Spontaneous uterine vessel rupture in the peripartum period is a rare but life-threatening condition. We report an unusual case of a spontaneous rupture of uterine vessels leading to hypovolemic shock, two hours postpartum. A 32-year-old patient, gravida 2 para 1, had a first uneventful pregnancy. She now had an induction of labor at a gestational age of 40 weeks 3 days, using prostaglandins, artificial rupture of membranes and oxytocin. Epidural analgesia was used for pain relief. After a short second stage of labor followed by a normal vaginal delivery, a girl with a birth weight of 4060g was born. Third stage labor was uneventful, and there was no abnormal blood loss. Hypovolemic shock was diagnosed after two hours. Clinical examination showed an abdominal tenderness. Bedside ultrasound showed a large amount of free fluid intra-abdominally. There was no abnormal vaginal bleeding. An urgent abdominal CT scan diagnosed a suspicion of spontaneous uterine rupture and a spontaneous rupture of uterine vessels on the posterior right side of the uterus. An urgent laparotomy was performed with hemostatic sutures and clipping of the vessels. Postoperative follow-up was without events. She was discharged ten days postpartum.
Spontaneous rupture of uterine vessels in the peripartum period, causing intraperitoneal hemorrhage, is a very rare but potentially life-threatening condition. A recent review of literature noted that are less than 100 reported cases of spontaneous rupture of uterine vessels in pregnancy or postpartum [1]. A case report stated that only five of them were reported during labor [2]. We need to acknowledge the difference between a spontaneous rupture of uterine vessels and a spontaneous rupture of the unscarred uterus, both leading up to an intraperitoneal hemorrhage. A spontaneous uterine rupture in the peripartum is also a very rare but severe complication with an incidence of 1 in 15 000 deliveries but will not be further discussed here [3]. Spontaneous rupture of a uterine vessel in the peripartum period may result in an intraperitoneal hemorrhage, leading to hypovolemic shock, need for blood transfusion, immediate imaging and urgent laparotomy or embolization [4].
We report a rare case of a spontaneous rupture of uterine vessels, diagnosed in the early postpartum period in a 32-year-old woman after a second successful vaginal delivery.
A 32-year-old woman, gravida 2 para 1, with no medical history was admitted for a planned induction of labor. First pregnancy was an uncomplicated pregnancy and vaginal delivery. A neonate with a birth weight of 3765g was born. In this current pregnancy, she was referred once with first trimester bleeding. There were no other important events throughout this pregnancy.
Gestational age at time of induction was 40 weeks 3 days. Prostaglandins were used for priming of the cervix, followed by an artificial rupture of the membranes, and starting an intravenous drip of oxytocin. Epidural analgesia was used for pain relief in labor. Cervix reached full dilation after approximately 10 hours. She had an uneventful vaginal delivery after a short second stage of labor. A female neonate was born with a birth weight of 4060 g. Third stage of labor was uncomplicated. Estimated vaginal blood loss was 150 cc. Two hours after delivery, she suddenly became hypotensive and tachycardic, with diagnosis of a hypovolemic shock. Clinical examination showed an abdominal tenderness and bedside-ultrasound showed a large amount of free fluid intra-abdominally. There was no abnormal vaginal bleeding. An urgent CT abdomen was performed, showing a large amount of free fluid, reaching from the pelvic cavity up to the peri-splenic and peri-hepatic areas. Absence of contrast enhancement in the anterior uterine wall was compatible with possible uterine rupture. Furthermore, a contrast-extravasation on arterial phase was described on the posterolateral right side of the uterus, indicative for an arterial hemorrhage. There was no indication for embolization. An urgent laparotomy, using midline incision, was performed. Two grams of cefazoline, two units of packed cells and carboprost were given pre-operatively. A hemoperitoneum was diagnose perioperatively with 3000 cc of blood intra-abdominally. Primary focus of the bleeding was located on the posterior right side of the uterus, as a lateral branch of the uterine artery in the parametrium. Bleeding stopped after hemostatic sutures and clipping of the vessel. Uterus was intact with no signs of uterine rupture, in contrast to what was suggested on imaging. There was no visible abnormal anatomy of uterine vessels suggesting possible aneurysm. Since the sutures were placed in the anatomical proximity of the ureter, its course was thoroughly explored with no signs of ureteral injuries. A methylene blue test at cystoscopy was also performed, with normal results. At the end of the surgery, a surgical drain was inserted in the pelvic cavity that could be removed on day 4. Postoperative follow-up was without events. 1 unit of packed cells was administered, given the postoperative hemoglobin level of 7.2 g/dL. She was discharged ten days postpartum. A neurological examination one month postpartum showed a hypoesthesia of the right nervus cutaneus femoralis lateralis with preserved sensibility. Spontaneous recuperation is to be expected (Figure 1, Figure 2 and Figure 3).
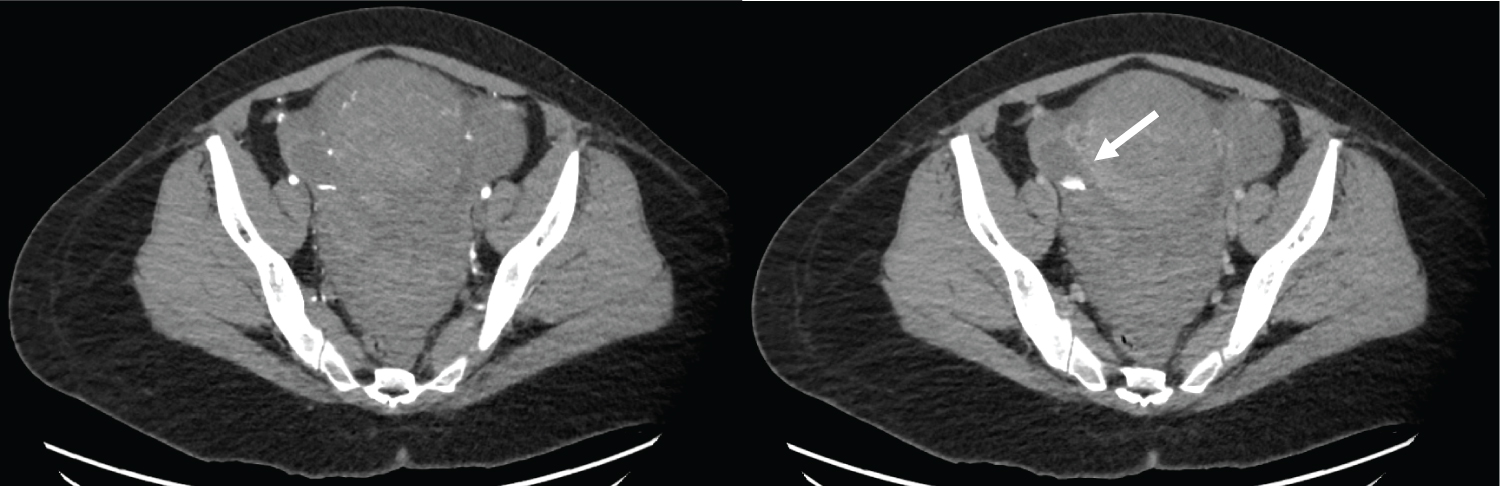 Figure 1: a) Axial early arterial phase; b) Portal venous phase images show contrast extravasation related to active bleeding in the right periuterine region (arrow).
View Figure 1
Figure 1: a) Axial early arterial phase; b) Portal venous phase images show contrast extravasation related to active bleeding in the right periuterine region (arrow).
View Figure 1
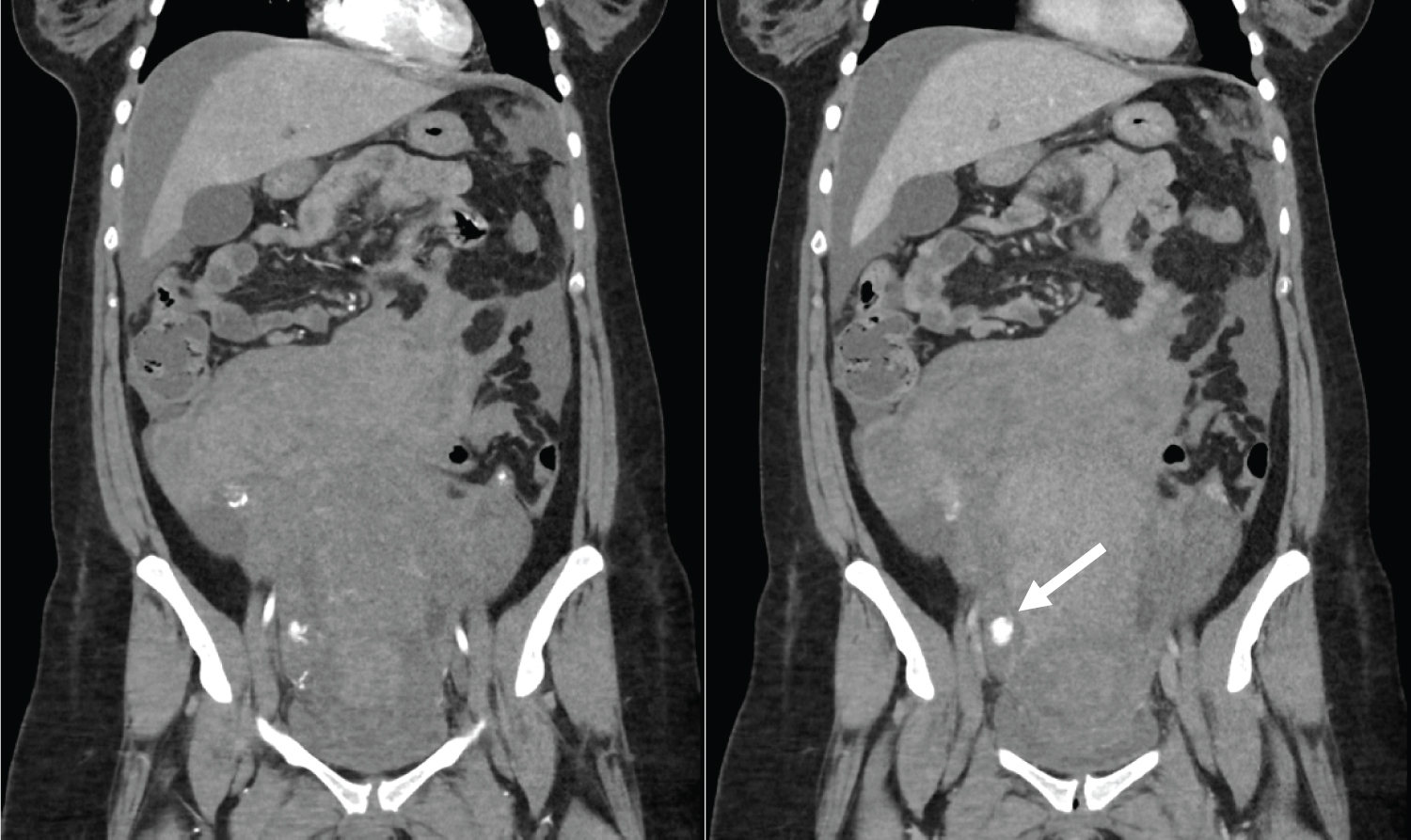 Figure 2: a) Coronal early arterial phase; b) Portal venous phase images show contrast extravasation related to active bleeding in the right periuterine region (arrow).
View Figure 2
Figure 2: a) Coronal early arterial phase; b) Portal venous phase images show contrast extravasation related to active bleeding in the right periuterine region (arrow).
View Figure 2
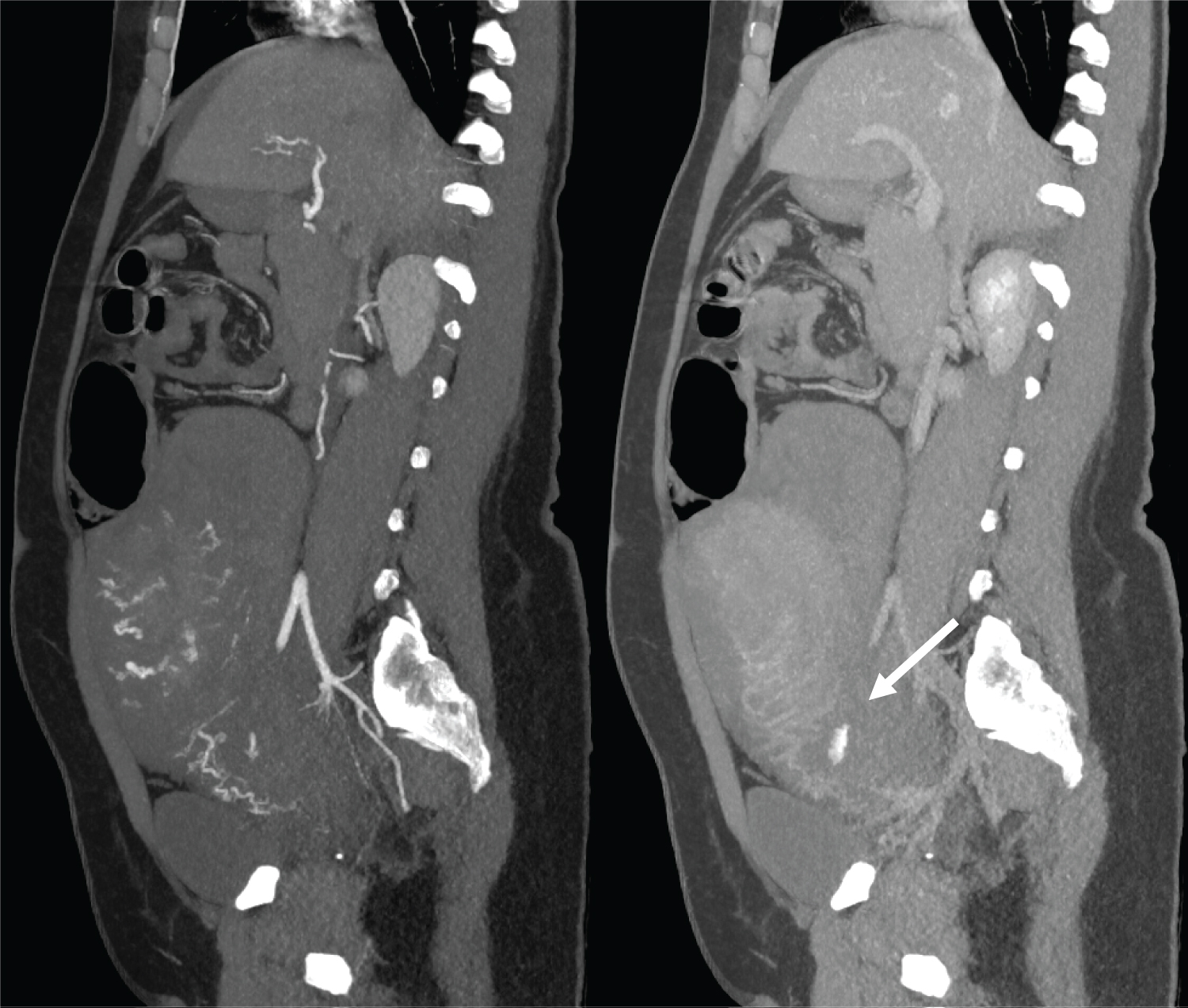 Figure 3: a) Sagittal maximum intensity projection (MIP) reformatted image shows the active bleeding in the right periuterine region as a small focus of contrast extravasation (arrow) in the arterial phase; b) Increasing in the venous phase.
View Figure 3
Figure 3: a) Sagittal maximum intensity projection (MIP) reformatted image shows the active bleeding in the right periuterine region as a small focus of contrast extravasation (arrow) in the arterial phase; b) Increasing in the venous phase.
View Figure 3
A spontaneous rupture of uterine vessels in the peripartum period is an uncommon but severe obstetrical complication. During pregnancy, uterine blood flow increases exponentially, to 450- 600 ml/min at term [1]. Rupture of these vessels can thus result in severe morbidity such as hypovolemic shock without significant external bleeding, need for surgical intervention, embolization, hysterectomy, but also possible maternal mortality [5,6]. Recent literature describes a maternal mortality of 1.7% [6].
The exact underlying pathophysiology of spontaneous utero-ovarian vessel rupture remains unknown, but is thought to be related to the hemodynamic, vascular, and hormonal changes associated with pregnancy. Another possible cause is the physiological atrophy of blood vessel walls in pregnancy, hence making them weaker and more fragile. Other contributing factors could include congenital arterial venous malformations, inflammatory processes, previous endometriosis surgery and chronic pelvic inflammatory disease [1,6-8].
Concerning the site of rupture, exact location may vary but the broad ligament is included in 75% of them, with the most reported locations being the utero-ovarian vessels and uterine arteries [9]. Moreover, most case reports describe the left uterine artery to be involved, in contrast to this patient in which the right side was affected. Factors linked to the increased frequency of rupture of the left uterine artery could be dextrorotation of the uterus, and an occipito-transverse/left occipito-anterior position of the fetal head, with the latter also being the case in this patient [8]. The most common presenting symptoms are acute abdominal pain, nausea, vomiting and syncope. Findings on clinical evaluation include hypovolemic shock without significant external bleeding, abdominal tenderness, and free fluid on ultrasound. [1,7]. Initial management includes stabilization using fluid resuscitation and transfusion of blood products, followed by prompt imaging if possible. Bedside ultrasound is frequently used as a first-line imaging modality to detect free fluid intra-abdominally but is not useful in locating the exact source of bleeding. Computed tomography (CT) is readily available in most emergency departments. If the patient is hemodynamically stable this is the imaging method of choice to locate the origin of the acute bleeding [1]. When an intraperitoneal hemorrhage is confirmed, an urgent exploratory laparotomy should be performed. Evacuation of hematoma with ligation of the bleeding vessels, selective arterial embolization or hysterectomy are suitable treatment options, depending on the peri-operative findings [7].
We would like to point out that on CT imaging there was a strong suspicion of a uterine rupture in combination with a vessel rupture, which is one of the reasons why embolization was declined. However, peri-operatively there were no arguments for a uterine rupture with an intact unscarred uterus. We could not find a reasonable and straightforward explanation. It could be linked to early postpartum changes in comparison to a nongravid uterus, such as contraction of the lower segment of the uterus, blood and fluid in the endometrial cavity or perfusion changes on the former placental site mimicking a uterine wall rupture.
This case is a unique presentation of a spontaneous uterine artery rupture of an unscarred uterus in the peripartum period. Although rare, it should be considered as of one of the differential diagnoses of postpartum collapse. The exact pathophysiology remains unknown but is linked to hormonal, vascular and hemodynamic changes in pregnancy. Other risk factors include endometriosis surgery, congenital AV-malformations, or inflammatory processes. Clinical symptoms are abdominal pain, abdominal tenderness, nausea and vomiting, possible hypovolemic shock, and absence of vaginal bleeding. Computed tomography (CT) is useful as a diagnostic tool to locate the bleeding, if patient is hemodynamically stable. Management is usually surgical.
Regarding possible future pregnancies, there is very limited information to counsel patients. The recurrence risk of vessel rupture is unclear. Thus, counseling should be indivualized.
The patient whose story is reviewed in this case report has provided her consent for its publication.