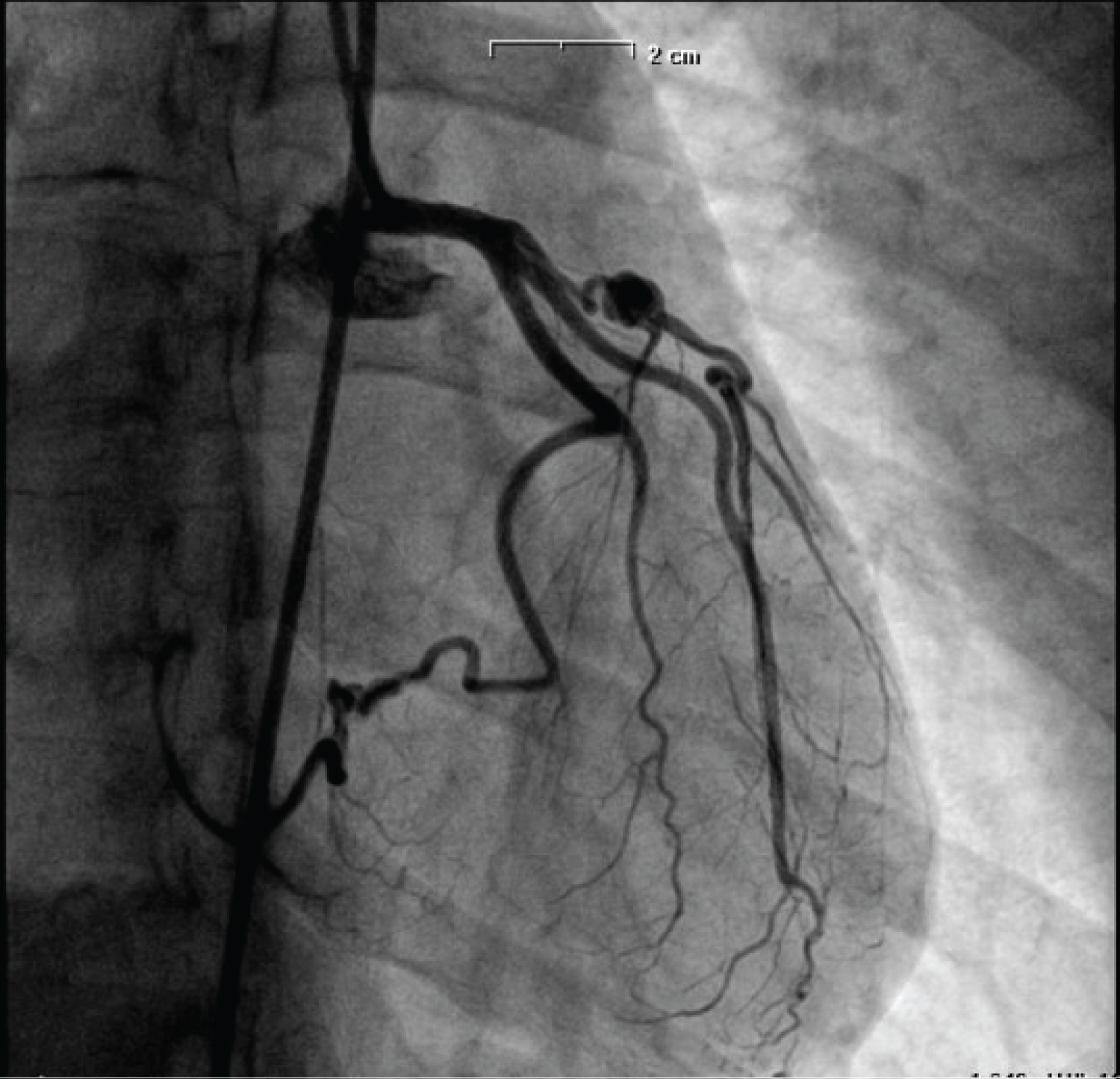 Figure 3: Coronary angiography shows: Stenosis at the proximal segment of LCA and two aneurysms.
View Figure 3
Figure 3: Coronary angiography shows: Stenosis at the proximal segment of LCA and two aneurysms.
View Figure 3
After that, the patient was hooked up to the outpatient service of the cardiovascular Operating Unit of the Major Civil Hospital of Verona and an adequate follow-up program was planned. During the timing of the follow-up the patient remained clinically asymptomatic (even while practicing sports).
Resting and stress Doppler echocardiography were performed in June 2015, showing electrocardiographic changes significant for ischemia (infero-lateral ST segment depression), but no anomalies of segmental kinetics. The ST depression remained stable on subsequent follow-up examinations (cycle ergometer test in July 2016 and in July 2018). The same finding was also highlighted in the cardiopulmonary test, done in September 2019: ST depression predominantly evident in the lateral leads (V4-V6), with slight alterations also in the inferior area which did not reach significance.
CCTA (Figure 4) was performed on March 2019, and showed the RCA occlusion at its origin still well-revascularized by the circumflex artery. The exam revealed the same two aneurysms at the proximal and medium segment of the LAD.
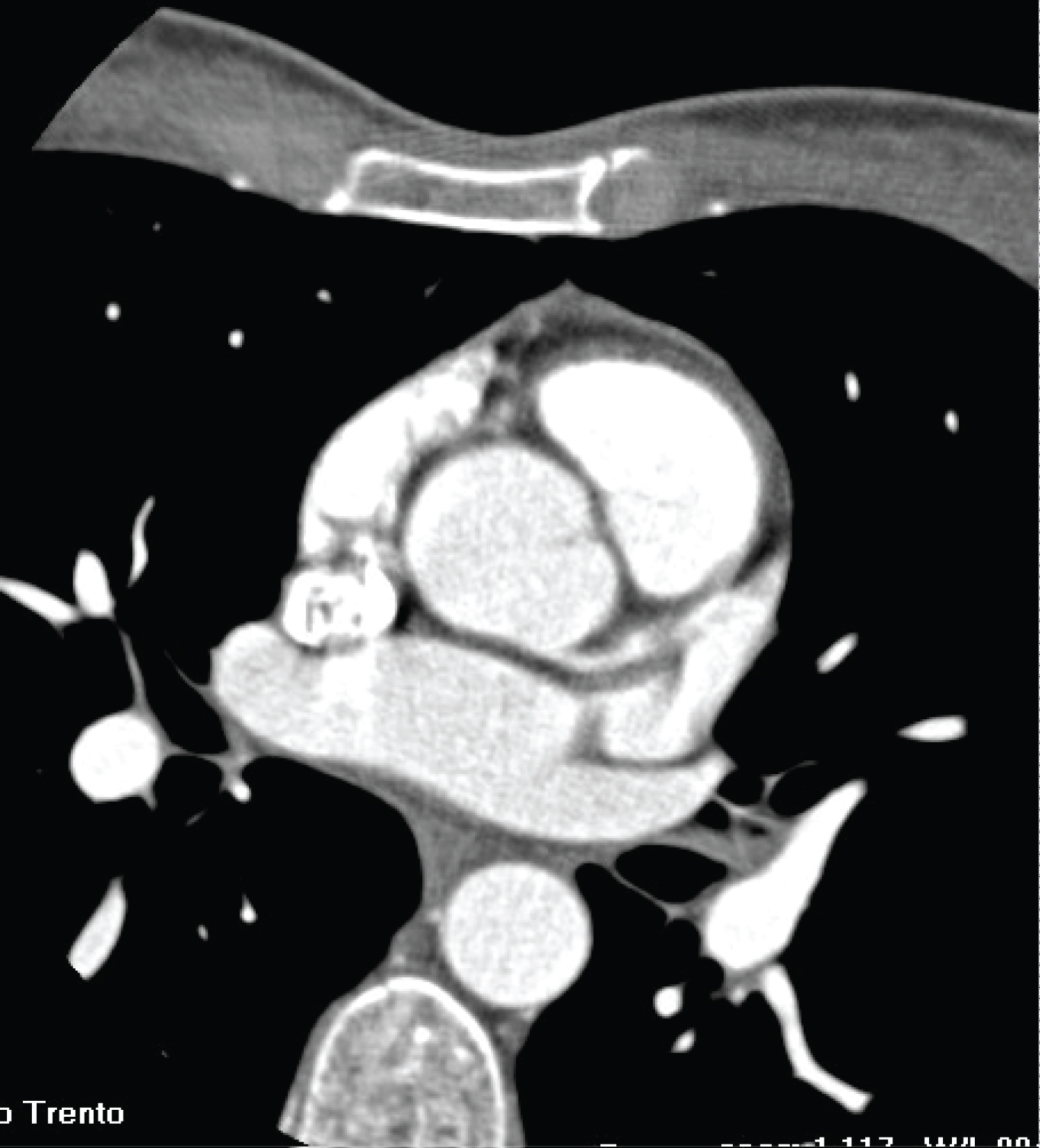 Figure 4: CCTA shows: RCA occlusion at its origin well-revascularized by the circumflex artery; stability of the two aneurysms at the proximal and medium segment of the LCA.
View Figure 4
Figure 4: CCTA shows: RCA occlusion at its origin well-revascularized by the circumflex artery; stability of the two aneurysms at the proximal and medium segment of the LCA.
View Figure 4
A 24-hours Holter monitoring was done in December 2019, showing no abnormalities in the ST segment or significant arrhythmias. A Doppler echocardiography was performed in August 2020 and resulted in normal findings, particularly a normal left ventricular size and wall motion, with a normal global systolic function.
During the entire timing of the follow-up the patient was treated with dual antiplatelet therapy (Acetylsalicylic acid 75 mg + Clopidogrel 75 mg) and beta-blocker therapy (Metoprolol 25 mg BID).
G. A., male. The patient developed KD in 1993 (age 1 year old). A Doppler echocardiography in the acute phase showed CAAs and pericardial effusion. One year later an echocardiography was repeated and it showed left coronary thrombosis without signs of acute myocardial infarction. A coronary angiography revealed coronary aneurysms involving the left coronary artery (LCA), the proximal portion of the LAD, the proximal portion of the RCA and the distal portion of the RCA. In that occasion, any surgical option was excluded (aortocoronary bypass grafting or heart transplant). Some years later, also two extracardiac aneurysms were detected, one involving the right axillary artery (11 x 8 mm) and another one involving the left axillary artery (8 x 7 mm). In 2009, when the patient was 17 years old, a CCTA was performed, showing a saccular coronary aneurysm of the distal portion of the LCA, involving the proximal portion of the LAD, of the intermediate coronary artery and of the circumflex artery (8.4 x 6.2 mm). Three other aneurysms were detected: one situated in the proximal portion of the circumflex artery, involving the origin of a marginal branch (7.1 x 6.6 mm); another calcific aneurysm situated at the origin of the LAD (maximum diameter 6.5 mm and a length of 15 mm); the last aneurysm involved the RCA right after its origin (9.7 x 9 mm). The same exam also showed a thrombotic occlusion of the LAD immediately after the proximal aneurysm, with a collateral recirculation.
In 2010 a cardiac scintigraphy showed an apical and septal hypokinesia and a reduced ejection fraction (45% at rest and 39% after stress).
In 2012 a new coronary angiography was performed confirming the aneurysms of the LCA, of the circumflex artery, of the proximal LAD, with the subsequent recirculated occlusion, and of the proximal segment of the RCA.
In 2014 a new cardiac scintigraphy was performed which showed antero-septal and apical ischemic alterations with signs of myocardial lesions more accentuated as compared to the previous examination.
In 2016 a cardiac magnetic resonance showed a slightly dilated left ventricle with a slightly reduced contractile function (Figure 5). Moreover, non-transmural late enhancement of the distal portion of the septal and anterior apex was detected.
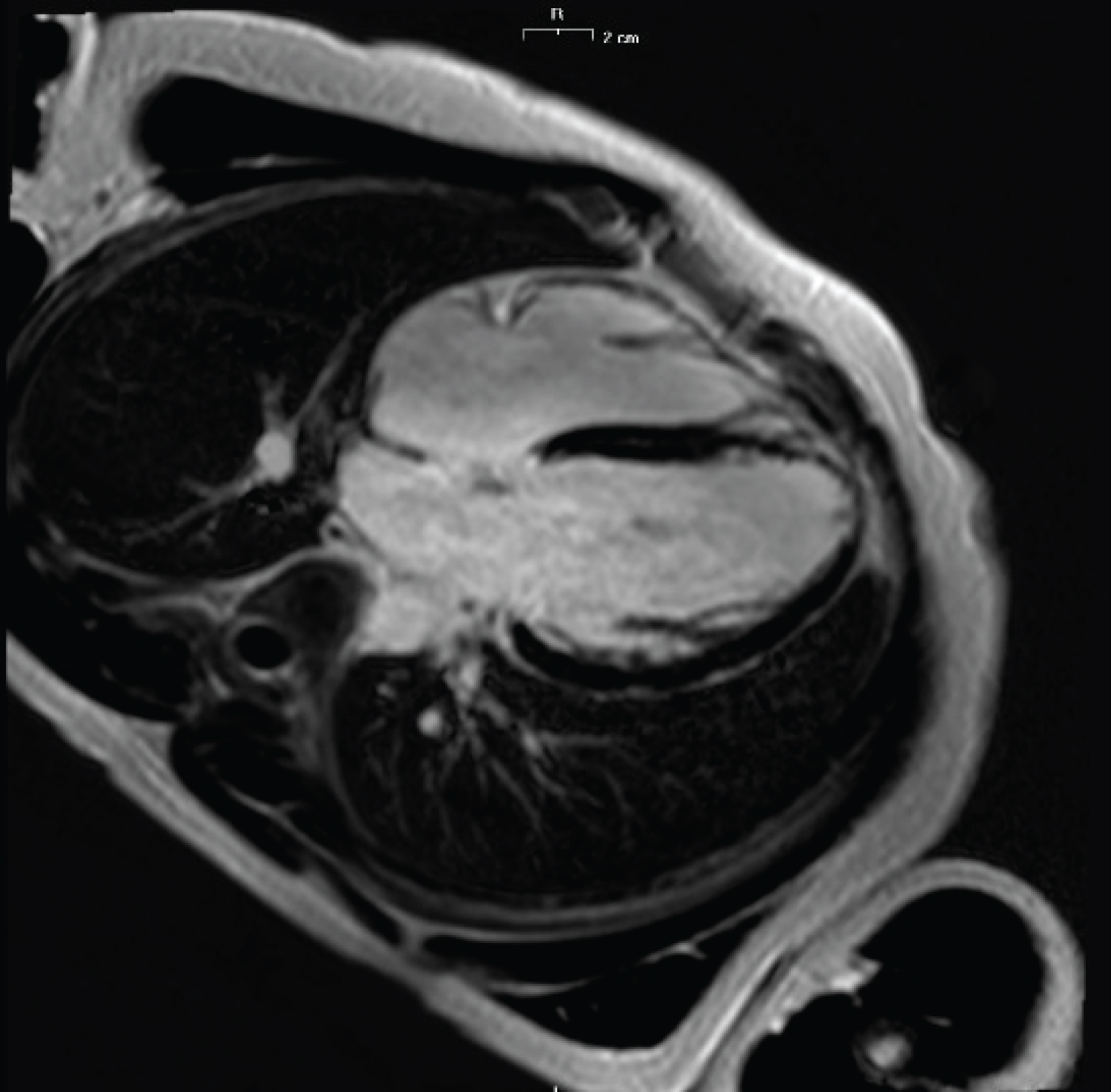 Figure 5: Cardiac magnetic resonance shows: Slightly dilated left ventricle; subendocardial late enhancement of the distal portion of the septal and anterior apex.
View Figure 5
Figure 5: Cardiac magnetic resonance shows: Slightly dilated left ventricle; subendocardial late enhancement of the distal portion of the septal and anterior apex.
View Figure 5
In 2019 a new CCTA was performed and showed aneurysms more or less unchanged as compared to the previous examination (Figure 6 and Figure 7).
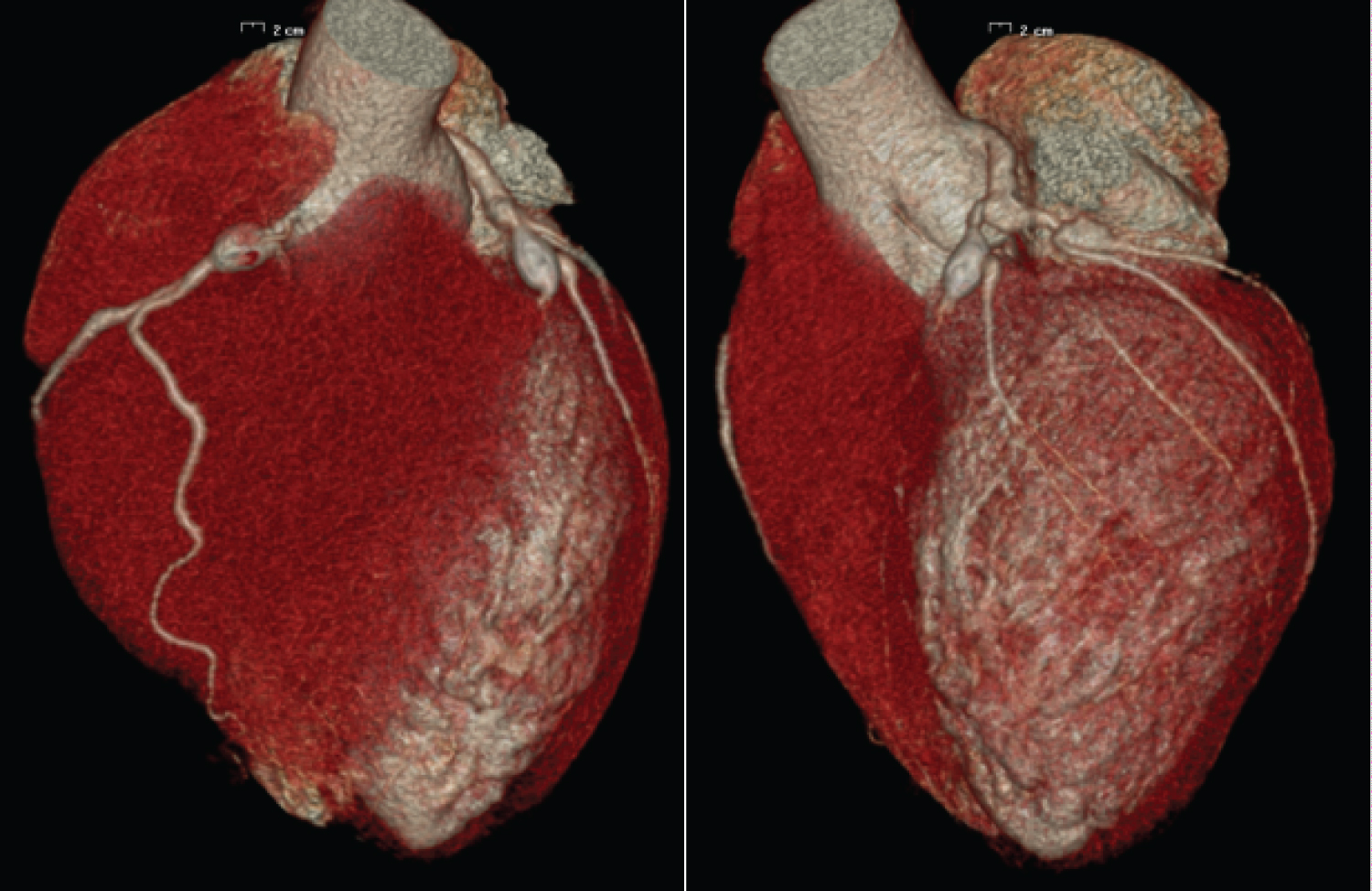 Figure 6 and 7: 3D-CCTA showing aneurysms of the right and left coronary arteries.
View Figure 6 and 7
Figure 6 and 7: 3D-CCTA showing aneurysms of the right and left coronary arteries.
View Figure 6 and 7
During the years of follow-up, also periodic cycle ergometer stress tests and 24-hour Holter monitorings were performed, without any relevant finding.
The last Doppler echocardiography was performed on 19/04/2021. The findings were comparable to the previous examination, with a dilated left ventricle with apical hypokinesia and a slightly reduced left ventricle contractility.
E.B., female. The patient developed KD in 1997 (age 8 months). It complicated with CAAs. She was treated with IVIGs and corticosteroids in the acute phase and then, in the long term, only acetylsalicylic acid at the dosage of 75 mg/die was administered. She was then followed up with periodic echocardiograms which confirmed the stability of the coronary picture. Several stress tests were performed, which were negative for inducible ischaemia.
A cardiac magnetic resonance in 2010 (14 years old) showed an aneurysm involving the RCA with a diameter of 5 mm and extending for 17 mm. No late enhancement was detected in myocardial walls. In the same year she suffered from a sincopal event after a prolonged standing. A magnetic resonance of the brain resulted in normal findings. Two EEGs were performed and the second one detected irritative anomalies in the fronto-temporal region. The patient was then evaluated by a neurologist which recommended a follow up program. No diagnosis was made and no specific drugs were introduced.
In 2015 (age 19 years old) a coronary CT (Figure 8 and Figure 9) showed persistence of the aneurysm, which was moreover increased in diameter (8 mm). Another aneurysm was also evident in the medium segment of the RCA, smaller than the previous one, measuring 4.2 mm of diameter and 16 mm of length.
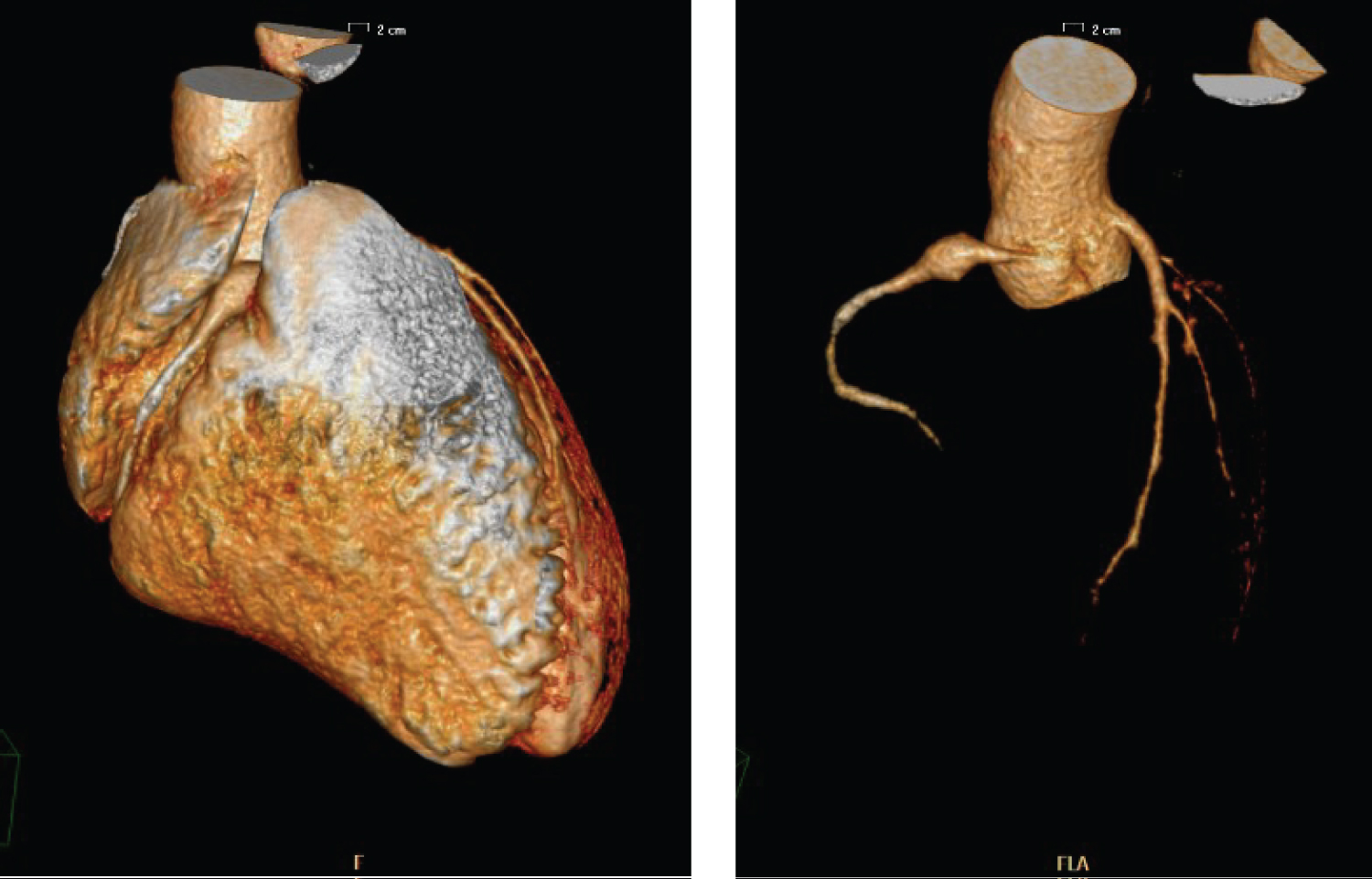 Figure 8 and 9: 3D-CCTA showing the aneurysm in the proximal portion of the RCA.
View Figure 8 and 9
Figure 8 and 9: 3D-CCTA showing the aneurysm in the proximal portion of the RCA.
View Figure 8 and 9
In 2019 an Holter ECG didn’t detect abnormal findings. In the last echocardiography (2021), the biventricular function was normal and stable as compared to the previous exams. The patient currently carries out a normal lifestyle, also performing physical activity two or three times a week with no cardiological symptoms.
KD is a relatively new disease. It was first described in Japan in 1967 by Tomisaku Kawasaki, who published a series of 50 cases in an allergy journal [4]. Shortly after, in the early ‘70s, some cases with clinical features attributable to KD were described in Hawaii [5]. From then on information about the disease spread worldwide. The diagnosis of KD today still consists in clinical criteria, as there is no confirmatory laboratory test. However, a lot of progress has been made in diagnosing KD since its first discovery. In particular, at the end of the ‘70s, echocardiography started to be used to detect coronary abnormalities [6,7] and it progressively became the pivotal imaging exam for the evaluation of children with KD. As for therapy, the first attempts consisted in antibiotics, steroids and aspirin, but they didn’t induce significant benefits on the clinical course of the disease [4]. Later on, in 1984, Furusho, et al. demonstrated the effectiveness of IVIGs as a treatment for the acute phase of the disease [8]. Subsequently, in 1988, the Committee on Infectious Diseases of the American Academy of Pediatrics endorsed IVIG treatment as the recommended therapy for children with acute KD [9]. This means that, in those years, people diagnosed with KD did not receive the optimal treatment due to the lack of evidence on therapy. As a consequence, many of them developed complications, such as coronary aneurysms or stenoses. The first and the third one of our case reports represent a sample of this. Moreover, there is to say that some patients, even when treated with IVIGs, may develop complications [2], as shown in our second and fourth case report. Not many studies have been made to estimate how big the population of patients with KD-related complications is. In 2012 Daniels LB, et al. reviewed the medical histories and coronary angiograms of 261 adults < 40 years of age who underwent coronary angiography for evaluation of suspected myocardial ischemia in 4 San Diego Hospitals. They found out that about 5% of the patients had aneurysms definitely or presumed secondary to KD. In the four patients with a clear history of KD, the aneurysms involved ≥ 2 vessels and were characterized by calcifications and high thrombotic burden. Moreover, 3 of them had also coronary stenoses. They noted that these patients had some characteristics in common: from an angiographic point of view the aneurysms involved the proximal segments of the coronary arteries, often with calcifications, followed by an angiographically normal distal segments; with regard to the clinical characteristics, they were younger, they had ≤ 1 of the traditional cardiovascular risk factors and 3 out of 4 were Asian [10].
It is important that cardiologists that deal with this type of patients are aware of the fact that treatment of KD vasculopathy may differ in several key ways from treatment of typical atherosclerosis. The high thrombotic and calcific burden make the normal angioplasty procedures unsafe. Therefore, it may be helpful to use intravascular ultrasound to avoid underestimation of the lumen size of the aneurysm [11], and rotational atherectomy to treat heavily calcified lesions [12]. Besides, KD patients with coronary complications are at higher risk of cardiovascular events than the general population [1]. For this reason, KD survivors should be followed-up at regular intervals for the treatment of cardiovascular risk factors and for a precocious identification of possible worsening of the clinical picture. All four of our cases have been followed closely with exercise tests and 24-hour Holter monitorings (about once a year). Second level exams, such as CCTA or coronary angiography, were performed with longer timescales.
In conclusion, we reported four cases of KD developed at young age, only one of which benefited in the acute phase of the disease from IVIG therapy, which is now a pivotal treatment to reduce the incidence of coronary abnormalities. Moreover, cardiac echocardiography either was not yet used in this context (case 1), or its systematic use was only at the beginning (case 2, 3 and 4). With these four case reports we have highlighted the possibility of finding a population of adult patients who may come to medical attention for acute events, such as myocardial infarction, presenting complicated and disastrous angiographic pictures: it is plausible that such a population, in addition to the traditional cardiovascular risk factors, may have developed a KD in the years of lacking diagnostic and therapeutic options.