Abdominal ectopic pregnancy is a more complicated and severe situation, as compared with tubal pregnancy. Accurate differential diagnosis between abdominal and tubal pregnancy is important before the choice of laparoscopic approach. We presented the use of contrast-enhanced computed tomography (CT) to diagnose an unusual presentation of large tubal pregnancy mimicking abdominal pregnancy.
A 24-year-old woman presented to emergency room (ER) with acute abdominal pain. Transabdominal ultrasound demonstrated an empty uterus, a 6 cm crown-rump length (CRL) live fetus about 12 weeks of gestation of uncertain location, and massive hemoperitoneum. Due to the lack of high-resolution transvaginal ultrasound available in ER, the initial transabdominal ultrasound failed to clarify the extent of placental involvement. Contrast-enhanced CT scan revealed that placenta was located in the right adnexa, without omental and bowel and other peritoneal cavity seeding. Meanwhile, the blood supply of placenta was well visualized and located, without connection with surrounding tissue. Thereafter, we choose laparoscopic approach. During operation, we found an engorged ampulla on the right Fallopian tube with a live fetus inside, the internal blood loss was 3800 mL. Right salpingectomy was done; the surgical specimen was then removed via a mini-laparotomy. The patient recovered well and was discharged without any sequelae.
Contrast-enhanced CT scan is useful to offer an accurate differential diagnosis between abdominal and tubal pregnancy before the use of laparoscopic approach.
Abdominal pregnancy, Computed tomography (CT), Magnetic resonance imaging (MRI), Hemoperitoneum, Tubal pregnancy, Minimal invasive surgery
Ectopic pregnancy is not an uncommon condition, the incidence is around 1-2% among all pregnancies, and gets higher to 2-5% in assisted reproductive technology [1,2]. Abdominal ectopic pregnancy, the implantation within the peritoneal cavity, is a more complicated and severe situation, with an incidence of 1:30,000 pregnancies [3,4]. The diagnosis of abdominal pregnancy is usually difficult and often missed with the use of traditional transabdominal ultrasound imaging. The presentation of abdominal pregnancy varies in wide range, either primary or secondary. Primary abdominal pregnancy is a direct implantation on abdominal cavity, e.g. the omentum, pelvic side wall, peritoneum, or uterine serosa; while secondary is the reimplantation after tubal abortion or rupture [5]. The maternal morbidity and mortality of abdominal pregnancy is as high as 90 times to normal pregnancy, and 7.7 times to tubal pregnancy [6]. The fetus of abdominal pregnancy is usually non-viable; only some rare case reports of viable full-term pregnancy. In most circumstances, abdominal pregnancy usually develops a poor outcome, even devastating sequela.
The choice of treatment of abdominal pregnancy depends on the size and the site of placental implantation, which is more complicated than that of tubal pregnancy. Due to surgical complexity, exploratory laparotomy is more commonly used to determine the extent of placental implantation, especially in well vascularized location Laparoscopic approach is only indicated in more simple situation [7]. Therefore, accurate differential diagnosis between abdominal and tubal pregnancy is important before the use of laparoscopic approach.
We herein presented an unusual presentation of large tubal pregnancy mimicking abdominal pregnancy. We used contrast-enhanced computed tomography (CT) scan to accurate diagnose, followed by a laparoscopic approach.
A 24-year-old woman, married, gravida 1 para 0, presented to our emergency room (ER) due to sudden onset of severe diffuse abdominal pain for 1 day. Before ER visit, she only had mild to moderate lower abdominal pain for 1 week, and intermittent vaginal spotting for 3 months. She was not aware of her pregnancy, therefore, she did not receive any prenatal care nor healthcare visits.
At ER, she was ill looking with pale conjunctiva, pulse rate was 146 beats/minute; blood pressure was 114/72 mmHg. Physical examination revealed peritoneal signs with diffuse abdominal tenderness, muscle guarding, and rebounding pain. Laboratory examination suggested normocytic anemia, with hemoglobin 6.6 g/dL, hematocrit 19.9%, and beta-HCG levels of 163,663.2 mIU/mL. Immediate resuscitation with large-bore catheters was given for intravenous fluid supplement and blood transfusion. A transabdominal ultrasound illustrated an empty uterus, an extrauterine live fetus, and massive hemoperitoneum (Figure 1). Transabdominal ultrasound demonstrated a 6 cm crown-rump length (CRL) live fetus about 12 weeks of gestation. The internal blood loss was estimated over 2000 mL, evidenced by fluid accumulation up to Morrison's pouch and splenorenal fossa. The initial clinical and image study suggested of an abdominal pregnancy.
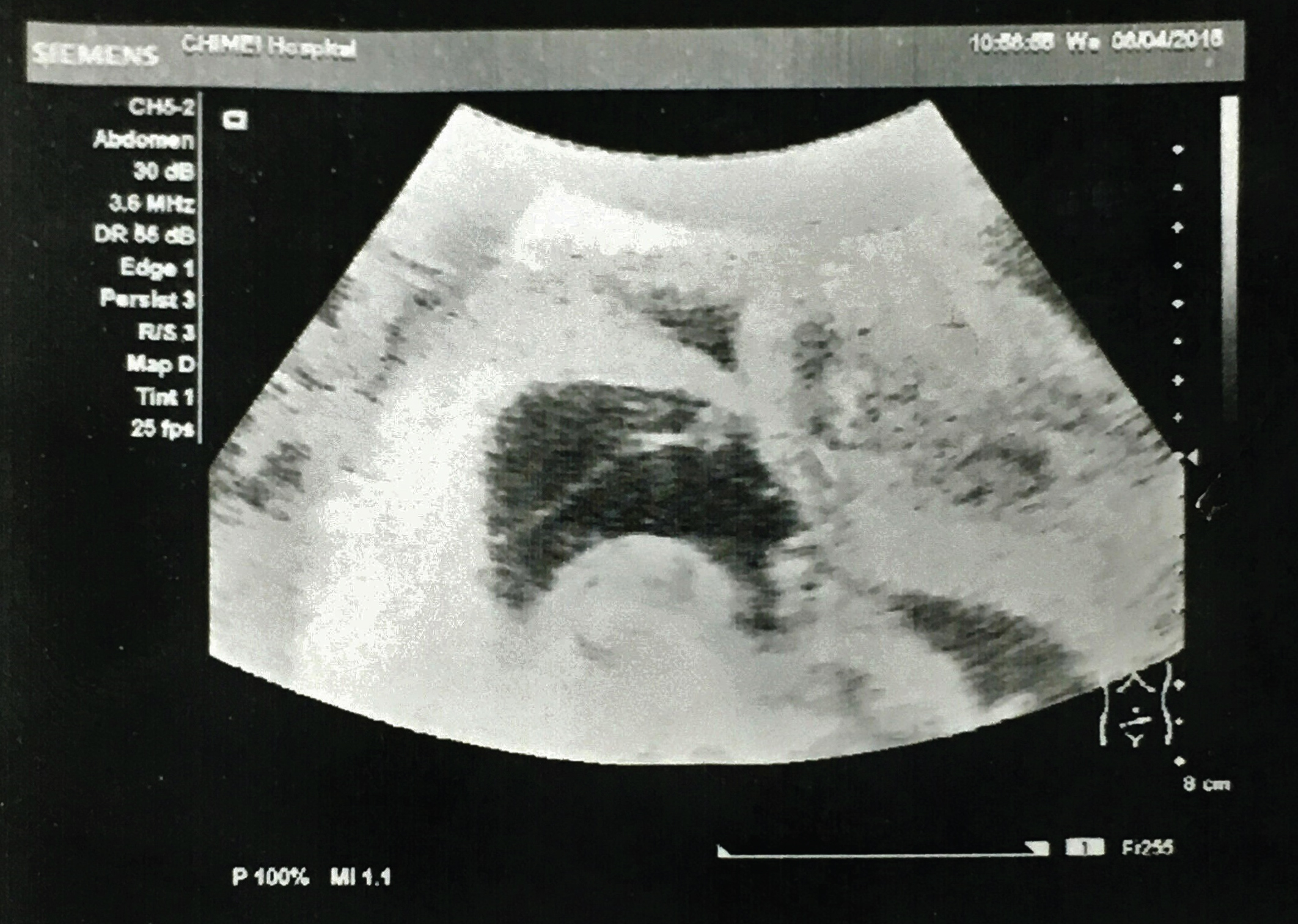 Figure 1: Transabdominal ultrasonography demonstrated an empty uterus (upper right), an extrauterine live fetus within an intact gestational sac (lower left), and massive hemoperitoneum.
View Figure 1
Figure 1: Transabdominal ultrasonography demonstrated an empty uterus (upper right), an extrauterine live fetus within an intact gestational sac (lower left), and massive hemoperitoneum.
View Figure 1
It was difficult to clarify the extent of placental involvement via transabdominal ultrasound. Due to risk for transferal to other examination room where tranvaginal ultrasound is available, we proceeded to contrast-enhanced abdominal CT scan examination. CT scan was used to differential diagnosis between abdominal and tubal pregnancy, before the surgical decision, either laparotomy or laparoscopy. We have explained to the patient and her family, that CT scan for localization of the ectopic gestational tissue (including placenta), may affect our decision for either laparoscopy or laparotomy. We chose CT scan, instead of magnetic resonance imaging (MRI), due to the availability of CT scan in our ER.
Emergent CT scan revealed that placenta was located in the right adnexa, without omental and bowel and other peritoneal cavity seeding. Meanwhile, the blood supply of placenta was well visualized and located, without connection with surrounding tissue (Figure 2). After CT scan offered a better localization of placental implantation and involvement, the diagnosis of tubal pregnancy was confirmed. Although the patient has massive internal bleeding, we set up large volume of IV fluid supplement, and blood transfusion. In the meanwhile, operation room was also preparing in the same time.
 Figure 2: CT scan revealed that placenta was located in the right adnexa, without omental and bowel and another peritoneal cavity seeding. The blood supply of placenta was well visualized and located from right ovarian artery (arrow), without connection with surrounding tissue.
View Figure 2
Figure 2: CT scan revealed that placenta was located in the right adnexa, without omental and bowel and another peritoneal cavity seeding. The blood supply of placenta was well visualized and located from right ovarian artery (arrow), without connection with surrounding tissue.
View Figure 2
Thereafter, we choose laparoscopic approach. Laparoscopic approach for ectopic pregnancy with massive bleeding is commonly performed in our hospital, a tertiary referral medical center. During operation, we found an engorged ampulla on the right Fallopian tube, within a live fetus, the internal blood loss was 3800 mL (Figure 3). Right salpingectomy was done; the surgical specimen was then removed via a mini-laparotomy about 4 cm (Figure 4). The patient recovered well, and was discharged without any sequelae.
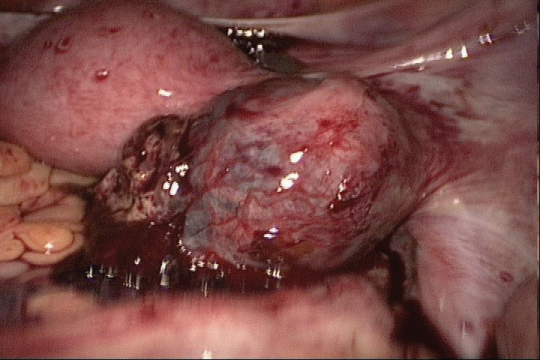 Figure 3: Laparoscopic view, right tubal pregnancy was confirmed. The whole gestational sac was even larger than the uterus.
View Figure 3
Figure 3: Laparoscopic view, right tubal pregnancy was confirmed. The whole gestational sac was even larger than the uterus.
View Figure 3
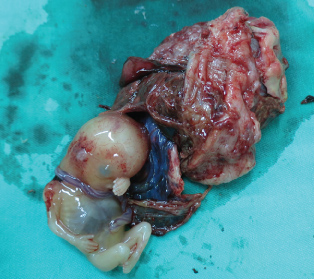 Figure 4: Right salpingectomy with specimen was removed via a mini-laparotomy. The incised tissue showed intact fetus within the gestational sac.
View Figure 4
Figure 4: Right salpingectomy with specimen was removed via a mini-laparotomy. The incised tissue showed intact fetus within the gestational sac.
View Figure 4
Abdominal pregnancy is a life-threatening condition, because of it commonly presented with massive hemoperitoneum and unstable vital signs. The difficulty of abdominal pregnancy treatment depends on the variable placental implantation sites, the extensive involvement of adjacent surrounding tissue, and vigorous surrounding blood supplies. Therefore, expectant management in abdominal pregnancy is only suitable when the placental implantation site is limited on the uterine wall, with relatively limited blood supply. Life threatening complications may occur when implantation onto omentum, bowel, ovarian ligament, liver surface, etc [5].
It is thus crucial to determine the accurate placental implantation site when the surgical treatment is imminent. Advanced image plays an important role to develop a relatively safe and reasonable treatment option and surgical planning [8]. MRI, when available, can be used to localize and identify the spatial relationship between the placenta and the adjacent organs and surrounding tissues. However, MRI is more time-consuming, expensive, and not easily available in ER setting in most of the hospitals, also in our case. We used contrast-enhanced CT scan to identify the location, extent, and blood supply of placental implantation (Figure 2). The reasons we arrange an abdominal CT scan evaluation first, before we sent the patient for an emergent exploratory laparotomy were: 1) CT scan facility is well provided and easily available in our ER setting; 2) The CT scan for localization of the ectopic gestational tissue (including placenta), may affect our decision for either laparoscopy or laparotomy. After the adequate image study, we could confidently choose minimal invasive approach without risking the patient safety.
In our case, laparoscopic salpingectomy and the removal of the ectopic gestational tissue was not difficult, since there were only a few vessels connected to the Fallopian tube. Laparoscopic approach with well hemostasis avoided the conversion to exploratory laparotomy, which may need more blood transfusion, more analgesia doses, more post-operative hospital stays, and more time to return to normal daily living [9].
In conclusion, contrast-enhanced CT scan is useful to offer an accurate differential diagnosis between abdominal and tubal pregnancy before the use of laparoscopic approach.
All authors declare no conflict of interest.