Different lumbar traction techniques are widely used for non-specific low back pain (NSLBP) however, which one is more effective is not yet ascertained.
The study was designed to examine the effect of manual lumbar traction (MLT) and prone traction (MPT) on pain intensity (PI), disability (Dis), range of motion (ROM) and health related quality of life (HRQoL) of patients with NSLBP.
Fifty-four consenting patients with NSLBP were purposely recruited and were randomized to MLT and MPT group equally. Subjects in MLT and MPT received manual lumbar traction and prone traction respectively, 10 minutes, twice weekly for six weeks, while PI, Dis ROM and HRQoL were examined at baseline, 2nd, 4th, and 6th weeks of treatment. Data was analysed using descriptive and inferential statistics. Alpha level was ≤ 0.05.
MLT and MPT had significant reduction on PI, Dis, ROM and HRQoL at P = 0.000 when baseline, 2nd, 4th and 6th week were compared. There were significant reduction (P = 0.001) when MLT and MPT groups’ PI Dis, ROM and HRQoL at 2nd, 4th and 6th week were compared.
MLT and MPT were effective in the management of NSLBP with MPT having higher reduction in PI, Dis, ROM and MLT having greater impact on HRQoL.
Clinical Trials.gov Identifier Number: NCT05518552
Manual lumbar traction, Prone traction, Pain intensity, Low back pain, Disability
Non-specific LBP is tension, soreness and/or stiffness in the lower back region for which is not possible to identify a specific cause of the pain but several structures in the back, including joints, discs and connective tissues, may contribute to symptoms [1]. The diagnosis of non-specific LBP is dependent on the clinician being satisfied that there is not a specific cause for their patient’s pain. LBP is regarded as a symptom from impairments in the structure of the low back which includes muscles, ligament and intervertebral disc [1]. Low back pain is a symptoms of myriad of causes which can be primary i.e. mechanical/nonspecific and also secondary with an underlying pathology i.e. non mechanical causes which occur in the rest of the population [2,3]. Non-specific low back pain appears to be commoner, affecting mostly individuals between ages 30 and 50 years [4]. However, in children and adolescents it appears to be usually secondary to an underlying pathology [5].
Physiotherapy is central to the overall management of LBP in the sub-acute and chronic phases [5]. In clinical setting, manual treatment (e.g. stretching, traction, mobilization and manipulation) and patients’ educational training are often used in combination, to give the patient pain relief and better function [6]. The use of traction in the management of patients with acute or chronic low back pain (LBP) has generally not been endorsed by evidence-based practice guidelines [6]. Alrwaily in the result of the systematic review submitted that though there was heterogeneity in the methods of traction to the low back among the randomized control study being reviewed, they concluded that the negative results on the outcome measures should be interpreted with caution [7]. Another study reported that lack of support is based on the results of randomized clinical trials that have examined heterogeneous samples of patients with LBP and failed to find any benefit for traction when compared with sham, placebo, or other treatments [8]. Evidence supports the contention that the power of clinical research can be enhanced when more homogeneous subgroups of subjects are studied, but most research on traction has not taken this into account [9].
Various forms of lumbar traction have been used for the relief of pain since the time of Hippocrates. During the 1950’s and 1960’s it became popular, and until today it is used by physiotherapists for treating patients with low back pain [10]. Although it effectiveness is still being questioned by a few clinical trials. However, because high-quality studies within the field are scarce, many are underpowered, and traction is often supplied in combination with other treatment modalities. Available literature does not support a firm conclusion that traction is not an effective treatment for patients with LBP [11]. There are three benefits of lumbar traction: distraction to increase the intervertebral space, stretching of the posterior longitudinal vertebral ligament and suction to draw the disc protrusion towards the centre of the intervertebral disc [12]. Different types of lumbar traction have been described such as mechanical traction, auto traction, manual traction, continuous traction, sustained traction, intermittent traction, gravitational traction [13].
Although traction is widely used for lumbar spine disease, a study reported lack of consensus about lumbar traction efficacy and application method [14]. In a study conducted by Krause, et al., in the United States, they found out that most of the Orthopaedic Physical Therapists in the United States use lumbar traction, though not necessarily consistent with proposed criteria that identify patients most likely to benefit from traction usage [14]. Clinicians use a variety of lumbar traction approaches (or spinal decompression approaches) equally, there was no generally accepted traction protocol available [15]. When identifying a traction protocol for the individual patient, clinicians need to consider various factors, including patient positioning, ease of application, availability of traction equipment and its efficacy.
Nevertheless, more studies have been conducted on various modes of traction techniques but little or no information exists on the utilization of manual lumbar traction and prone lumbar traction techniques. Therefore, due to the paucity of such literature, this study was conceived to investigate the effects of these two techniques and their comparison in this study on patients suffering from NSLBP. Considering the flaws of some researches about the homogeneity of the protocols; manual lumbar traction considered in this study was in prone position, the prone traction as well was in prone position, no mechanical application of pulling but majorly manual to produce traction force. The researchers were trying to have homogeneity of protocols as much as possible to address some of the flaws in the previous researches. Again, based on the financial plight facing the facility where the study was conducted which has affected some of the equipment especially traction machine, it is highly needed to consider other means of traction for the patients with NSLBP which will not involve either machine or electricity. In order to assess the effectiveness of these two protocols and to ascertain which one could render better result, the study was therefore conceived and executed.
Subjects for the study were recruited from the patients with Non-specific Low- Back Pain (NSLBP) coming for treatment at the Outpatient Physiotherapy Clinic of the Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Osun State, Nigeria.
The following categories of subjects were recruited for the study:
Patients diagnosed with Non-Specific LBP of not less than 3 months’ duration.
The minimum age to enter the study was 40 years.
1. Patients with low back pain with specific pathology, such as systemic inflammatory diseases, pregnancy, fractures of the spine, tumours, infections.
2. Patients with pathology affecting the trunk or upper and lower extremities.
A purposive sampling technique was used to recruit subjects for the study. But they were allocated to the groups randomly.
The sample size for the study was determined using the formula.
n = 2 (Ζα∕2+ Ζ1-β) 2 /(µ 1 -µ 2/ σ ) 2 [16].
where Ζα∕2 - represents the critical value of the normal distribution at α∕2. (i.e. for a confidence level of 95%, α is 0.05 and the critical value is 1,96), Ζ1-β represents the critical value of the normal distribution at 1- β (i.e. for a power of 80%, β is 0.2 and the critical value is 0.84), µ 1 and µ 2 are means from 2 independent groups. δ is the effect size which is the standardised difference and equal to the absolute difference (Δ) divided by standard deviation (σ). Thus, n (size per group) = 25 [16].
Subjects were randomly allocated to the two groups using fish bow method. This was conducted by one of the authors. Once a patient was assessed and found qualify for the study, two wrapped paper were presented for the patient to pick one. On each of the paper was inscribed: Manual or prone traction. Each patient is now allocated to the label picked until the desired number was satisfied. The flow chart and the consort were shown in Figure 1.
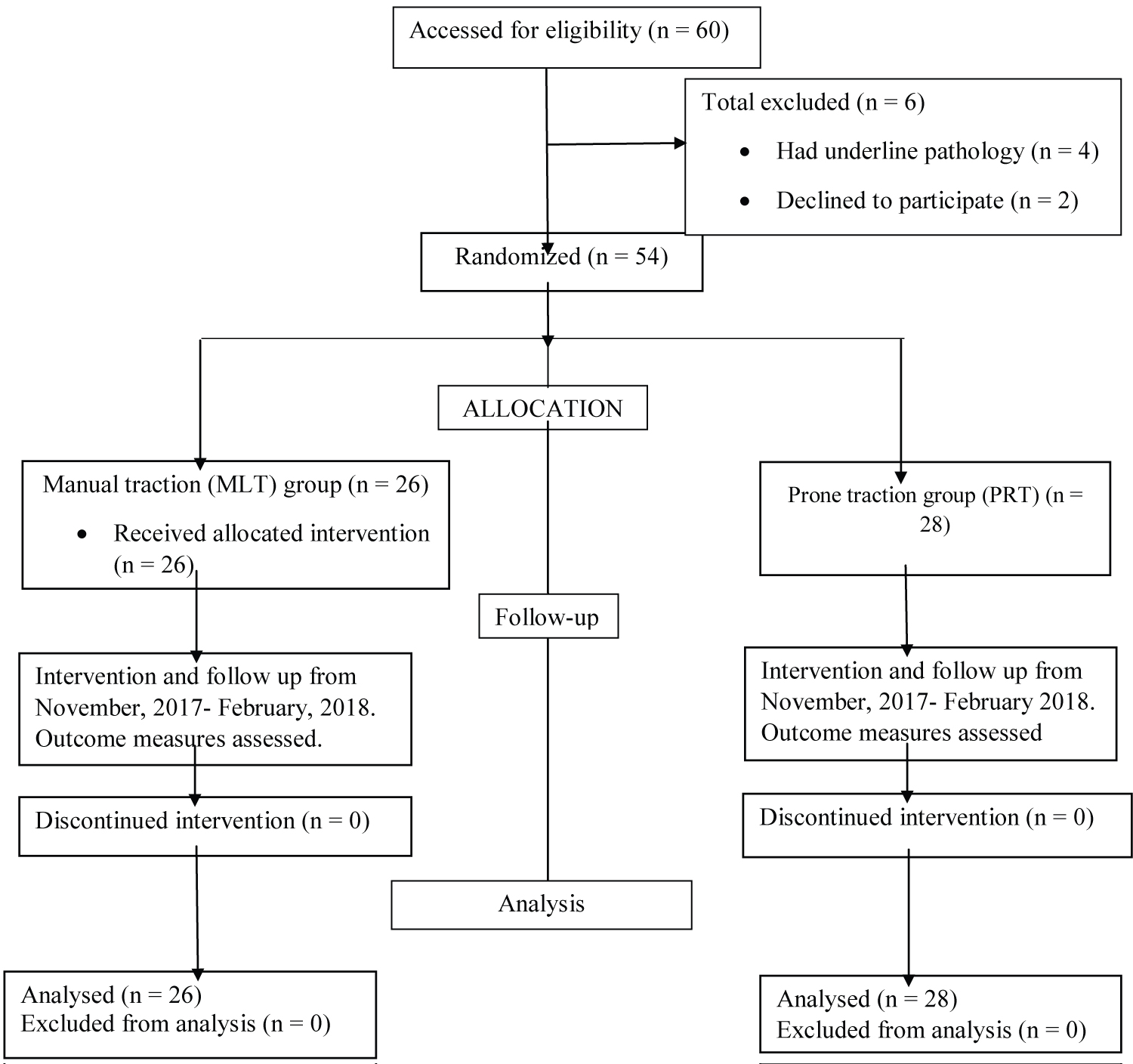 Figure 1: Randomization. Consult diagram of random allocation of participant into 2 groups.
View Figure 1
Figure 1: Randomization. Consult diagram of random allocation of participant into 2 groups.
View Figure 1
The research design was pre and post-test randomized control study.
The following instruments were used in this study.
i. Visual analogue scale: The visual analogue scale was validated with Verbal Rating Scale by Price, et al. [17], they arrived at the point that Verbal Rating Scale provide useful alternative to the visual analogue scale scores in the assessment of chronic pain. Visual analogue was used to measure present pain in the study. Patient placed a check mark next to the phrase that best describes the current intensity of their pain. A response of “No Pain: Is given a value of Zero and 10 worst possible pain.
Roland Morris low back pain Disability questionnaire: (RLMDQ) This 24-item questionnaire was developed by Roland and Morris [18]. The scoring entails totalling the sum of circled items (maximum is 24), thus representing the final score. According to Von Korff and Saunders, a RMLDQ cut off score of > 14 represents significant disability associated with an unfavourable outcome [19]. It is referred to as the best single study to assess the short-term outcome of primary care in patients with LBP.
SF-12 (version 2) was used to measure the quality of life. The SF-12 Health Survey (SF-12). It is a 12-item questionnaire used to assess generic health outcomes from the patient’s perspective [20]. Generic patient-reported outcome measures like the SF-12 assess general health and well-being [or health-related quality of life (HRQOL)], including the impact of any and all illnesses on a broad range of functional domains. The SF-12 consists of a subset of 12 items from the SF-36 Health Survey (SF-36) [21]. Ware, et al. covering the same eight domains of health outcomes, including physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health [21]. SF-12 scales and summary measures are scored so that a higher score indicates a better health state. The reliability and validity of the SF-12 and SF-12 has been evaluated and is summarized in user manuals [22].
Ethical approval for the study was obtained from the Health Research and Ethics Committee of the Institute of Public Health Obafemi Awolowo University, Ile-Ife before the commencement of the study (IPHOAU/12/976). The nature and purpose of the study was explained to the subjects and informed consent was obtained from each subject.
Each subject’s back pain status and eligibility for the study was checked at the point of recruitment into the study by medical history, interview and clinical/physical examination using the following tests according to Konin, et al. [23].; Ely’s test, Lasegue’s test, forward flexion, back extension, side rotation, and digital pressure along the spine. The criteria for participation are the eliciting of pain in at least two of the tests. Radiographs of such patient were examined to rule out red flag signs like Pott’s disease, osteoporosis and other infection.
At the beginning of the treatment the weight, height, waist and hip circumferences of each participant were measured and recorded. The initial pain intensity was assessed using Visual Analogue scale. Rolland Morris Disability Questionnaire and SF-12 were administered to the participants to fill as the baseline in order to assess the level of disability and HRQoL. Spinal ROM was measured with inclinometer.
Manual traction: Manual traction was administered with the patient lying prone on a couch using a manual technique by pulling from the ankles of the patient. Manual traction was performed by the one of the authors by pulling at the patient’s ankles [12]. The patient was fitted with counter action harness at the chest to the couch. Straight and steady pull was performed from the ankle joints until noticeable distraction was felt by the patient at the lumbar region. The pull was sustained for 5 minutes seconds a resting period of another 3 minutes with 4 repetitions. The procedure was carried out twice weekly for six weeks Figure 2.
 Figure 2: A patient on manual lumbar traction.
View Figure 2
Figure 2: A patient on manual lumbar traction.
View Figure 2
Prone traction was administered as described by Dawodu [24]. Prone traction kit (three pillows arranged on each other) was used to support the patient at the level of the umbilicus while the patient lies prone transversely on a couch. The two lower limbs were on one side on the couch, the umbilicus was on the traction kit. The trunk and the two upper limbs were on the other side of the couch hanging. The researcher crossed his two hands in the opposite direction pressing the posterior dimples and the level of the first lumbar vertebral. Each subject maintained the prone position for 5 minutes and the procedure was repeated 4 times per session, two times a week for six weeks Figure 3.
 Figure 3: A patient on prone traction.
View Figure 3
Figure 3: A patient on prone traction.
View Figure 3
Outcome measures: Visual analogue scale: This was used to measure subject’s present pain intensity (i.e. pain at the time of study), at the beginning, 2 nd , 4 th and 6 th weeks of the treatment sessions.
i. The Roland-Morris Low back pain Disability Questionnaire (RMLDQ): This was used to assess the disability of the patient. This was measured at the beginning, 2 nd , 4 th , and 6 th weeks of the treatment sessions.
ii. Spinal ROM (forward flexion and extension): Inclinometer was used to measure the spinal ROM. These were measured at the beginning, 2 nd , 4 th , and 6 th weeks of the treatment.
iii. Health Related Quality of life (HRQoL): This was measured using SF12, it is usually self-administered by completing the questionnaire in the clinic. This was measured at the beginning, 2 nd , 4 th , and 6 th weeks of the treatment.
Data was analysed using Statistics Package for Social Science (SPSS version 23). The analysis was summarized using descriptive and inferential statistics. Independent t test was used to compare the physical characteristics of the two groups. Two-way ANOVA was used to compare the means of pain intensity, disability, ROM and quality of life between the two groups. Repeated measure ANOVA was used to compare the mean values of the pain intensity, disability, ROM and quality of life of all the subjects within the group. Post hoc analysis was carried out where necessary. Alpha level was set at 0.05.
Table 1 presents the sex distribution of subjects in MLT and MPT groups. There were 12 females and 14 males that participated in MLT group and there were 14 each of females and males in the MPT group.
Table 1: Summary of sex distribution of all subjects (N = 54). View Table 1
Presented in Table 2 are the mean anthropometric characteristics of the subjects in both groups. The mean age, BMI and WHR for MLT group were 59 ± 10.5 yrs, 27.31 ± 2.47 kg/m 2 and 0.93 ± 0.07 respectively while 59.9 ± 8.74 yrs, 27.15 ± 10.34 kg/m 2 and 0.96 ± 0.09 were the respective mean age, BMI and WHR in the MPT group. There was no significant difference (P > 0.05) when the two groups were compared.
Table 2: Physical characteristics of the subjects in MLT and MPT groups (N = 54). View Table 2
Table 3: Effects of MLT on PI, Dis, Fl, Ex and HQoL of MLT group. n= 28. View Table 3
Table 4: Summary of repeated measure ANOVA and Post hoc comparison the pre-treatment 2nd, 4th and 6th week treatment of PI, Dis, Fl, Ex and QoL in MPT group n=28. View Table 4
Table 5: Shows comparison between effects of MLT and PRpre-treatment, 2nd, 4th and 6th week treatment of PI, Dis, Fl, Ex and HRQoL of MLT and MPT Group (N = 54). View Table 5
Table 3 presents the summary of repeated ANOVA with Post hoc comparing the difference between mean values of the of outcome measures of pre-treatment and each of 2 nd , 4 th , and 6 th week; the difference between the 2 nd week and each of 4 th , and 6 th week and the difference between 4 th and 6 th week treatment session of participants in MLT group. The results revealed that there was a significance difference in effects on pain intensity, (PI) (F = 49.369; p ˂ 0.001), Disability (Dis) (F = 29.998; p ˂ 0.001), flexion (FROM) (F = 16.825; p < 0.001), extension (EROM) (F = 36.527; p < 0.001) and health related quality of life (HRQoL) (F = 26.333; p ˂ 0.001). The peak of pain reduction, disability and increment in other outcome measures were observed between the pretreatment and the 6 th week intervention (Pnd3, Did 3, FROMD3, EROMd3, HQoL3).
The results in Table 4 showed the repeated measure of ANOVA, comparing the difference in mean values of pretreatment and each of week 2, 4 and 6 of the intervention of prone traction on PI, Dis, FROM, EROM and HRQoL The results revealed that there was a significance reduction in PI (F = 30.589; p < 0.001) and Dis (F = 19.770; p < 0.001), improvement in FROM (F = 13.786; p ˂ 0.001), EROM (F = 19.787 p < 0.001) and HRQoL (F = 17.432; p ˂ 0.001). The peak of pain reduction, disability and increment in other outcome measures were observed between the pretreatment and the 6 th week intervention (Pnd3, Did 3, FROMD3, EROMd3, HQoL3).
The results in Table 5 showed the two-way ANOVA comparing the effects of manual traction and prone traction on PI, Dis, Fl, Ex and HRQoL of the pre-treatment, 2 nd , 4 th and 6 th . It was revealed that there was no significance difference in the effects between 2 nd week and pretretment values in all the outcome measures but subsequently Manual Prone traction proved to improve all the outcomes measures better compared to Manual Lumbar traction (PI F = 37.298; p ˂ 0.001), Dis (F = 21.529; p ˂ 0.001), Fl (15.122; p < 0.001), Ex (23.602; p < 0.001) and HRQoL (17.882; p < 0.001). More importantly the peak difference was observed between the pre-treatment and the 6 th week mean values in all the outcome measure.
It was observed from this study that the baseline values of clinical variables: Pain intensity, disability, range of motion, quality of life and the physical characteristics of the participants in the two groups were not significantly different from each other. This was an indication that the subjects in the two groups were comparable, therefore the changes observed in the study was due to the intervention.
In managing LBP, the importance of natural history of LBP should be borne in mind when considering the efficacy or effect of any intervention instituted. Natural remission of acute episode of LBP over a period of time was recognised while recurrence of LBP was a common feature in patients with chronic LBP [25]. Therefore, the possibility of acute LBP coexisting with chronic LBP (acute or chronic) improving with time could not be overruled [26]. However, since none of the subjects in the two groups received any other treatment for LBP from other health care personnel during the study, the greater improvement in the clinical variables as obtained in the two groups could be attributed to LBP treatments instituted and implemented in the present study [25].
In this study, there was a significant reduction between the pre-treatment, 2 nd , 4 th and 6 th post-treatment pain intensity in manual traction group. Manual traction was found to produce significant reduction in pain intensity; this was in accordance with the work of Ljunggren, et al. who found out that manual lumbar traction was efficient in relieving pain of lumbar origin [27]. Pain intensity was significantly reduced with simple manual lumbar traction according to Ljunggren, et al., and they recommended simple manual lumbar traction variety be preferred for patients with lumbar intervertebral disc prolapse [27]. Their study involved patients with lumbago-sciatica and prolapsed lumbar intervertebral disc with the usage of manual traction and auto traction; the usage of manual traction was in tandem with our study. Their study concluded that one fourth of patients treated with manual lumbar traction avoided operation after using manual lumbar traction and there was no recurrence of symptoms after two years [27]. The reduction in pain intensity could be adduced to the mechanical separation of vertebrae, decreased intradiscal pressure leading to reorganisation of discal materials in annulus pulposus and stimulation of mechanoreceptors causing non-nociceptors release as suggested by Peláez and Taniguchi [28]. Pain reduction could also be achieved due to distraction to increase the intervertebral space, stretching of the posterior longitudinal vertebral ligament and suction to draw the disc protrusion towards the centre of the inter vertebra disc [12]. There was also significant decrease in disability in this study after the intervention using the manual lumbar traction. Ones the pain reduces, disability is expected to improve.
This study observed a reduction between pre-treatment, 2 nd , 4 th and 6 th week of pain intensity of patients who underwent prone traction, this was in accordance with the study carried out by Ojoawo, et al. to determine the effect of prone traction on non-specific low back pain where there was a significant reduction in pain intensity and reduction of disabilities of patients with low back pain [29]. Ojoawo, et al.’s work did not compare their study but the aspect of prone traction was similar with the present study [29]. Gravitational traction has being observed to increase intervertebral space and was found to be an effective method to distract lumbar vertebrae [30]. Distraction was more than approximately 3 mm in each intervertebral space in both groups with low back pain and without low back pain [30]. In the review carried out by Cavagnaro, et al. they detected a study concerning inversion therapy [31]. It was a prospective randomized controlled trial in which twenty-four patients awaiting surgery for pure lumbar discogenic disease were allocated to either physiotherapy or physiotherapy and intermittent traction with an inversion device. Authors concluded that the association of inversion traction and physiotherapy resulted in a significant reduction of the patient’s complaint. Though our study did not consider patients with discogenic pain but low back pain from spondylosis, however the results have a similar presentation.
A significant reduction in pain intensity was also observed in both MLT and MPT groups. This was in accordance with the work of Tekeoglu, et al. [30], who reported that traction mechanism to relieve pain seems to separate the vertebrae, remove pressure or contact forces from injured tissue, increase peripheral circulation by a massage effect, and reduce muscle spasm. However, prone traction relieves pain, reduces disability, and increases range of motion more than manual traction across the week. The application of prone traction involves pulling of the body segment upside down where the lower limbs pull the lower part of the body on one side and the trunk pulls it on the other side instituting a separation on the lumbar region. The pillows as well push the lumber region up to enhance the distraction and separation at the lumber region. All these were not the features of manual traction. These may be accounted for a better improvement on prone traction over the manual traction. The cultural differences in pain expression can be a factor influencing the feeling of pain among the participants. There is a cultural uniqueness language of pain and the way it is being expressed which will notify the relatives and other people around. The cultural differences are determined by the emotion, postural mobility and verbal expression in response to pain, injury or disease [32]. The subjects in this study belong to a culture that expresses the feeling of pain both emotionally and verbally. If there is pain or discomfort, such an individual will display a change of action or attitudes, sadness and depression are common feature to be noted. Therefore, it gives the researcher an easier way of assessing the pain intensity.
Coluccia, et al. [33] submitted that chronic low back pain is a disabling disease which restricts quality of life; they observed a strong association between disability and the physical quality of life domain. This was an indication that disability negatively affects and strongly influences physical quality of life in patients with chronic low back pain. The influence of pain and disability on quality of life progresses whiles the pain last, indicating that as pain reduces, disability and quality of life improves, which was observed in this study, back pain is one of the complaints that has negative effect on various aspect of life [34]. Panahi, et al. studied 200 students to assess the aspects of life quality and its relationship with disability due to low back pain among students, the study indicated low back pain could affect not only on students' physical aspects of quality of life but also psychological and social aspects of quality of life could decrease [35]. The health related quality of life questionnaire used may have some cultural inclination in the way the subjects responded to the questions. However, the effect of culture may not be too important here based on the fact that the subjects in the two groups were assessed using the same questionnaire.
The results from this study showed that prone lumbar traction yielded more significant improvement than manual traction on pain intensity, disability and range of motion in both flexion and extension. However, manual traction resulted in more significant improvement in the quality of life. One of the mostly accepted mechanism traction produces therapeutic effect is via the separating force produced in the spine. This may account for how prone traction produces more significant improvement because the gravitational force combined with body weight is an added advantage to produce more traction force at the lumbar region. Distraction of lumbar vertebrae and subsequent widening of disc space reflect a stretching of anterior and posterior vertebral ligaments. This resulted into better lumbar flexibility and consequently increases in range of motion. While manual traction requires the effort of the therapist which may be tiring and unsustainable enough to achieve the desired tractive force, prone traction uses the body weight and gravitational force for its action.
Tekeoglu, et al. also reported significant widening of intervertebral disc space with gravitational traction by lateral lumbrosacral radiographs [30]. Prasad, et al. reported similar results about inverted traction therapy with which the results from this study were consistent [36]. However, patients with low back pain are more mentally distressed. Self-reported symptoms of somatisation, anxiety, phobic anxiety, obsessive-compulsive disorder, hostility, and depression are all common among patients with LBP, compared to the general population [37]. All these result to poor quality of life among patients with low back pain. Though both tractions were applied in prone position, the simplicity and less cumbersome of manual traction over the gravitational assisted position in the prone lumbar traction may account for the psychological benefits of manual traction on the aforementioned self-reported symptoms and thereby yielding better improved quality of life following the therapy sessions. It was observed generally in the study that the maximum effects considering all outcomes measures and in the two groups was at the difference between the pretreatment and the 6 th week of the intervention. This inferred that the maximum result could be obtained from the patient after 6 week of treating a patient with non specific low back pain using prone or mechanical traction for 6 weeks.
It can be concluded from the study that MLT and MPT might be effective in the management of NSLBP with MPT causing higher reduction compare with MLT in PI, Dis, ROM and but MLT having greater impact on HRQoL than MPT. The two techniques have comparative effects on pain intensity, disability, lumbar range of motion and quality of life in patients with non-specific low back pain.
There are some limitations to the study. One of them is that there was no control group in which no treatment was given to such patients. Again, there were no other groups with a different intervention for comparison. In addition, the study did not capture the result of the outcomes beyond 6 weeks to know how sustained the effects were.
Adesola Ojo Ojoawo: Conceived the ideas did the data analysis, interpreted the data and did the final write up; Olusesan Olufemi Adedeji: Collected the data, search for literature, did the skeletal write up; Kayode Kunuji: Assisted in the data collections, supply the literature, contributed in the skeletal write up; Taofik Olusegun Afolabi: Assisted in the data collection, assisted in the data analysis and partake in the critical writing of the final manuscript.
None.