Adenomyosis refers to the occurrence of ectopic endometrial glands and the surrounding stroma within the myometrium. A distinction is made between diffuse and focal forms (rare nodular forms and an adenomyoma). Ectopic pregnancy (EUG) occurs in about 1.5 to 2.0% of pregnancies and can be a life-threatening event. 2% of all EUG are cornual/intramural ectopic pregnancy. We present the case of a 33-year-old women (GII/PI) who complained about vaginal bleeding in the 6th week of pregnancy. The next presentation took place in 7 + 3 gestational weeks due to contraction-like pain in the lower abdomen and constant pain in the right lower abdomen. Sonographically we discovered the intrauterine amniotic cavity with an abnormal embryonic development, an intracavitary hematoma and a "thickening" in the right tube angle. After 4 days (8 + 0 weeks of gestation), the patient complained again with constant pain in the right lower abdomen comparable to dysmenorrhea. Sonographically, an empty amniotic cavity and a cystic mass in the right-angle of fallopian tube continued to be present. HCG was 6774 mIU/ml. With the high suspicion of a cornual ectopic pregnancy, a laparoscopy and a curettage were indexed. Intraoperatively, a protrusion in the right-angle of fallopian tube was present. The finding was cut with a monopolar needle and a chocolate-like secretion emptied. Here, endometrial tissue became apparent. A wedge resection was carried out with the removal of the entire ectopic endometrial tissue. After the histological processing of the preparation, endometriosis with a moderate proliferative activity emerged: Ki 67 of 10%. In the abrasion material a gestational sac, as well as parts of pregnancy-typical endometrium were detected. In case of a sonographically seen gestational sac located at the angle of a fallopian tube, one should think of a cornual/interstitial localization of a EUG. However, even in nodular adenomyosis a cystic finding may form as it was proven in our case. Therefore, in order to formulate a precise and reliable diagnosis a laparoscopy with tissue removal for histological may be necessary.
Nodular adenomyosis, Cornual pregnancy, Ectopic pregnancy, Endometriosis
Adenomyosis refers to the occurrence of the endometrial glands and surrounding stroma within the uterine myometrium. A distinction is made between diffuse and focal forms: rare nodular forms and adenomyoma [1,2]. Adenomyoma is a tumor-like lesion of adenomyosis uteri with structurally complex endometrial glands in a hyperplastic stroma consisting of smooth muscles or leiomyo fibromatous tissue [2,3]. About 1% of the affected patients are under 40 years of age, in these cases the reproductive phase of the woman is affected [4].
Ectopic pregnancy (EUG) occurs in about 1.5 to 2.0% of pregnancies and can be a life-threatening event. Such pregnancies cause 6% of all maternal deaths in gynecology [5]. 2% of all EUG are cornual/intramural pregnancies [6]. Ascornual/intramural gravity is a pregnancy implanted in the myometrium and not surrounded by decidua. Risk factors are previous adnexitis and internal genital surgery, in particular homolateral salpingectomy, and adenomyosis uteri. Cornual/intramural pregnancies are very rare [7,8].
A 33-year-old GII/PI patient presented herself with vaginal bleeding in the 6th week of pregnancy in our emergency department. Sonographically, one could detect an intrauterine amniotic cavity corresponding to the week of pregnancy. Thus, physical rest and a follow-up were initially recommended (Figure 1).
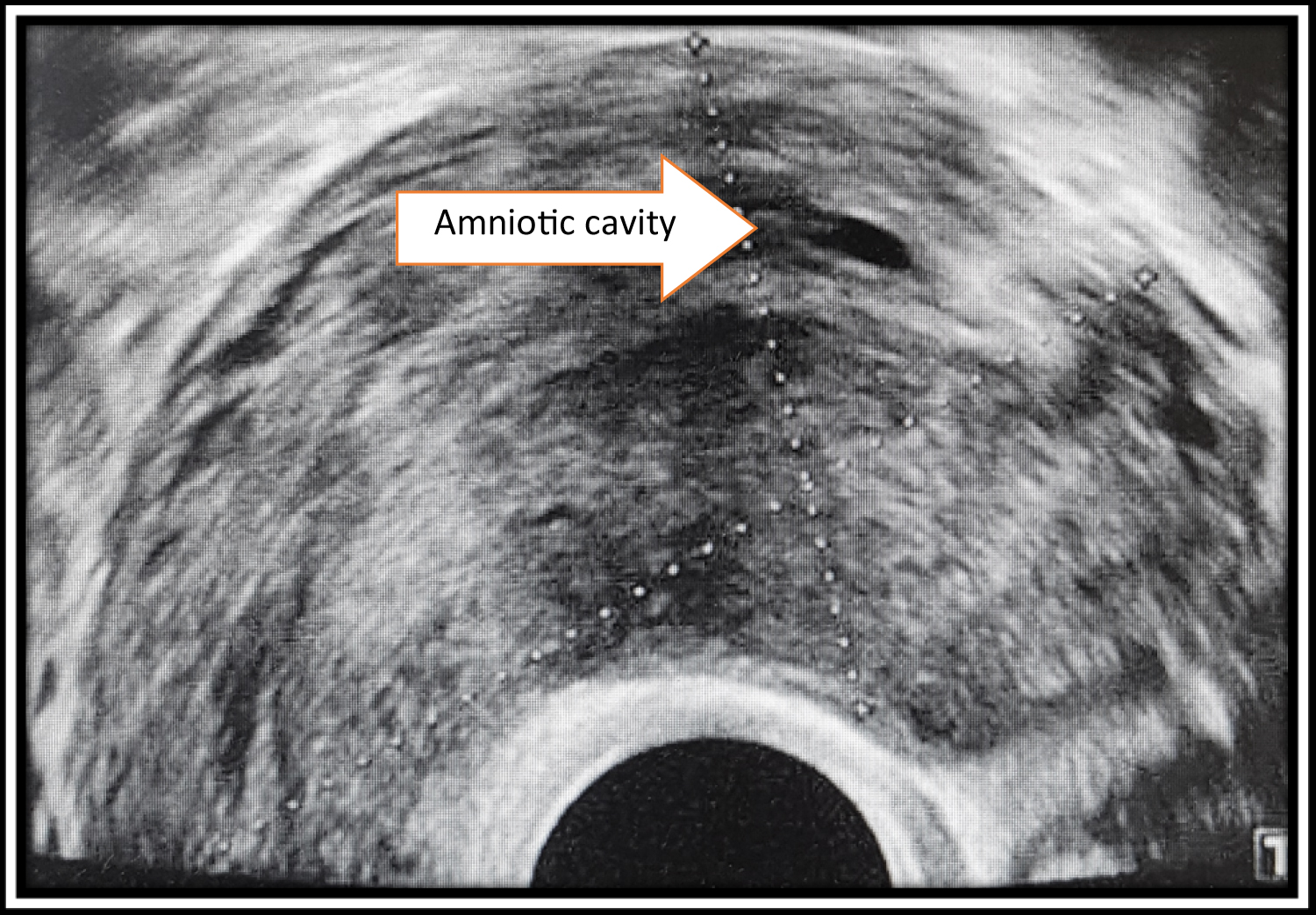 Figure 1: Uterus in sagittal section (6 gestation weeks).
View Figure 1
Figure 1: Uterus in sagittal section (6 gestation weeks).
View Figure 1
At the time of 7 + 3 gestational weeks the patient presented herself again with the main complaints of contraction-like pain in the lower abdomen, constant pain in the right lower abdomen and persistent vaginal bleeding. Sonographically, an amniotic sac without an embryo and an intracavitary hematoma were found, which gave rise to the suspicion of an abortus incipiens. This ultrasound showed a "thickening" in the right uterus horn/angle of fallopian tube. The patient reported that she had been suffering from pain of similar nature, described as severe dysmenorrhea in the right lower abdomen already before pregnancy (Figure 2 and Figure 3).
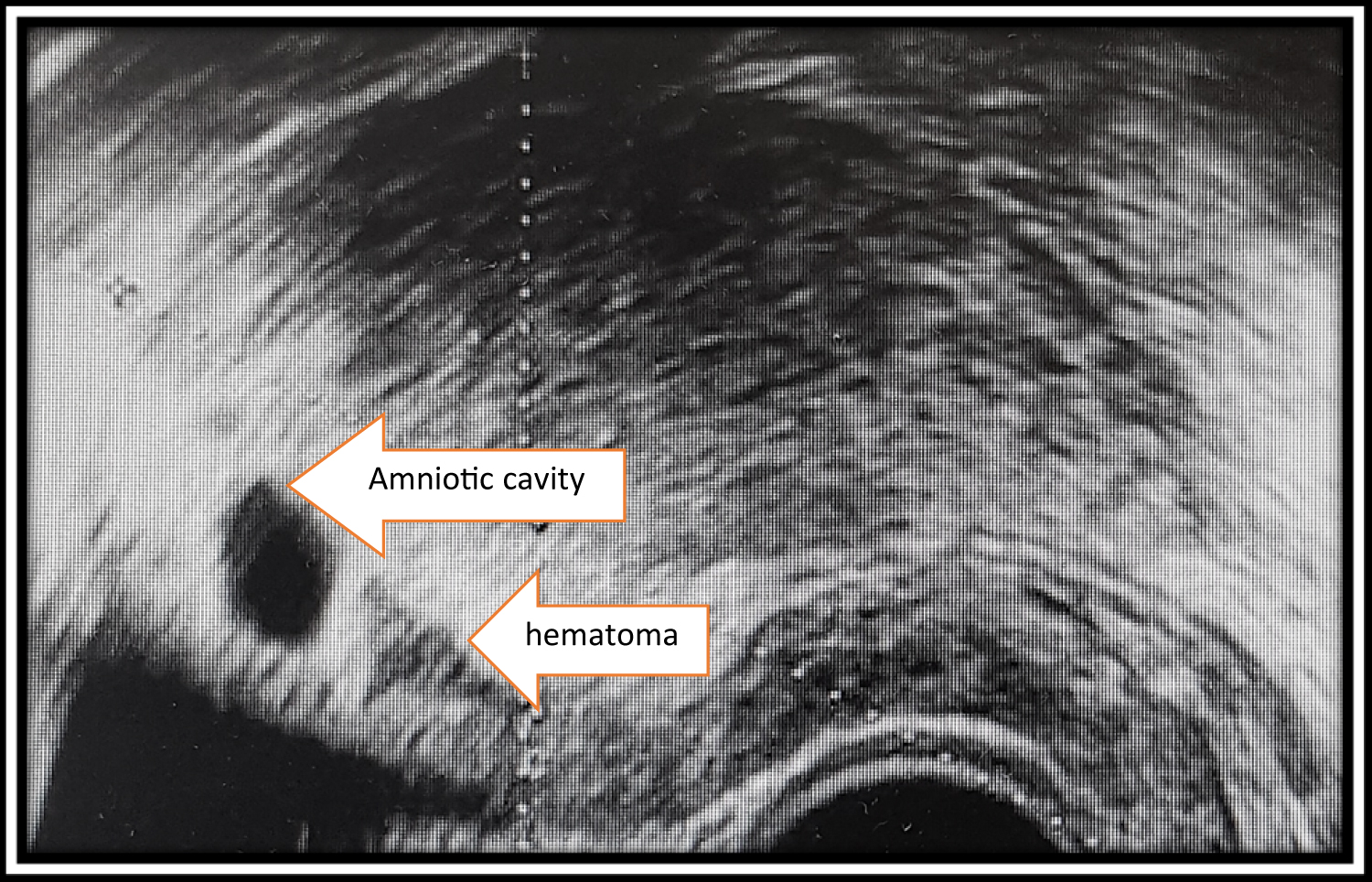 Figure 2: Uterus in the sagittal section (7 + 3 gestation weeks).
View Figure 2
Figure 2: Uterus in the sagittal section (7 + 3 gestation weeks).
View Figure 2
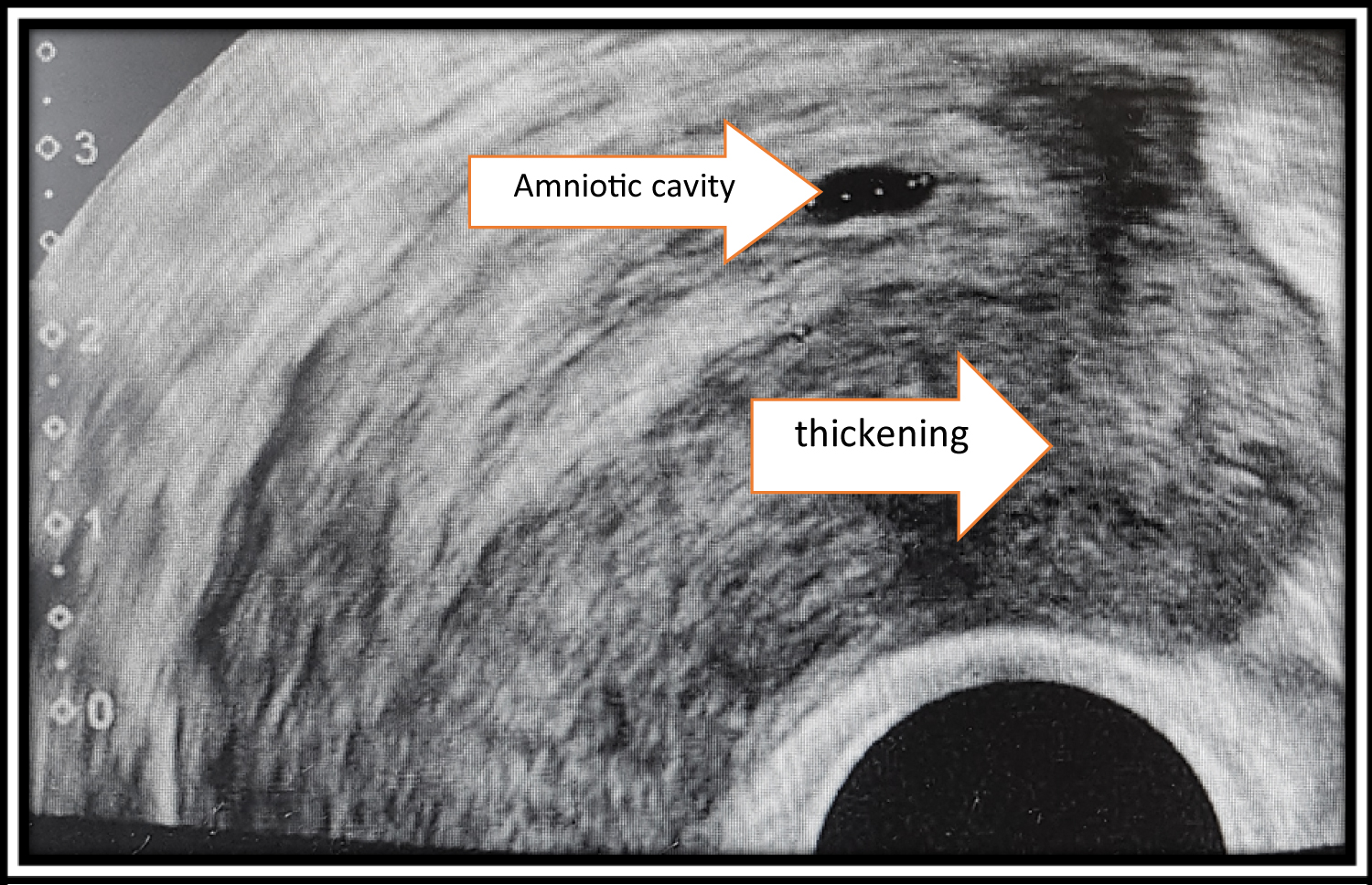 Figure 3: Uterus in cross section (7 + 3 SSW).
View Figure 3
Figure 3: Uterus in cross section (7 + 3 SSW).
View Figure 3
The patient did not want any further therapy at this time.
4 days later, the patient still suffered from constant pain in the right lower abdomen, as in dysmenorrhea. A vaginal examination in the right lower abdomen was very painful for the patient. The β-HCG value at that time was 6774 mIU/ml. Sonographically, an empty amniotic cavity and a cystic mass at the angle of the right fallopian tube continued to be present. There was an urgent suspicion of a cornual pregnancy, so that laparoscopy and simultaneous curettage were indexed (Figure 4 and Figure 5).
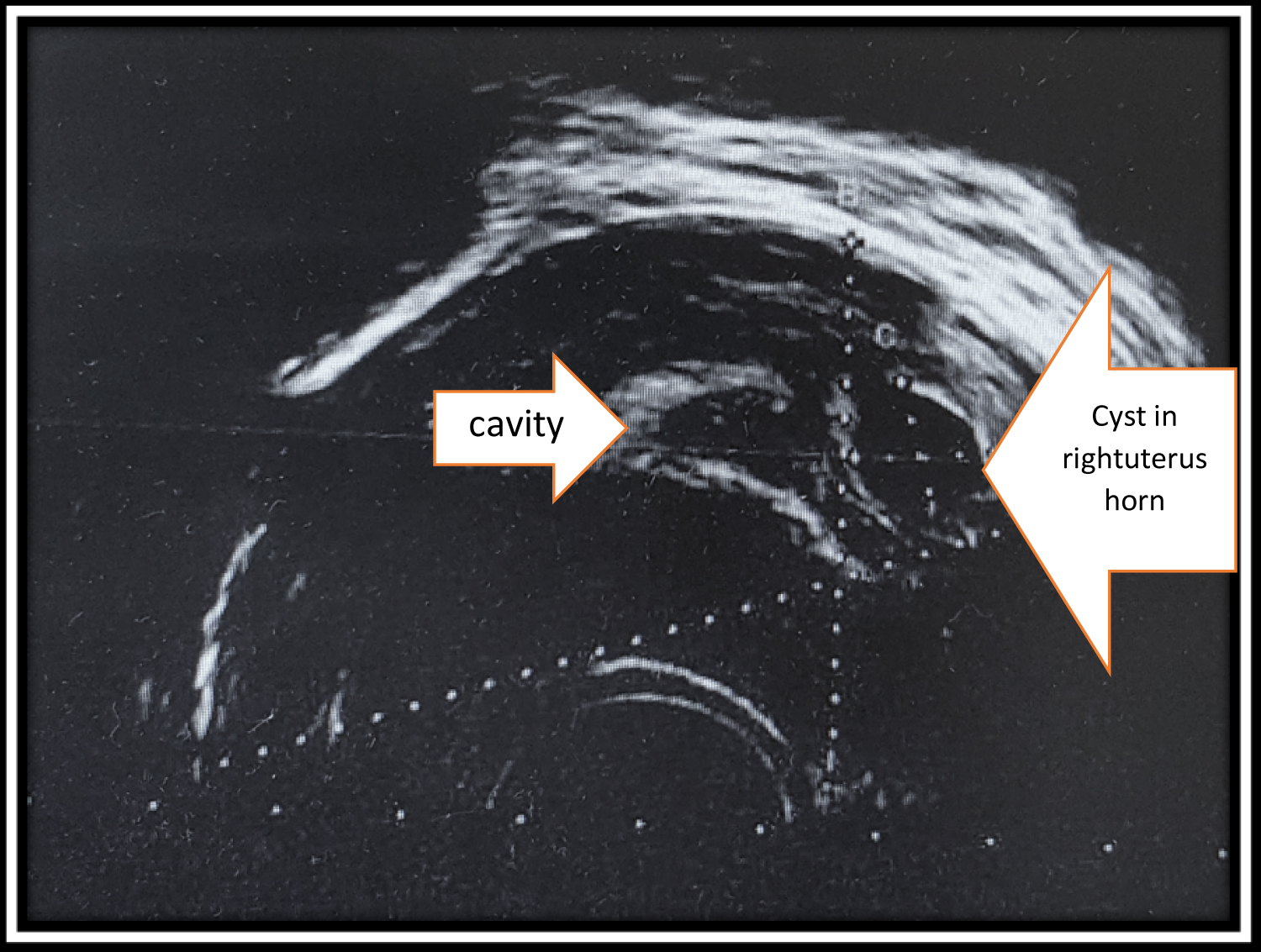 Figure 4: Uterus in sagittal section (8 + 0 gestation weeks).
View Figure 4
Figure 4: Uterus in sagittal section (8 + 0 gestation weeks).
View Figure 4
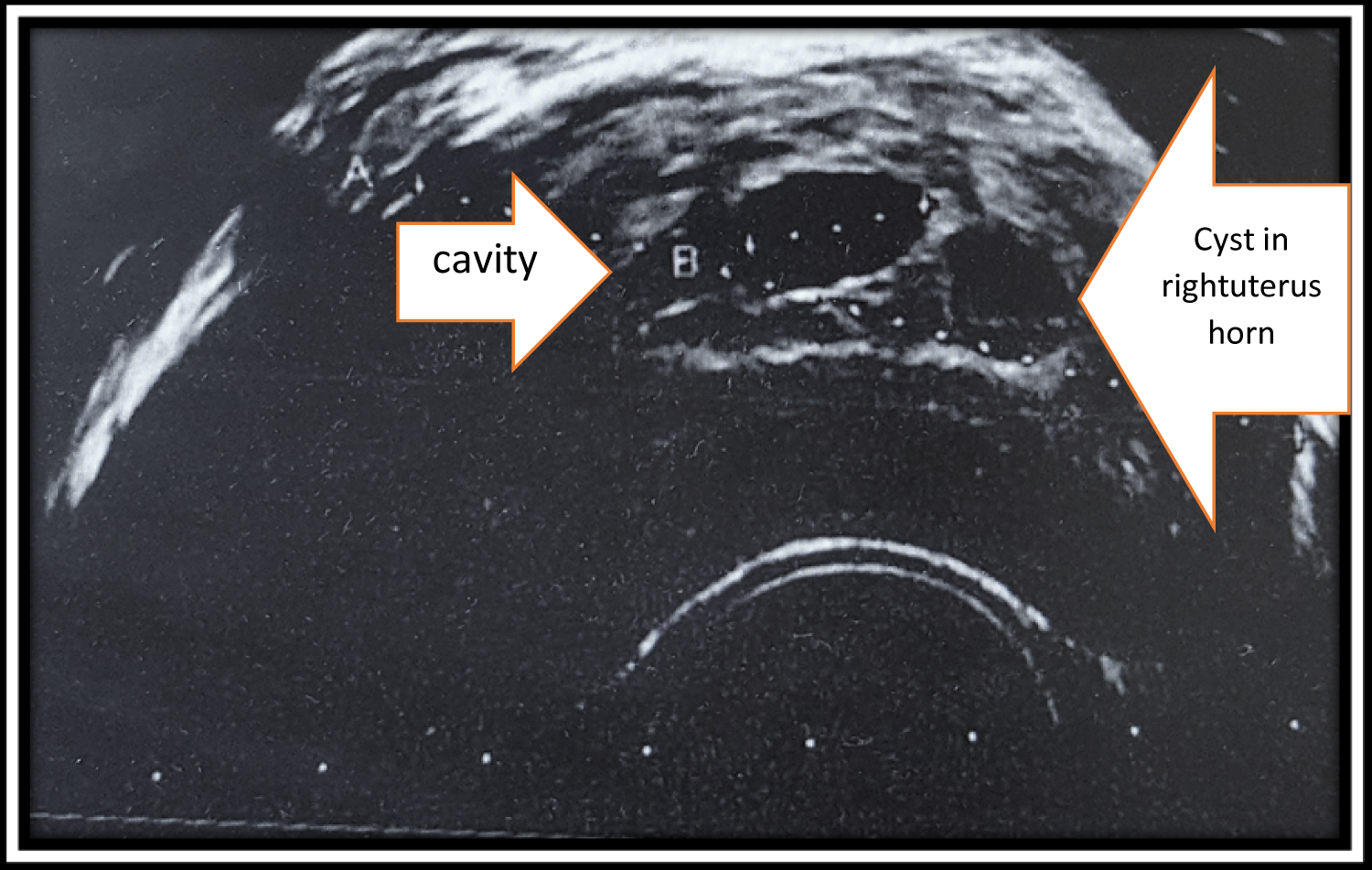 Figure 5: Uterus in cross section (8 + 0 gestation weeks).
View Figure 5
Figure 5: Uterus in cross section (8 + 0 gestation weeks).
View Figure 5
The patient underwent surgery on the same day. In the curettage, a lot of pregnancy-typical material was obtained. Subsequently, laparoscopy took place. Intraoperatively, a protrusion was present at the angle of the right fallopian tube. Through an incision with a monopolar needle and chocolate-like secretion was drained off. Also, endometrial-typical tissue emerged. Wedge resection was carried out with removal of the entire endometrial tissue after injection of diluted adrenalin. The wound was treated with resorbable suture material (Figure 6).
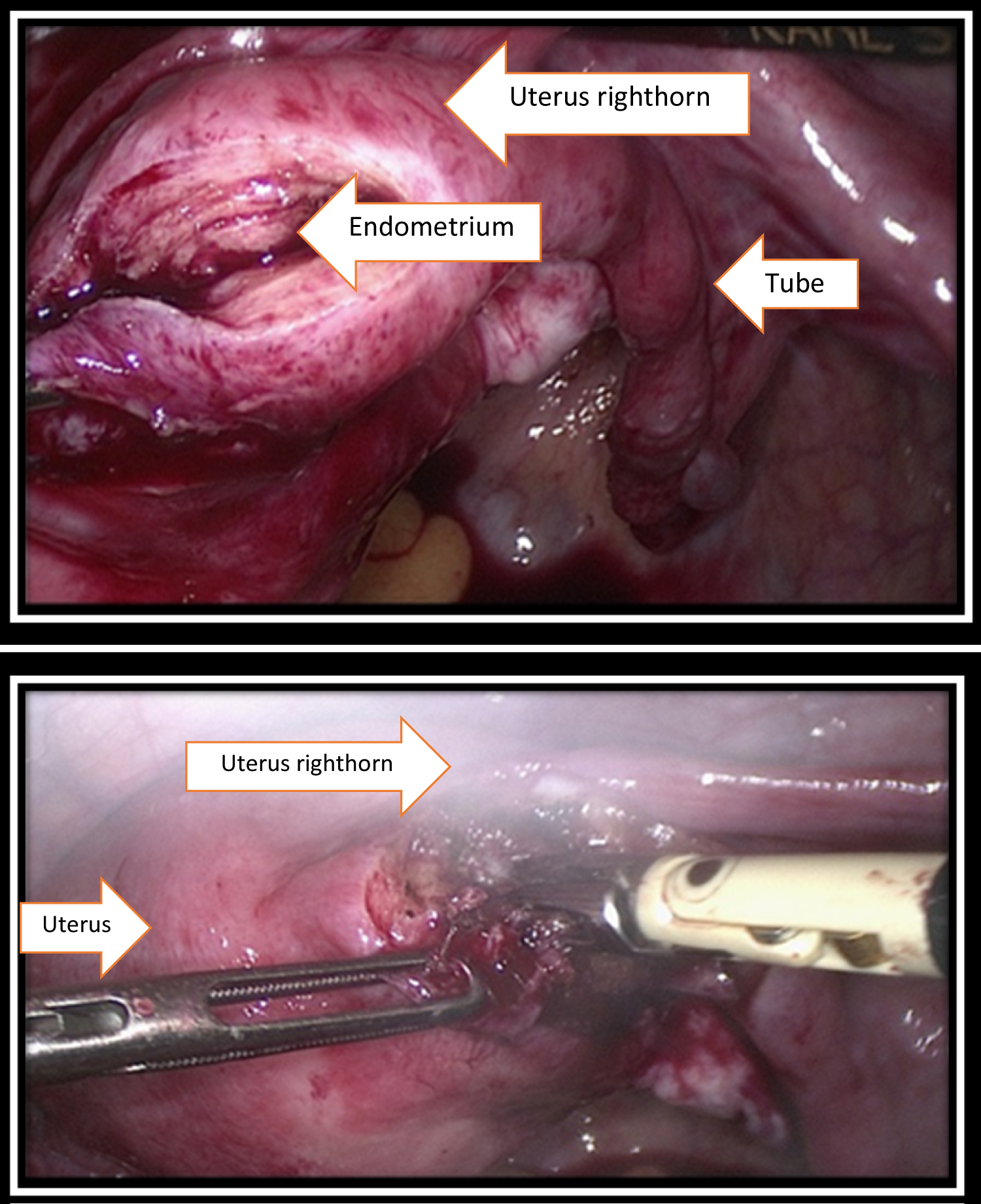 Figure 6: Wedge resection was carried out with removal of the entire endometrial tissue.
View Figure 6
Figure 6: Wedge resection was carried out with removal of the entire endometrial tissue.
View Figure 6
Postoperatively, the patient became free of complaints. After inconspicuous checks, she was discharged after two days in good health.
Histological processing of the obtained material showed following results:
I. Abortion material: Gestational sac with hydropic regressive changes and part of pregnancy-typical endometrium.
II. Uterine exudation: An endometriosis with a moderate degree of proliferative activity: Ki 67 of 10%.
In this case two findings were seen at once: On one hand, there was a pregnancy and subsequent early spontaneous abortion. On the other hand, the patient had a nodular adenomyosis in the right uterine horn, which developed further during pregnancy. The β-HCG value fell to 1288 mIU/ml on the first postoperative day. The further postoperative controls were inconspicuous.
In local adenomyosis, uterine-preserving resection can take place. In nodular adenomyosis, a resection or a volume reduction of adenomyosis can be sought. The adenomyoma should be resected, similar to the management of uterine fibroids, especially in patients who wish to have children with findings > 4 cm [9,10]. However, the procedure of resecting adenomyoma is technically more demanding than extracting myomas, because adenomyoma is destroying the myometrium whereas myomas merely displace the myometrium [11].
If pregnancy is excluded, hormonal therapy can also be performed. Progestins are available in the various application forms. Orally, combined ovulation inhibitors can be used especially in the long-cycle regime as well as progestogen-only preparations. Using a LNG-IUS locally is also worth considering, because there is a very good data situation for Levonorgestrel containing intrauterine device (LNG-IUS) [12].
The treatment of cornual pregnancy is distinguished in surgical and drug therapy with methotrexate. However, in cornual pregnancies, wedge resection with removal of the entire chorial tissue appears to be the therapy of choice [13].
The clinical differential diagnosis between nodular adenomyosis in an angle of fallopian tube during pregnancy and a cornual ectopic pregnancy is very difficult. Sonography can be a valuable tool in diagnosis. In the case of a gestational sac in an angle of fallopian tube, one should think of an interstitial or cornual localization of a EUG. However, even in nodular adenomyosis a cystic finding may form as it was proven in our case. Therefore, in order to formulate a precise and reliable diagnosis a laparoscopy with tissue removal for histological may be necessary.
The authors declare that they have no conflict of interest.
This manuscript was not funded.
The patient has consented to this manuscript.
This manuscript was carried out in consensus with our university´s ethics guidelines.