Background: Mullerian duct anomalies are congenital defects of the female reproductive tract which arise from an error in development of the Mullerian ducts. A didelphys uterus is one of the rarest mullerian duct anomalies.
Case: Patient is a 27-year-old G2P1001 from Michigan, found to have spontaneous dichorionic diamniotic twin gestation in the setting of known uterine didelphys, with a twin localized to each uterine horn. Both twins were affected by severe fetal growth restriction, and the patient ultimately delivered via cesarean section at 29 weeks gestation, secondary to HELLP syndrome. Cesarean section was complicated by fetal malpresentation, requiring T-incision, and elevated quantitiate blood loss of 1400 mL.
Conclusion: Uterine didelphys may result in increased risk for obstetrical conditions related to placentation particularly in the setting of twin gestation.
Uterine didelphys is categorized as a class III Mullerian anomaly according to the American Society of Reproductive Medicine (ASRM). Patients with this type of anomaly are typically asymptomatic outside of pregnancy but are suspected to be at increased risk of adverse pregnancy outcomes, such as increased risk of fetal malpresentation, preterm birth, fetal growth restriction, and cesarean delivery compared to those with normal uterine anatomy [1-3].
Prevalence of uterine didelphys in the general population is rare; in a systematic review on the prevalence of congenital uterine anomalies, the study team found a prevalence of 0.3% in the general population [3]. The rate of dicavitary twin pregnancy in the setting of didelphys uterine anomaly is even lower, with one case report estimating the rate of appropriate conditions for such an occurrence at 8 in 10^7, or approximately 1 in one million [4]. We present a case of a patient with a known uterine didelphys and a spontaneously conceived dichorionic/diamniotic twin gestation. Her pregnancy was complicated by severe fetal growth restriction of both twins, development of HELLP syndrome necessitating urgent pre-term delivery due to concern for maternal condition, and fetal malpresentation at time of delivery.
A 27-year-old gravida-2 para-1 abortus-0 with spontaneously conceived dichorionic diamniotic twins in the setting of known didelphys uterus ultimately delivered via repeat cesarean due to HELLP at 29 weeks 1 day gestational age.
Didelphys uterus was first diagnosed on initiation of prenatal care during her first pregnancy approximately 2 years prior. Initial pelvic exam was significant for a thick complete vaginal septum with a cervix on either side. The pregnancy, measuring 8 weeks 1 day by transvaginal ultrasound was consistent with LMP, and was found to be in the left hemi-uterus on ultrasound. Given that that pregnancy was complicated by insulin requiring gestational diabetes and uterine anomalies, serial growth ultrasounds were performed. At 37 weeks and 2 days gestation fetal growth restriction by lagging abdominal circumference was diagnosed, with 1 of 3 umbilical artery dopplers abnormally elevated. She was subsequently directed to Labor & Delivery for an OB Triage evaluation.
Work-up revealed preeclampsia without severe features, and induction of labor was recommended. She progressed to 4 cm dilation, but given persistent non-reassuring fetal heart tones remote from delivery, cesarean delivery was performed. The singleton fetus was delivered via low transverse hysterotomy from the left uterus, and intra-operative inspection of the left and right adnexa demonstrated normal anatomy. The male fetus weighed 2470g, ultimately AGA at the 31 st percentile. Her postpartum course was uncomplicated and she was discharged home on postoperative day #2.
She then represented to care for her second pregnancy. On initial ultrasound at 8 weeks gestation, she was found to have spontaneous dichorionic-diamniotic twins, with one fetus in each horn. Low-dose aspirin (162 mg) daily was initiated in the second trimester given her elevated risk for development of pre-eclampsia secondary to a history of pre-eclampsia as well as multiple gestation. Screening ultrasound at 16 weeks 1 day noted growth and amniotic fluid were normal for gestational age, though with a discrepancy in growth of 17%.
At the anatomy screening ultrasound, performed at 20 weeks 6 days, fetal growth of both twins was noted to be lagging, by 11 days for Twin A and by 8 days for Twin B. Follow-up ultrasound at 24 weeks 0 days demonstrated both fetuses measuring at 4 th percentile with normal dopplers. But by the next ultrasound at 26 weeks 1 days, both twins were severely growth restricted, with estimated fetal growth at or below the 1 st percentile by Hadlock, with normal umbilical artery dopplers and amniotic fluid.
At 26 weeks 5 days, she was briefly admitted for observation due to elevated blood pressures at home, subsequently meeting diagnostic criteria for gestational hypertension. During this admission, Twin B was diagnosed with new onset elevated umbilical artery dopplers. She received a course of antenatal corticosteroids given increasing concern for pre-term delivery, but she was ultimately discharged with close outpatient follow-up.
At 29 weeks 1 day, she presented to triage endorsing new onset nausea and vomiting with severe right upper quadrant pain awakening her from sleep. On evaluation, she demonstrated persistently elevated blood pressures systolic 140s to 150s/diastolic 80s to 90s with significant new onset transaminitis (AST 447/ALT 227), thrombocytopenia (Platelets 105k), and proteinuria (urine protein creatinine ratio 0.36). Labs evaluating for evolving HELLP syndrome were equivocal with hemolyzed LDH, stable hemoglobin (11.9 g/dL) and a bump in bilirubin (0.9 up from baseline of 0.2.) Abdominal ultrasound demonstrated a 9.1 × 6.7 cm echogenic area in the right lobe of the liver, etiology was unclear and MRI was recommended.
Given concern for worsening maternal status, decision to move toward delivery was made. Intravenous magnesium sulfate was initiated for fetal neuroprotection and maternal seizure prophylaxis. Fetal status via electronic fetal monitoring was overall reassuring and both fetuses were confirmed breech presentation by ultrasound prior to delivery.
Cesarean delivery was performed under spinal analgesia, with the patient in supine position with leftward tilt and via Pfannenstiel skin incision. Upon entering the peritoneum, the left uterine horn presented closer to the incision, and thus delivery of the fetus in the left horn was performed first. A low transverse hysterotomy was made initially, however, due to compound presentation of the fetal parts through the hysterotomy at time of amniotomy, this was converted to a T-incision to facilitate breech delivery of twin A. Attention was then turned to the right uterine horn and the second fetus was delivered breech through a low transverse hysterotomy without complication. APGAR scores of Twin A were 3 and 8, with the infant weighing 870g (14%) at time of delivery; APGAR scores for Twin B were 1 and 8, with infant weight of 955g (22%) (Figure 1). Intra-operative blood loss was 1400 mL and postoperative day 1 hemoglobin was 9.3 g/dL. She received 24 hours of intravenous magnesium sulfate for maternal seizure prophylaxis postpartum and serial laboratory studies demonstrated improvement of her transaminitis and thrombocytopenia, with stable blood pressure measurements. She was discharged home on post-operative day 3 without any long-acting antihypertensives. 2 months later MRI was performed that was unremarkable and did not demonstrate the liver abnormality initially seen on ultrasound.
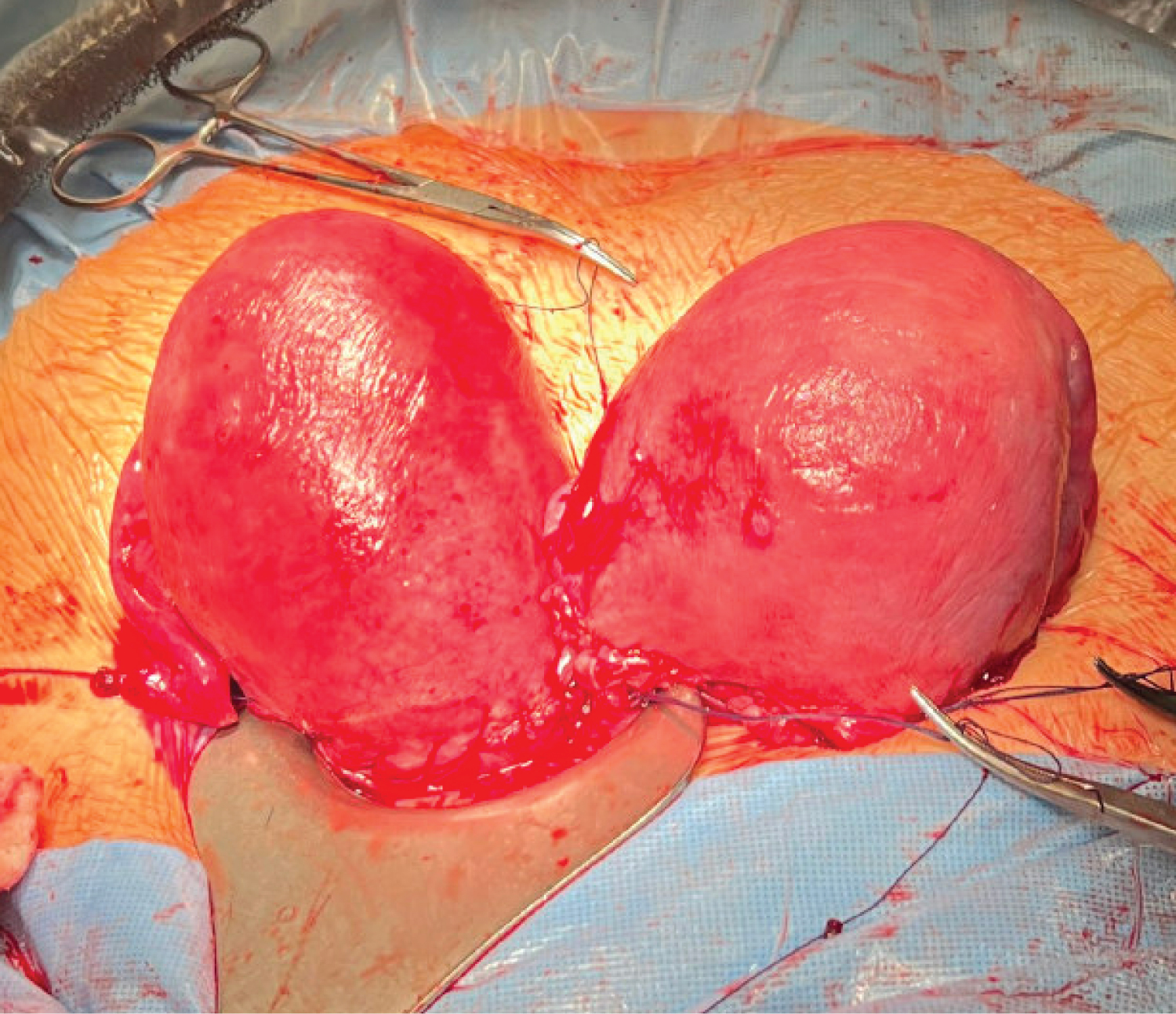 Figure 1: CT - angiography, CT - perfusion and cerebral angiography before endovascular treatment. A) CT - angiogram showing AVM and aneurism localization; B) CT - prefusion showing hyperperfusion zone in AVM and high-flow drainage vein; C) Cerebral angiography showing AVM of the right fronto-parietal region and the proximal flow - related aneurysm on the right terminal ACA afferent.
View Figure 1
Figure 1: CT - angiography, CT - perfusion and cerebral angiography before endovascular treatment. A) CT - angiogram showing AVM and aneurism localization; B) CT - prefusion showing hyperperfusion zone in AVM and high-flow drainage vein; C) Cerebral angiography showing AVM of the right fronto-parietal region and the proximal flow - related aneurysm on the right terminal ACA afferent.
View Figure 1
The goal of presenting this case was to contribute to the body of literature regarding dicavitary twin pregnancies in patients with known uterine didelphys. Review of available literature regarding pregnancy outcomes in patients with uterine anomalies suggests increased risk of adverse pregnancy outcomes. However, data regarding twin pregnancies in these patients, particularly in patients with uterine didelphys, has been limited to case reports.
Review of these reports suggests that it is difficult to assess whether the elevated risk of adverse pregnancy outcomes is primarily due to the presence of the uterine anomaly or due to the nature of a twin gestation. For example, despite the increased risk for cesarean delivery, successful vaginal delivery is possible under appropriate conditions and that uterine didelphys alone is not an indication for cesarean delivery [5,6]. Additionally, pre-term delivery is a common outcome of these pregnancies, but can be achieved in the late pre-term period (32 weeks and beyond) with good maternal and neonatal outcomes [5,7]. Our case was complicated by the development of severe maternal hypertensive disease as well as severe fetal growth restriction but the extent to which uterine anomalies played a role is unknown.
We did not receive any financial support of the study from a commercial organization.
We did not receive any funding including from organizations such as NIH.