Background: Incarceration of the gravid uterus (IGU) poses significant risk for maternal and fetal complications during pregnancy. Several risk factors have been implicated in the development of an incarceration of the gravid uterus; however, the association between IGU and the Ehlers-Danlos syndromes (EDS) has not been reported.
Case: A 28-year-old female at 24 weeks gestational age presented with concern for preterm labor. IGU was diagnosed and she underwent surgical reduction of the incarceration via midline laparotomy. She experienced a recurrent IGU with her second pregnancy and was ultimately diagnosed with EDS.
Conclusion: Further studies are necessary to determine if the occurrence of IGU should warrant testing for EDS or if EDS serves as an independent risk factor for IGU.
Incarceration of the gravid uterus, Pregnancy, Ehlers-danlos syndromes, Maternal complications, Fetal complications, Preterm labor
Incarceration of the gravid uterus (IGU) is a rare complication that poses significant risk for maternal and fetal complications during pregnancy. Several risk factors have been implicated in the development of IGU; however, the association between IGU and the Ehlers-Danlos Syndromes (EDS) has not been reported.
We present the first detailed case report of a late second trimester IGU in a patient ultimately diagnosed with a variant of EDS.
A 28-year-old Caucasian female, gravida 1 at 24 weeks and 2 days gestational age (GA) presented to her local obstetrician with complaint of painful uterine contractions. On initial exam, she had a severely retroverted uterus with anterior displacement of the cervix behind the pubic symphysis. She had no urinary retention or constipation. Her medical history was significant only for mild mitral valve prolapse and patella subluxation. She had no prior surgical history other than right eyelid ptosis correction. She was transported to a tertiary care center due to concern for incarceration of the gravid uterus.
Upon arrival, she was admitted to labor and delivery. Her vital signs were within normal limits. She was noted to have regular, painful uterine contractions every 3 minutes. Abdomen was gravid, soft and nontender to palpation. A pelvic exam revealed a bulging soft tissue mass palpable just inside the vaginal introitus. The cervix could not be visualized on speculum exam and was only palpable behind the pubic symphysis with suprapubic pressure. Cervix was undilated, not effaced, and without bloody show. Ultrasound demonstrated a vertex fetus with a posterior placenta. The fetal size was appropriate with an estimated fetal weight of 908g. The amniotic fluid volume was normal. A vaginal wet mount was negative. A course of betamethasone was initiated for fetal lung maturity; magnesium sulfate was ordered for fetal neuroprotection and tocolysis.
A pelvic MRI was obtained and the diagnosis of IGU was confirmed (Figure 1 and Figure 2). The cervix was 13.1 centimeters in length and the myometrium of the uterine fundus was thin. Given the frequency and intensity of uterine contractions despite tocolytic agents there was concern for uterine rupture without intervention. A neonatal consultation was obtained in case preterm delivery was warranted. On the second hospital day, the patient was taken to the operating suite for reduction of the uterine incarceration. Neuroaxial anesthesia was administered and an attempt at manual reduction was unsuccessful. An exploratory laparotomy was performed via a vertical midline incision. The uterine fundus was too deep in the pelvis to reduce abdominally, so a third assistant elevated the uterine fundus from a vaginal approach, displacing the fundus enough to allow the primary surgeon to complete the anteversion maneuver restoring normal uterine polarity. The vaginal assistant was immediately able to palpate the cervix in its normal anatomic position. The cervix remained undilated. The fetus was now in breech presentation and the placenta was along the anterior uterine wall by ultrasound assessment. After several minutes of reassuring intraoperative fetal monitoring, the abdomen was closed in the normal fashion and the patient was taken to the recovery room. Continuous fetal monitoring was performed overnight. Her postoperative course was uncomplicated and she was discharged on hospital day 8.
 Figure 1: Sagittal MRI image of a 24 week GA incarcerated gravid uterus. The fetus is in vertex presentation with the placenta implanted along the inverted anterior uterine wall. Uterine cervix is elongated to over 13 centimeters (dashed line). The fundal myometrium overlying the fetal head is extremely thin. View Figure 1
Figure 1: Sagittal MRI image of a 24 week GA incarcerated gravid uterus. The fetus is in vertex presentation with the placenta implanted along the inverted anterior uterine wall. Uterine cervix is elongated to over 13 centimeters (dashed line). The fundal myometrium overlying the fetal head is extremely thin. View Figure 1
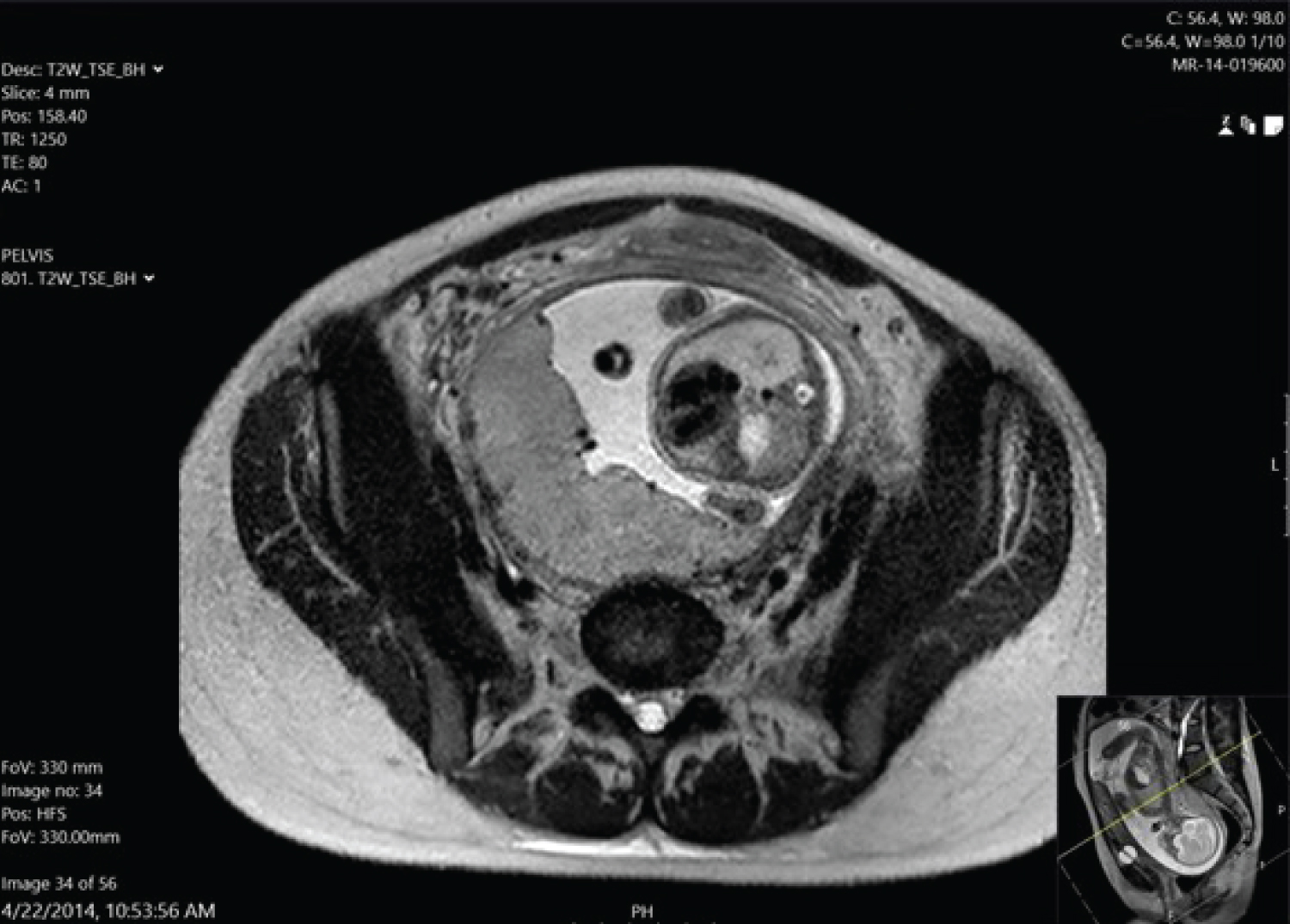 Figure 2: Mid pelvis axial MRI image of a 24 week GA incarcerated gravid uterus. Notice the cross-section of uterine cervix (circled) extending well above the pubic symphysis. View Figure 2
Figure 2: Mid pelvis axial MRI image of a 24 week GA incarcerated gravid uterus. Notice the cross-section of uterine cervix (circled) extending well above the pubic symphysis. View Figure 2
After discharge, she resumed care with her local obstetrician. Her pregnancy was uncomplicated until 33 weeks gestation. At that point she experienced preterm labor with resultant preterm, premature rupture of membranes. At 34 weeks GA, she was delivered by cesarean section secondary to breech presentation and advancing preterm labor. Her postoperative course was uncomplicated and the neonate did well.
During her second pregnancy, the patient again experienced uterine incarceration at 14 weeks GA. This was quickly identified and corrected with manual reduction in the lateral decubitus position under moderate sedation. Due to her history of preterm delivery, she was monitored with serial cervical lengths. At 21 weeks GA, there was significant cervical shortening with no measurable cervix on ultrasound (previous cervical length the week prior was 3 cm.) She was hospitalized for 2 weeks and was ultimately delivered by cesarean section at 23 weeks GA due to advancing preterm labor and breech presentation. There were no postpartum maternal complications. The neonate did well and was discharged home after a prolonged NICU stay.
The patient underwent genetic evaluation and was found to have a variant in the COL5A1 gene. This variant has been described in patients meeting clinic criteria for diagnosis of the Ehlers Danlos syndromes. She has elected to have no further pregnancies.
During the first trimester, approximately 15% of uteri are retroverted [1]. This issue typically resolves without intervention by week 14 of pregnancy as the gravid uterus transitions from a pelvic to an abdominal organ. However in an estimated 1 in 3000 pregnancies, the fundus fails to transition to a cephalad position and results in an incarceration of the gravid uterus (IGU) [2]. In these rare instances, the uterus becomes wedged between the pubic symphysis and the sacral promontory and remains entrapped while uterine contents continue to increase in size [3].
Multiple factors have been identified that can contribute to IGU including pelvic adhesions, sacral anomalies, endometriosis, uterine prolapse, ovarian tumors, leiomyomas and Mullerian anomalies [4-8]. Further, patients with a history of incarceration are reported to be at increased risk of this complication in subsequent gestations [2,9,10]. An article by Lind, et al., notes a self-reported instance of IGU in a Dutch EDS patient, but no further information is provided on this specific case [11]. Our presented case is the first to describe an Ehlers-Danlos Syndrome - or any connective tissue disorder - as a risk factor for the development of IGU.
Early recognition and treatment of IGU can reduce risk for maternal and fetal morbidity. In the first trimester, complications can include pregnancy loss, vaginal bleeding, and urinary tract infection. Second and third trimester complications include rupture of the uterus, bladder or cervix, renal failure, sepsis, and premature rupture of the membranes, hence, few of these pregnancies rarely reach term [1,12]. Moreover, pregnancies with IGU are often complicated by fetal growth restriction, likely due to compression of uterine vessels and subsequent dysfunctional uterine blood supply [4].
Early recognition is often difficult due to presentation with nonspecific symptoms including tenesmus, constipation, lower abdominal and/or back pain, urinary retention, urgency, and dysuria [4]. Asymptomatic cases of IGU have been reported at time of cesarean delivery and can result in surgical complications [3,9]. Urinary retention remains a key symptom in suspecting IGU as the retroverted gravid uterus results in urethral obstruction [12]. The vaginal examination will yield a large pelvic mass that can be felt in the pouch of Douglas, as well as failure to visualize the anteriorly displaced cervix during speculum examination [4,12]. Important differential diagnoses to consider include uterine torsion, uterine anomalies, an adnexal mass extending into the pouch of Douglas, and uterine fibroid [1].
Confirmation of the diagnosis may be made utilizing MRI [1,5,12]. Ultrasonographic examination alone may miss IGU [12]. MRI is also key to evaluate the displaced pelvic and uterine anatomy, and remains important in formulating management options [1].
First-line treatment for IGU is manual reduction prior to 20 weeks GA, with the highest rate of success when attempted before 15 weeks GA [3,13]. Manual reduction can be attempted by emptying the patient's bladder, placing the patient in the dorsal lithotomy or inverted decubitus position and then using gentle vaginal pressure to restore proper uterine polarity [3,12]. Use of ultrasound to guide the manual reduction has also proved to be a helpful aid in treatment [14,15].
Colonoscopy-assisted insufflation may be considered if manual reduction fails [1,3,4,12,16-18]. Colonoscopy-assisted reduction by insufflation of the rectosigmoid is performed with the patient in the left lateral decubitus position as the colonoscope is passed through the rectum to the sigmoid colon. Pressure from the colonoscope releases the fundus from the inferior margin of the sacral promontory [3]. As with manual reduction, success is likely before the 20th week of gestation [1,3,4].
Laparotomy may be considered when all other interventions have failed [4]. This treatment is seen as the last option for reduction, as it poses greater risk for maternal and fetal morbidity [3]. Excluding the currently presented case, our review of the available literature identified two other descriptions of reduction of IGU via laparotomy. Both cases ended well with the mothers giving birth in both cases by cesarean section in the 38th week of gestation [10,16]. In the first reported case, laparotomy was successfully completed at 22 weeks of gestation [10]. In the second case, the patient had an initial manual reduction of IGU performed at 22 weeks GA. The procedure was considered successful at the time; however, the patient represented at 25 weeks with IGU. The case report was unclear whether this was a persistence of IGU or recurrence [16]. The uterus was successfully repositioned at 25 weeks GA by median laparotomy [16].
Other documented treatments to correct uterine polarity include a case of a patient with a large subserous fibroid who presented at 20 weeks with IGU. After an abdominal myomectomy was performed, the patient's gravid uterus returned to its correct anatomic position [19]. Another rare case occurred in which there was spontaneous reduction of the uterus after general analgesia was administered [17].
Some patients with IGU may remain asymptomatic throughout their pregnancy [4,6,9,12,20-22]. Asymptomatic cases that present after 20 weeks gestation or in which attempts at reduction fail could be considered for expectant management with serial ultrasounds to monitor fetal growth and amniotic fluid volume [3,22]. It is imperative that a clinician has preoperative recognition of IGU as a vaginal delivery is impracticable and can result in severe maternal morbidity and even fetal death [9]. For those cases in which the incarcerated uterus is irreducible prior to delivery, extra caution is recommended to execute a cesarean section by median laparotomy at term [1,3,4,9].
The Ehlers-Danlos syndromes (EDS) are a genetically linked group of disorders that affect connective tissues. Patients with EDS show abnormal collagen synthesis, which effects ligaments, skin, blood vessels, organs and joints [23]. Though prevalent in up to 2% of the population, they remain largely undiagnosed [24].
Approximately 29 genes, located on chromosomes 15 and 24, play a role in collagen protein structure. Disruption of any of these genes results in development of EDS. As of 2017, there are 13 recognized subtypes of EDS distinguished by genetic mutation, though the symptoms of the diseases frequently overlap [25,26]. Shared symptoms of EDS subtypes include joint hypermobility, hyperextensibility and fragile skin. Many EDS variants also include characteristics such as extreme fatigue, irritable bowel, pain, sleep disturbance, and other cardiovascular, gastrointestinal, orthopedic, neurological, oromandibular, psychological, and allergic/immunological manifestations [27].
Patients with EDS are at risk for multiple pregnancy complications, including higher rates of infertility, premature rupture of membranes, precipitous labor, postpartum hemorrhage, atonic uterus, bleeding, vaginal and/or perineal tears during birth, wound dehiscence and varicose veins [24,27,28].
Furthermore, prior cases have described the increased risk for fetal malpresentation secondary to uterine muscle laxity. A survey by Lind reported 66 women with EDS who carried a total of 194 fetuses beyond 24 weeks gestation. Of those pregnancies, 15 cases of abnormal presentation were reported. One patient self-reported an instance of IGU, but no further description was given of that occurrence [11].
The predominant growth mechanism of the gravid uterus is by way of stretch-induced myometrial hypertrophy, in which collagen plays a role by providing connective tissues with rigidity [29]. Some authors have suggested that one of the mechanisms by which obstetric dysfunction occurs in EDS patients is the maintenance of excessive distention of the uterine myometrium, complicating the normal uterine growth progressions of pregnancy [23].
Early diagnosis of IGU is critical to prevent complications involving both mother and fetus. Recognition of mild, nonspecific symptoms in the presence of known risk factors for IGU enables obstetricians to intervene during early gestation. The presented case highlights the potential increased risk for IGU in patients with EDS. Further studies are needed to determine if the occurrence of IGU should warrant testing for EDS or if EDS serves as an independent risk factor for IGU.
No financial support or funding for this project.
All authors report no conflict of interest.