Retroperitoneal hematomas following vaginal delivery are life threatening rare complication in obstetrics. There is no report showed that identification of retroperitoneal hematoma following vaginal birth after cesarean (VBAC) in the literature.
Case presentation: A 35-year-old G3P1A1, VBAC patient, presented in the clinic with severe rectal pain a few hours following uncomplicated vaginal delivery with small mediolateral episiotomy. In initial findings, patient was hypotensive and tachycardic. The hemoglobin (Hb) measurements were low (postpartum to 8.6 g/dL). Episiotomy was reopened 2 hour later after delivery. Huge right pelvic hematoma, approximately 12 cm diameter, was drained and multiple tight sutures were carefully replaced every layer of perineum and bleeding was taken under control. Hb level was risen to 10.4 g/dL after transfusion of 2 units of packed red blood cells (RBC). Patient was stable with no pain and her vital signs were normal at postoperative intensive care. However, the Hb level was measured low in follow-ups to 6.4 g/dL at postpartum 12 hours. Evaluation of MRI showed large extraperitoneal bleeding which was reaching from perinea to umbilicus and surrounding bladder bilaterally. No fluid was detected in Douglas pouch. There was a huge hematoma, so immediately active management of postpartum bleeding was performed. Blood supplies was given, close monitoring of her vital sign and coagulation parameters was measured. The operation was performed conservatively because vital signs were normal. Patient was stable postoperative days and discharged from hospital on the 7th day.
Postpartum hematomas should be managed carefully. Surgical removal and arterial embolization are the treatment options of postpartum hematoma.
Retroperitoneal hematoma, VBAC, TOLAC, Dinoproston, Conservative management
Postpartum retroperitoneal hematomas are rare life-treatening obstetric complication following vaginal or cesarian delivery Patient can admit to hospital with just simple pelvic pain to hypovolemic shock [1]. It has been mentioned mostly with case reports. Accurate incidence and management of this complication are difficult [2]. Even though, etiology remains unclear, the traction and damage to pelvic veins during the second stage of labor or episiotomy repair are most common causes for this complication and can’t be completely ruled out [3].
In Turkey, there is no established national guidelines for diagnosis and treatment of VBAC, physicians are following the international guideliness [4]. During prenatal visits, VBAC score is calculated depending on patient age, ethnicity, body mass index (BMI), previous obstetric history and interdelivery interval and this score is used for the management strategies of VBAC [5]. Previously, data is getting acumulated about VBAC [4], so we want to make a contrubition about our experience.
This case report summarizes a case of retroperitoneal hematoma that developed at 3 hours following an uncomplicated vaginal delivery. This is the first case with retroperitoneal hematoma during VBAC trial in the literature.
A white, 35-year-old woman (gravida 3, para 1, abortus 1) at 40 weeks 2-day pregnancy, who was eligible for VBAC after 9 years of uncomplicated cesarian section (CS), was admitted to our clinic and hospitalized at Jan 2022 for labor induction with diagnosis of oligohydroamnios. On previous prenatal visits, predicted chance of VBAC was calculated around 60-70%. Her BMI was around 25. She had no specific previous medical history, drug usage or surgery except CS at previous pregnancy. She had an emergency CS in 2013, 9 years ago with the diagnoses of small gestational age + rupture of membranes + anhydroamniosis.
Cervix was central, soft, open (2 cm) but tight, her bishop score was 7, slightly unfavorable, so dinoprostone was placed to posterior fornix for induction of labor. The latent phase continued for 3-4 hour and active phase was 3-4 hours, respectively. Small right mediolateral episiotomy was performed to reduce afterload of uterus. The newborn weighed 3050g and was in good health on an initial assessment (APGAR scores was 8 and 9, respectively). Her uterine tonus was toned, and episiotomy cut was clear. After episiotomy repair stiches, patient was transferred to postpartum section of service. After 3 hours, she began reporting bulging and severe pain on her episiotomy area. On pelvic exam, we found that she had approximately 6 cm hematoma under the incision. Her control Hb level was 11.6 g/dL however postural hypotension and tachycardia was detected in physical examination. Under anesthesia and antisepsis conditions, patient underwent surgery. During the operation, pelvic hematoma was drained out vaginally but there was great crater in the right side of perineum; (left wall of crater was rectal mucosa, posterior and right wall was levator ani muscle). Compression sutures were carefully applied every layer of perineum. Intraoperative control Hb was 8.6 g/dL. After 2 units packed RBC infusion, her Hb rose up to10.4 g/dL. Her pain score was relief and vital signs were within normal limits. Wound care and broad-spectrum antibiotics were started intravenously.
She was cooperative and oriented but in postop 14 hours period, her follow-up Hb level started dropping from 10.4 to 8.6, 6.9 and 6.7 respectively. Most serious complication of VBAC for patient including doctor is uterine rupture. Transvaginal and suprapubic ultrasound was performed to rule out this diagnosis immediately, and USG showed that uterus was intact, and no fluid was found in Douglas pouch. Pelvic MR showed that big (measurements) retroperitoneal fluid was all around the pelvis reaching umbilicus and was squeezing the bladder bilaterally (Figure 1a, Figure 1b and Figure 1c). Patient was stable. Under analgesia her pelvic pain was absent, and her abdominal examinations were normal. Even though patient was stable, 2 nd surgery was considered to manage postpartum hemorrhage. There was a chance that another surgery to patient and surgical evacuation might lead to loss of the advantages of the tamponing effect on the bleeding source which could result in undue dissection and end up with a fatal outcome. So, we decided to follow up the hematoma conservatively with close, careful monitoring. Tersier referral hospital was informed about possible arterial embolization, or another further surgery as needed.
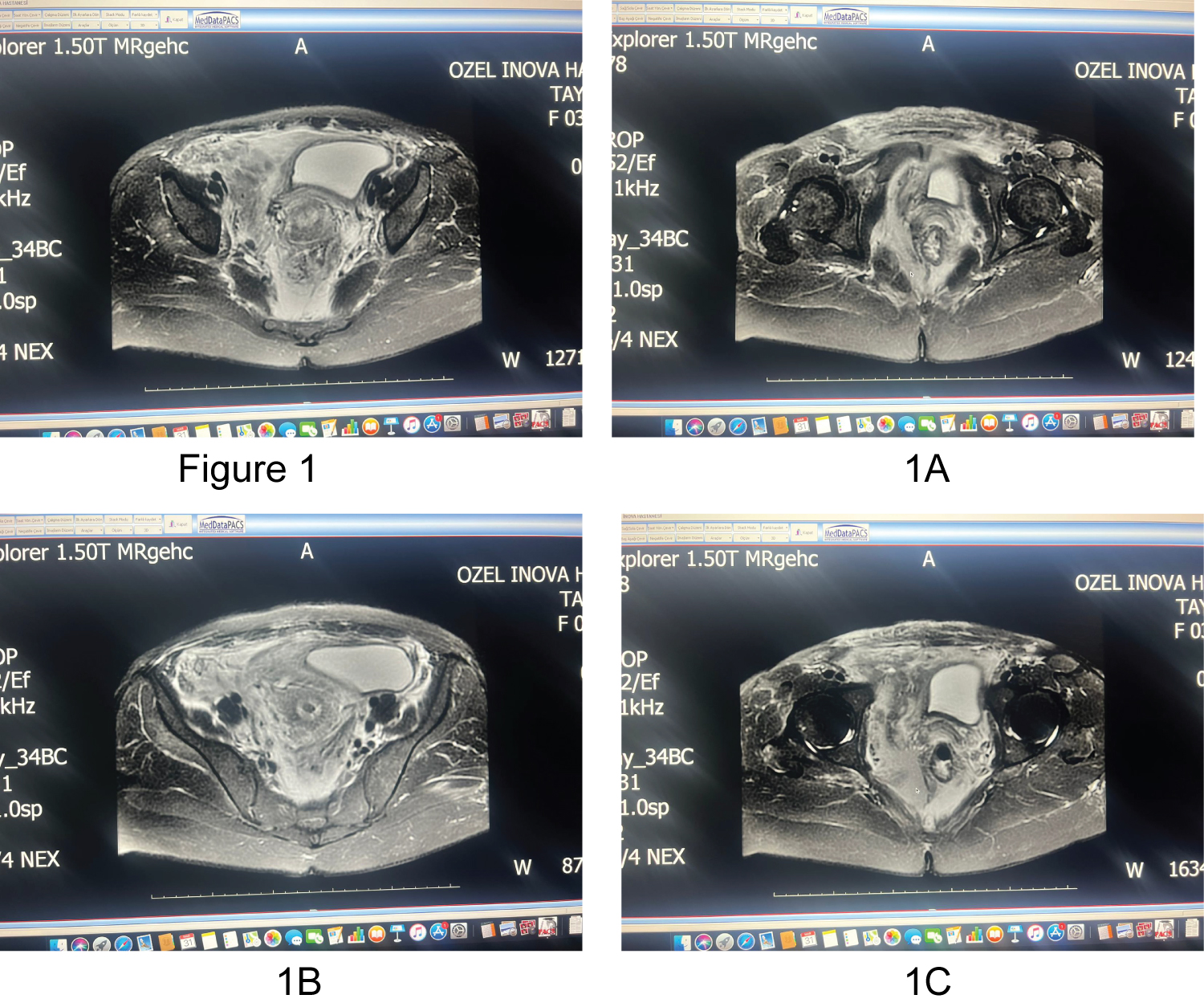 Figure 1: MR showed that big dissemine retroperitoneal fluid was all around the pelvis reaching umbilicus and was squeezing the bladder bilaterally. (a) T1 weighted fat-suppressed transvers MR imaging; (b) T1 weighted fat-suppressed sagittal MR imaging; (c) T2 weighted transvers MR imaging.
View Figure 1
Figure 1: MR showed that big dissemine retroperitoneal fluid was all around the pelvis reaching umbilicus and was squeezing the bladder bilaterally. (a) T1 weighted fat-suppressed transvers MR imaging; (b) T1 weighted fat-suppressed sagittal MR imaging; (c) T2 weighted transvers MR imaging.
View Figure 1
The patient was transfused 3 more units of packed RBCs (totally 5 unit packed RBCs) and 2 unit fresh frozen plasma (FFP). Her coagulation parameters, especially fibrinogen level was within normal range (What were the measures?). Transamine was given two times to lead coagulation better [6]. The patient was closely monitored for a week with supportive treatment. The patient became more stable and was finally discharged from hospital on the 7 th day.
She was fully recovered with no sequelae and showed no signs of hematoma at her 2-month follow-up. Second abdominal MRI was planned at 3 month follow up, May 2022 to check resolution of hematoma.
Postpartum retroperitoneal hematomas are rare, life-threteaning obsterics complications. There is no actual incidence and management algoritm [2]. The literature shows in only case reports, and different managements of this complication. Also, our patient is the first case of TOLAC with complication of retroperitoneal hematoma.
Recently, more TOLAC case were diagnosed [4]. Risk factors, contraindications and complications are getting more clear but still we do not have certain criterias and/or national guidelines for Turkey. We are guided by literature and our best knowledge on patient experience is the key point for the management. Patient age, ethnicity, BMI, previous obstetric history and interdelivery interval are the factors that effects TOLAC decision [5].
Risk factors for retroperitoneal hematoma includes multiparity, macrosomia, preeclampsia, prolonged second stage of labour, multi-fetal pregnancy, vulvar varicosities, pregnancy itself and blood clotting disorders [1,7-10].
Our case was a TOLAC patient, her induction went well, first and second stage of labor progressed well with no delay. Small episiotomy was performed to reduce afterload of uterus and help us for management of TOLAC. Fetus was relatively small. Delivery went uneventfully. Maternal age and BMI is favorable. There was no presense reason for excessive bleeeding.
Some of the reported iatrogenic causes of puerperal retroperitoneal hematomas include traumatic deliveries, manual removal of placenta, inadequate hemostasis at CS, and anticoagulation therapy [11]. Our patient did not have any of these situations.
As in our patient, most common sings of hematoma are postural hypotension, tachycardia and pain. So, we needed to drain out pelvic hematoma via vaginal route because of pain and hemodynamic status of patient. After evacuation of right pelvic hematoma, huge crater left in there so compression sutures were carefully applied to every layer of perineum. After surgery, pain was relieved, vitals signs were normal however hemoglobin level started to drop again at postop 12 hours. Most crucial complication of TOLAC is uterine rupture [12] but MR and ultrasound showed that bleeding was in extraperitoneum and myometrium was intact. Retroperitoneal hematomas occur as a consequence of injury to branches of the internal iliac arteries. The majority of cases occur in the context of uterine artery lacerations during hysterectomy, uterine rupture, or as an extension of a paravaginal hematoma [3].
Our hypothesis of about that complication is, pelvic area was taken undercontrol with sutures but bleeding has still continued from pelvic venous plexus to all around the lower abdomen until umbliculus. After MRI report, we thought that there was a chance to damage the venous plexus during the surgery but there was a huge crater after evacuation so it could be happened before surgery. These veins could be damaged on the second stage of labor or could be damaged during episyotomy. There is a slight possibility that our patient have undiagnosed mild bleeding disorder related with connective tissue or coagulation cascade and paravaginal hematoma extened from pelvic floor to umbliculus.
Management of retroperitoneal hematomas are conservatively, surgically, or through use of angiographic embolization [13]. The patient’s hemodynamic stability plays a key role in the management plan. Conservative management is usually preferred for hemodynamically stable patients with no active bleeding [13]. Fortunately, our patient was hemodynamically stable so we could treated her conservatively.
If it is available, selective arterial embolization (SAE) is more appropriate treatment option because pelvic blood supply is more complicated and source of bleeding during laparotomy can’t be identified. Also, surgery can remove tampon effect of coagulum and cause to restart bleeding again. Surgery can be preferred at selective cases. For further surgery or SAE application we had been in contact of referral center.
Postpartum retroperitoneal hematomas must be managed carefully. Timely diagnosis and management properly are essential. It is rare and dangerous complication of obstetrics. Suspicion and awareness of this complication is the key attitude and it should be considered at TOLAC pregnancies. Management of that complication should carefully apply according to patient status, hospital set up and clinical expertise.
TOLAC experience of clinics are getting rise and this case contribute to literature about that rare complication, retroperitoneal hematomas, on TOLAC patients.