Benign leiomyoma can undergo degeneration that result in unusual clinical and radiological presentations. Diffuse hydropic fibroid degeneration resulting in myometrial cyst formation is very rare. Here we describe intra-operative ultrasound recognition of this phenomenon.
A 35-year-old nulliparous woman presented to the Gynaecology Oncology Clinic with menorrhagia and pressure symptoms. Abdominal examination revealed an abdominal mass extending to the umbilicus. Ultrasound showed complex pelvic mass with thick septations and solid components. CA125 and germ cell markers were normal. Transverse suprapubic laparotomy revealed a hugely expanded uterus with normal ovaries and fallopian tubes. Intra-operative ultrasound showed a multi-cystic lesion within the myometrium. Using our suggested surgical technique for myometrial cystectomy, the lesion was enucleated, the pseudocapsule was resected and the myometrium was reconstituted. Histopathology showed benign leiomyoma with extensive hydropic degeneration.
Myometrial cysts due to hydropic uterine leiomyomata are extremely uncommon and can mimic neoplastic adnexal disease on ultrasonography.
Uterine fibroid, Surgical technique, Intra-operative ultrasound, Gynaecological surgery, Hydropic fibroid degeneration
MRI: Magnetic resonance imaging; GP: General practioner; GOPD: Gynaecology outpatient department
Uterine leiomyomata are the most common type of gynaecological neoplastic disease with prevalence of 20-30% in women of reproductive age [1]. Composed of monoclonal expansion of smooth muscle cells, they typically occur in the uterus but can also occur at extra-uterine locations and more rarely can have vascular involvement (intravenous leiomyomatosis) [2]. Symptoms range from none with incidental diagnosis to irregular bleeding, to pain or pressure symptoms with large or degenerating fibroids [1]. Uterine leiomyoma can undergo degenerative changes including hydropic degeneration [3], resulting in a range of appearances on ultrasonography and Magnetic Resonance Imaging (MRI). In rare instances, extensive hydropic degeneration can cause appearances of a complex cystic structure. While most fibroids have characteristic appearance on ultrasound, diagnosis can be challenging with patterns of degeneration such as hydropic cystic degeneration resulting in their misinterpretation for more sinister pathologies [4]. This case report describes cystic degeneration of uterine fibroid mimicking a multiloculated adnexal cyst in a premenopausal woman.
A 35-year-old nulliparous woman referred to Gynaecological Oncology Outpatient Department (GOPD) by her General Practitioner (GP) with history of abnormal uterine bleeding and a complex pelvic mass on imaging. The patient reported a seven-month history of new prolonged heavy menstrual bleeding associated with clots and flooding. She also complained of new onset of urinary frequency, constipation and deep dyspareunia. There was no history of sub-fertility or past medical or surgical history. Cervical smear history was up to date. She was an active smoker of 15 cigarettes per day with a 20-pack year history. Family history was significant for a maternal aunt with gynaecological malignancy in her twenties, the details and histological subtype of which were unknown to the patient but increased the risk stratification for this patient. A trial of the oral combined contraceptive pill had been commenced by the GP but with no change in symptoms. An ultrasound at a private radiological facility described a large complex right adnexal mass 12.5 × 10.1 × 13.4 cm, which prompted an urgent referral to the gynaecological oncology service at a tertiary centre.
On assessment in outpatient clinic, her examination revealed a large non-tender lower abdominal mass extending to the level of a sixteen-week uterus. Transvaginal ultrasound showed a pelvic mass that appeared complex with thick septa with solid components adjacent to the capsule (Figure 1 and Figure 2). It was difficult to discern the origin of the mass. A normal left ovary was seen. Serum tumour markers (Cancer antigen-125, lactate dehydrogenase, human chorionic gonadotrophin and alpha-fetoprotein) were normal. As the patient was patient was symptomatic and the ultrasound appearance convincing for a complex adnexal pathology, surgical intervention was offered.
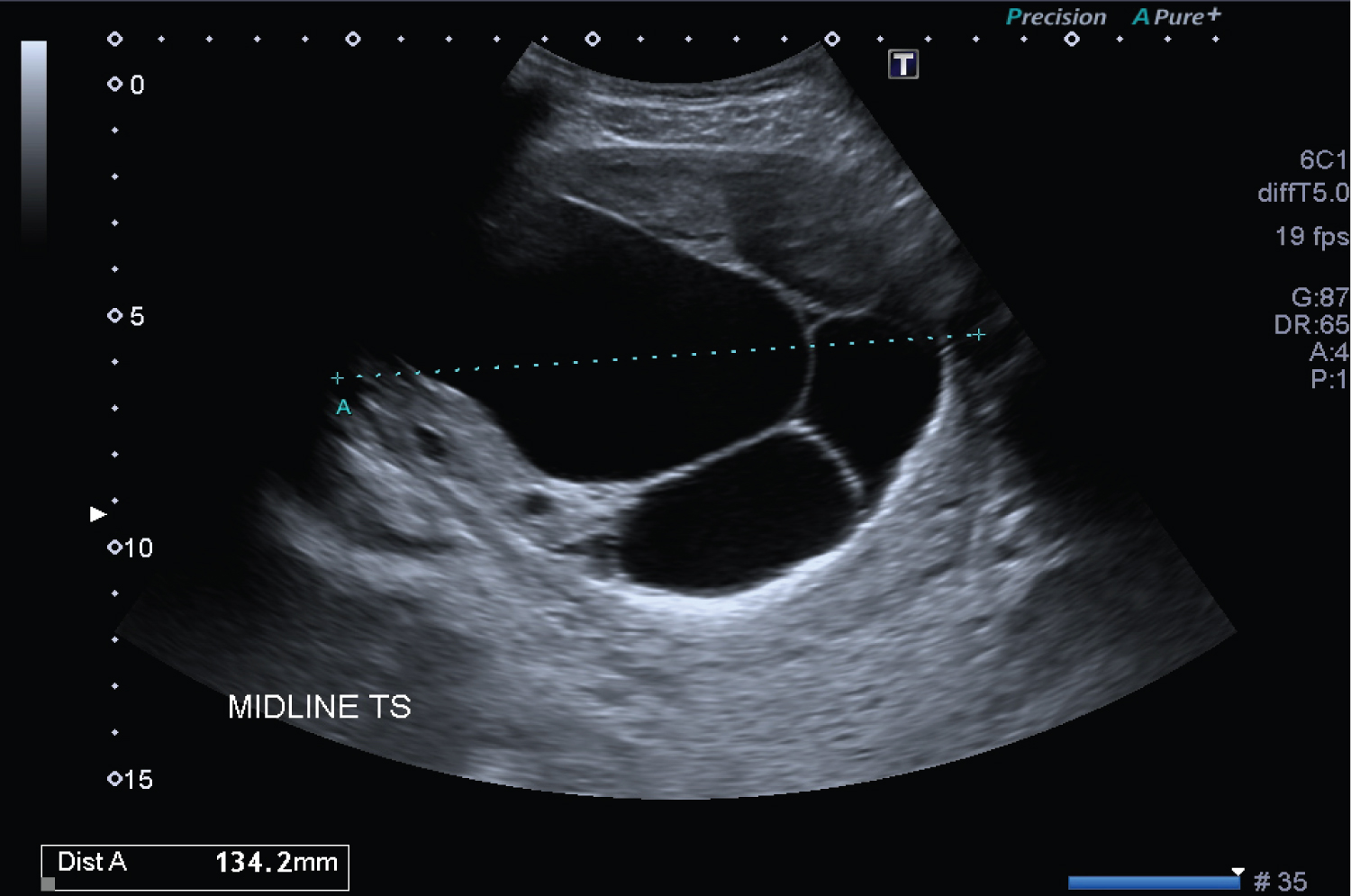 Figure 1: Pre-operative ultrasound of the large complex pelvic mass, displaying solid and cystic components, suspected to be a complex adnexal pathology in this pre-menopausal patient. View Figure 1
Figure 1: Pre-operative ultrasound of the large complex pelvic mass, displaying solid and cystic components, suspected to be a complex adnexal pathology in this pre-menopausal patient. View Figure 1
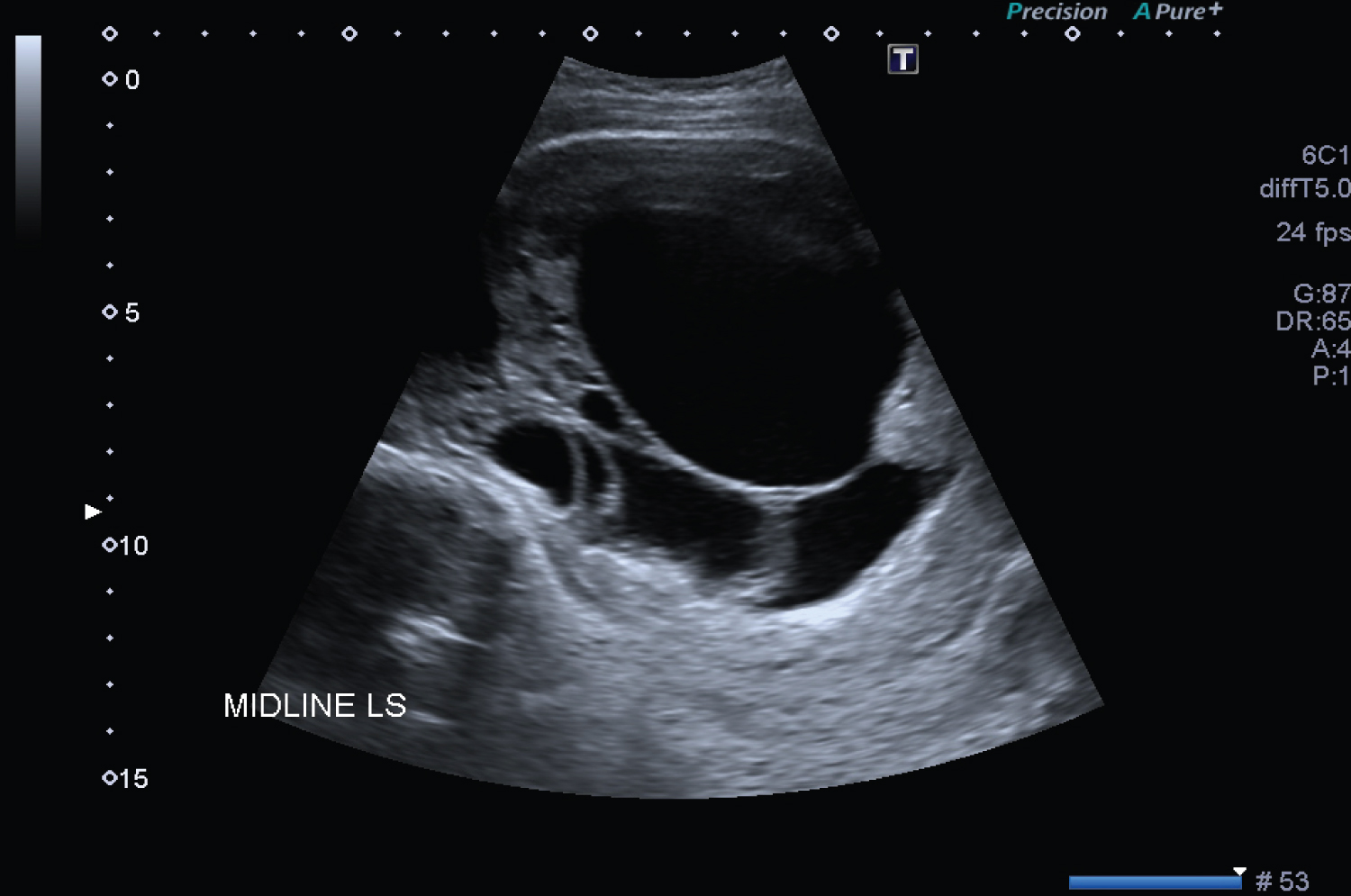 Figure 2: Pre-operative ultrasonography of the complex pelvic pathology showing large fluid filled multiloculated cystic areas. View Figure 2
Figure 2: Pre-operative ultrasonography of the complex pelvic pathology showing large fluid filled multiloculated cystic areas. View Figure 2
Hysteroscopy and exploratory laparotomy were performed. Preliminary hysteroscopy revealed an elongated cavity which was indented anteriorly near the fundus but was otherwise unremarkable. Endometrial curetting was benign on histopathological examination. After careful examination of the pelvic organs through an extended transverse suprapubic incision, normal ovaries and fallopian tubes were noted bilaterally (Figure 3), with the right adnexa located posterior to the uterus which may have resulted in difficulty visualising it on pre-operative ultrasonography. The uterus was enlarged (Figure 3), and an intra-operative trans-myometrial ultrasound showed a multi-cystic structure within the myometrium itself (Figure 4).
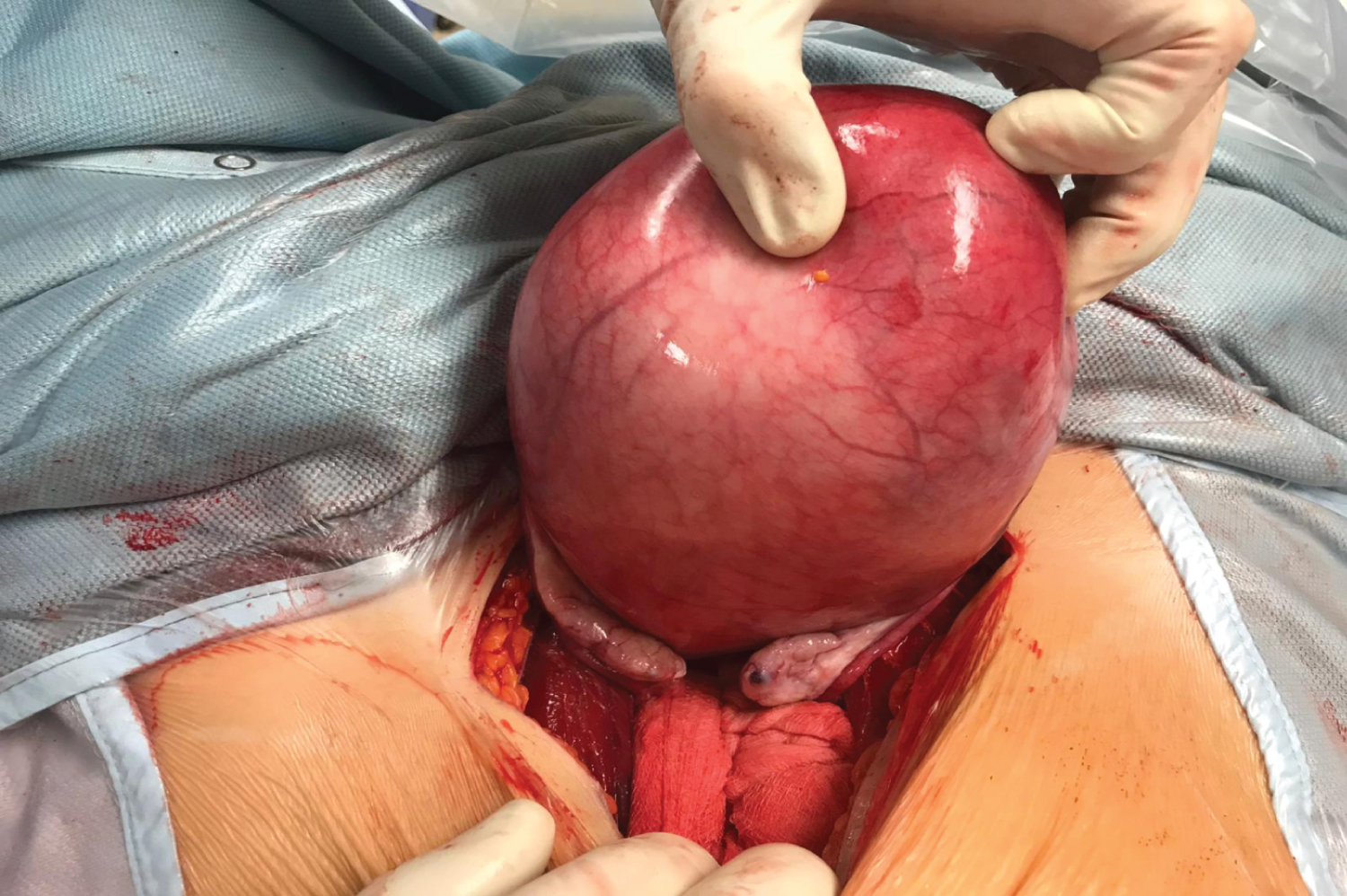 Figure 3: Intra-operative findings on transverse suprapubic laparotomy - normal fallopian tubes and ovaries and a markedly enlarged uterus. View Figure 3
Figure 3: Intra-operative findings on transverse suprapubic laparotomy - normal fallopian tubes and ovaries and a markedly enlarged uterus. View Figure 3
 Figure 4: Intra-operative ultrasound confirming a multilocular myometrial cyst with solid components. View Figure 4
Figure 4: Intra-operative ultrasound confirming a multilocular myometrial cyst with solid components. View Figure 4
A myometrial cystectomy was performed through an elliptical incision in the anterior uterine wall inferior to the round ligaments, opening the upper uterus as a lid to reveal the capsule of a cystic lesion. The lesion was dissected free from the compressed surrounding false capsule of myometrium. The incision did not extend to the endometrial cavity. The uterus was then reconstituted with deep interrupted sutures and Herring Bone Wong [5] suturing of the superficial myoserosal layer with a 00 Monocryl (poliglecaprone 25) monofilament suture.
The patient's post-operatively recovery was uncomplicated, and she was discharged home on day four post-operative in good condition. She was well at her two-week follow-up visit. The histopathological findings confirmed a large hydropic leiomyoma with extensive cystic degeneration, without evidence of malignancy or atypia.
Myometrial cysts are extremely uncommon and pose a diagnostic challenge for both gynaecologists and radiologist alike. In this case, pre-operative ultrasound findings suggested a complex cystic adnexal lesion, a much more common diagnosis. Hydropic degeneration of leiomyoma is rare, especially in the nongravid uterus, with only three previous reported cases [6-8]. It is reported to be more common in pregnancy [9] when rapid growth can occur.
The first-line imaging modality for pelvic lesions is ultrasonography. Appearances of atypical degenerating leiomyomas are variable on ultrasonic imaging and are better characterized using MRI [8]. On MRI, they can appear as complex lobulated masses with mainly high T2 signal and internal strands of low T2 signal. With more simple architecture, cystic leiomyomas can appear as unilocular or multilocular pelvic masses [4]. These appearances lead to misinterpretation as the much more likely adnexal cyst and raise concern for malignancy. The misinterpretation of hydropic leiomyomata on ultrasonography has been reported in both the premenopausal setting [4,8-10] and post-menopausal setting [11]. Diagnosis of uterine leiomyomata can be made even more challenging when they not only have an atypical degenerative pattern, but when this is combined with an atypical extra-uterine location [4,12].
While cystic fibroid degeneration has been previously reported, this case is the first to describe intra-operative ultrasound assessment to plan surgical technique. Intraoperative ultrasound in gynaecological surgery improves complete resection and minimizes damage to surrounding reproductive structures [13,14]. Where unanticipated pathologies are identified during exploration of the pelvis, we advocate use of intra-operative ultrasonography to ascertain the underlying architecture of the uterine pathology to proceed with tailored resection. We also describe proposed surgical technique for fertility-sparing myometrial cystectomy, the first description of this procedure in the setting of hydropic leiomyoma.
This case highlights the complexity of the ultrasound appearance of a degenerating uterine fibroid. Optimally MRI would have been performed before surgery as it is likely to have better identified the separate normal adnexa. In the event of the unusual finding at surgery intraoperative ultrasound delineated the lesion satisfactorily and facilitated optimisation of uterine body incision to access and enucleates it. The gynaecologist should be aware that hydropic degeneration of fibroid occurs outside of pregnancy and include it in the differential diagnosis of complex cystic pelvic lesions.
None to declare.
None to declare.
None to disclose.
None to disclose.
All listed authors played active roles in the reporting of this case. GAC drafted the manuscript. The manuscript was critically appraised by CT, ZM and NG.