Juvenile idiopathic arthritis (JIA), defined by the onset of arthritis evolving for more than 6 months, before the age of 16-years-old, with no evident etiology. It is the most common type of arthritis in children under the age of 16. The polyarticular form is characterized by more destructive joint and less systemic impairment. Cardiac involvement is not a usual presentation and varies from pericardial to myocardial involvement to heart failure. It is more seen in systemic form of AJI. Valvular heart disease is not common and rarely described at young age, and dominated by mitral valve prolapse with or without insufficiency.
There are only few publications about the association of aortic regurgitation and polyarticular JIA. We report a rare case of a 9-year-old child, treated in the pediatric department for polyarticular juvenile idiopathic arthritis, who presented during her follow-up with a severe aortic regurgitation (AR).
To our Knowledge, this is the third case in literature having an aortic regurgitation in seronegative polyarticular JIA and the first with a severe assessment not requiring surgery.
Juvenile idiopathic arthritis, Polyarticular form, Aortic regurgitation, Children
AR: Aortic Regurgitation; JIA: Juvenile Idiopathic Arthritis; ESR: Erythrocyte Sedimentation Rate; RF: Rheumatic Factor; ANA: Antinuclear Antibodies; ASLO: Antistreptolysin O; anti CCP: Citrullinated Protein Antibodies; TDE: Telediastolic Effect; ERO: Effective Regurgitant Orifice Area; PHT: Half Pressure Time; RV: Regurgitation Volume
Juvenile idiopathic arthritis (JIA), formerly known as juvenile rheumatoid arthritis, is the most common type of arthritis in children under the age of 16. Cardiac involvement is not a frequent outcome of the disease. It varies from pericardial impairment to myocardial and heart failure form. Valvular heart disease is not common and not frequently described in children. It is more seen in systemic forms of JIA and in seropositive patients with severe destructive forms.
We report a rare case of a 9-year-old child, treated in the pediatric department for polyarticular juvenile idiopathic arthritis, who presented during her follow-up with a severe aortic regurgitation.
It is a 9-year-old girl, followed in the pediatric department for polyarticular juvenile idiopathic arthritis in its seronegative form, diagnosis based on female sex, the involvement of more than four articulations and morning rusting. During her follow a series of biological tests were performed. The hemoglobin level was at 9 g/dl, white blood cell count of 15000/mm, a platelet count of 669000/mm3 and an erythrocyte sedimentation rate (ESR) at 74 mm/h. Immunoassay including rheumatic factor (RF), antinuclear antibodies (ANA) Antistreptolysin O (ASLO) and anti CCP; all were negative as well as phosphocalcium blot. Other renal and liver function tests were normal.
A radiological assessment made of radiography of the two hands, two knees, two ankles, thoracolumbar spine and pelvis showed arthritis of the knees and hands with bone demineralization. The abdominal ultrasound was normal and didn’t show renal medullary cyst. An ophtalmic examination showed a decrease in both visual acuity with iridocorneal synechia and at ultrasound a posterior hyaloidial bilateral detachment.
Because of the significant joint damage, the patient was initially treated by non-steroidal anti inflammatory drug (Ibuprofen), and methotrexate in addition to physiotherapy.
The patient was lost to follow up for seven years. She was admitted in the outpatient clinic because of worsening of her joint symptomatology. The clinical examination found a weight of 35 Kg, Height of 92 cm, a bilateral hallux valgus, a deformation of the two ankles, the 4th toe and 2 big toes and she nearly had lost motion of her cervical spine and had a retrognathia.
The cardiovascular examination found a blood pressure of 100/50 mmHg, a heart rate of 75 bpm, and a harsh diastolic murmur 5/6th on left border sternum. She did not report dyspnea or limitation at her daily activity. ECG showed sinus rhythm, narrow QRS, no conduction or repolarization disorder.
Transthoracic echocardiography revealed a significantly enlarged left ventricule with LVEDD at 53 mm (Z score 2,6), with preserved systolic function. Trileaflet aortic valve was thickened, with a severe aortic insufficiency (ERO = 50 mm2, Rpisa = 9 mm, PHT = 170 ms, TDE = 23 cm/s,), without stenosis. No signs of infective endocarditis were present. A competent mitral valve. No pericardial effusion was noted. The ascending aorta was morphologically normal (Figure 1 and Figure 2).
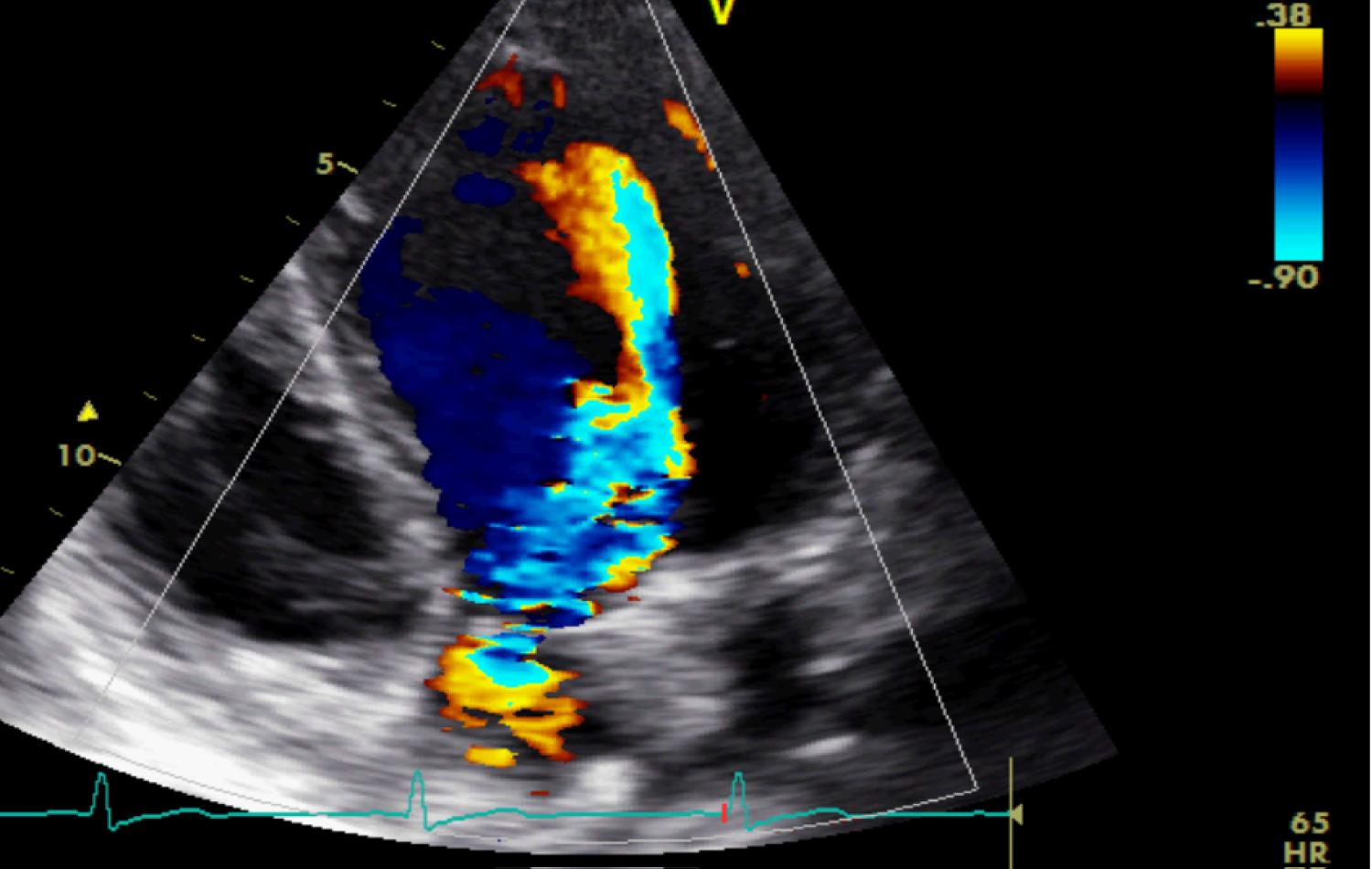 Figure 1: Apical five chambers view revealing a severe aortic regurgitation.
View Figure 1
Figure 1: Apical five chambers view revealing a severe aortic regurgitation.
View Figure 1
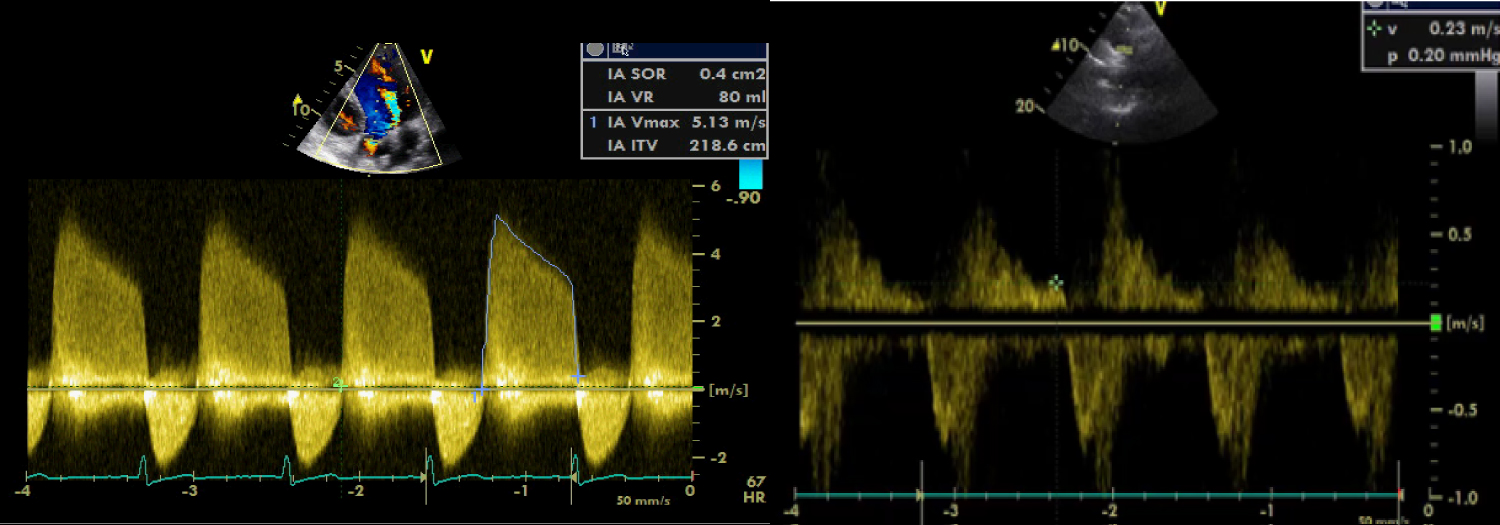 Figure 2: Continuous and pulsed Doppler revealing criteria of severity of AR (At left ERO, RV, at right TDE).
View Figure 2
Figure 2: Continuous and pulsed Doppler revealing criteria of severity of AR (At left ERO, RV, at right TDE).
View Figure 2
The patient was diagnosed to have severe aortic regurgitation complicating polyarticular AJI in its seronegative form. An other biological essay was done to exclude an acute articular rheumatism (ASLO), was negative. Thus, a treatment based on angiotensine converting enzyme inhibitor and diuretics in addition to corticosteroids and methotrexate was administrated. And because she was asymptomatic and didn’t show signs of limitation of her daily activity the decision was to follow her at outpatient clinic unit. The evolution till today is stable, the patient doent’t show any signs of heart failure, so we kept the same medication, as she doesn’t require surgery for now.
Juvenile idiopathic arthritis (JIA) is defined by the onset of arthritis evolving for more than 6 months, before the age of 16-years-old, with no evident etiology. It is the most common connective tissue disease in childhood [1]. It is divided into seven groups according to the ILAR (International league of association of rheumatology) classification [2].
The polyarticular form, defined by arthritis of more than five articulations persisting for more than six months, is not the most common form, with a prevalence of 11 to 30% in its seronegative form and 2 to 10% in its seropositive one [3-5]. Seronegative form occurs more often in girls, with 2 peaks of age, between 2 and 4 years and between 6 and 12 years, while the seropositive form occurs much later [4].
Cardiac involvement in JIA is not frequent, estimated at 4.7% in Sevenston study [6]. The most common one is the pericardial effusion, with a prevalence of 30 to 36% [7], its clinical presentation is mostly silent, or discovered accidentally during a routine ultrasound, but can also be responsible of sudden death by tamponade [8].
Myocarditis and heart failure can also be seen in the evolution of JIA but are generally not the leading clinical presentation. They contribute thought in the morbidity and mortality of the disease [9].
Valvular heart disease is rare and the average age of onset was 8 years with a sex ratio of 1.5 [9]; It is dominated by mitral valve prolapse or thickened mitral valves, associated or not with mitral regurgitation. The aortic lesions, mostly discovered in the course of an infectious endocarditis or at histological biopsy that may reveal specific granulomatous nodules or non-specific lesions [10]. Huppertz, et al. found AR in 4 children among 40 patients diagnosed with JIA [11]. Alkady and D Sircar reported a percentage of 24.3% vs. 5.4% respectively for the mitral and aortic thickening without regurgitation [12].
This AR is more often seen in the systemic and in seropositive forms of the disease, rarely in the seronegative polyarticular form [4].
However to our knowledge, there are only 2 cases reported in literature in the polyarticular form, especially in its seronegative form. The first one is a 13-year-old boy who had a mild aortic regurgitation associated with a predominant severe mitral regurgitation [4]. And the second is a nine-year-old girl diagnosed with seronegative polyarticular form, and who had moderate both aortic and mitral regurgitation treated with prednisone and did not require surgical intervention [8].
Our case is supposed to be the third one, and is different from the other ones because we had severe AR while the others had moderate AR and did not have an associated mitral regurgitation.
The revelation of AR is usually late, in general after 10 years of the onset of the disease, in patients with severe and destructive joint involvements and in serepositive forms [1,5]. However, early forms have been described as the case of J. HEYD presenting severe early aortic regurgitation only 4 months after diagnosing an JIA in its systemic form in a 13-year-old boy; and that has evolved favorably thanks to indometacine, without requiring surgery [5].
AR has generally good prognosis, regressing after medical treatment. I Bultink, et al. [10] report the case of an 18-years-old young women, who had seropositive polyarticular form of JIA complicated by severe AR requiring valve replacement with good evolution [2]. However, sometimes it can require surgery by aortic valve replacement either by bioprosthesis [1] or mechanical prosthesis [13]. As the example of a 29-years-old female patient, followed for JIA since childhood with the discovery at adult age of a severe AR with aneverysmal dilatation of ascending aorta requiring surgical intervention [9].
The prognosis depends on age of onset of AR, left ventricular dilatation, Left ventricular ejection fraction (LVEF), and aortic root dilatation that sometimes needs replacement [12].
In developing countries, the mean differential diagnosis at the early age is acute rheumatic fever especially if the initial presentation is cardiac, or when the articular damage is not progressive. It is more frequent and can lead more to valvular heart disease. However the differential diagnosis is relatively easy since the articular damage is worst testing and the testing of ASLO is negative in JIA [13].
Cardiac involvement is more frequent in children with JIA than their peers in a normal population and occurs sometimes after the onset of the disease, worsening its prognosis [9]. It is the second leading cause of death in JIA [2] .Thus , ongoing efforts for timely diagnosis of cardiovascular involvement even in the absence of clinical manifestations is critical to better provide an effective treatment and improve health related quality life [14], regardless of the severity of the disease. Whenever cardiac damage is detected, follow up should be regular to avoid severe complications that could need cardiac surgery [8,9].
The abstract has not been presented or published in any journal or conference.
None to declare.
None to declare.