Spinal deformities are referred to Scoliosis and Kyphosis-Lordosis following human race from birth, under the phenomenon of congenital anomalies, later as adolescent spinal deformities, till the last period of human life under the term of aging Spine.
This paper presents the measuring protocol and the measurements’ reliability obtained in normal subjects, using a recently developed, real-time spine monitoring system, called "SPIMON".
For the purpose of this study a group of 40 healthy volunteers (26 male and 14 female), were finally selected out of 50 healthy volunteers initially examined. The results are presented regarding the Thoracic Forward Flexion and Thoracic Backward Flexion (Extension), the Lumbar Forward Flexion and Lumbar Backward Flexion (Extension), the Thoracic Spine Bending Tests and the Lumbar Spine Bending Tests. The results are compared to physiological values, as published in the literature and were found within the normal limits, while at the same time "SPIMON" introduces a series of advantages including: Real-time monitoring and observing of the Spine, Relatively simple and easy donning on and off and a non-radiation and non-invasive system. Disadvantages of the proposed system may be a Low accuracy in obese patients and User dependent results.
The term “Spinal Deformity” embraces to two major kinds of deformities: The Scoliosis and the Kyphosis-Lordosis. Scoliosis is the spinal deformity referred to as the Coronal plane of the spine, while Kyphosis-Lordosis is referred to as the Sagittal plane. In most cases, Kyphosis and Scoliosis co-exist and the term Kypho-Scoliosis is also used. Based on the US Census Bureau and using current prevalence estimates, there are approximately 27.5 million elderly people with some form of spinal deformity, with the high rate of growth that brings this number to more than 60 million by 2050, in US only [1]. Adolescent idiopathic scoliosis is present in 2 to 4 percent of children between 10 and 16 years of age [2].
The Golden Standard for measuring spinal deformities remains the X-ray radiography, with the drawback of radiation exposure, especially when it comes to pediatric patients [3]. For this reason, new technologies have been developed to measure spinal deformities without the use of ionizing radiation, like the Spinal mouse, the Scolioscan and the Diers 4D motion Lab [4-7]. Spinal mouse is a non-invasive, external device, manually guided over the skin of the back along the spinal column, over the lumbar and thoracic spine, measuring mostly kyphosis and lordosis angles [4]. Although Spinal mouse may depict information regarding the movement of the Spine in the sagittal plane (Kyphosis and Lordosis), it is not used for Scoliosis curvatures (coronal plane) live movements. Scolioscan is an Ultrasound (U/S) imaging system used for Scoliosis [5] that depicts live movement information of a small part of the spine, because the use of the U/S probe needed, sufficiently limits the overall view of the spine. The Diers 4D motion Lab offers the capability of live observation of the whole spine in both coronal and sagittal planes but the equipment used reaches the magnitude of a whole laboratory and therefore it does not meet the capabilities or infrastructure capacity of a normal medical office, as well as the needs of a population-screening program [6,7]. More recently, an inertial measurement unit (IMU) based wireless wearable system has been proposed, allowing real-time three-dimensional measurement of spinal deformities, in a non-invasive manner [8].
This paper presents the measuring protocol and the measurements reliability obtained in normal subjects, using the recently developed afore mentioned spine monitoring system, now called “SPIMON”. The results are compared to physiological values, as published in the literature.
The SPIMON system is comprised of one wireless main unit and 26 wired along sensor nodes, to form a lightweight wearable sensor stripe for superficial attachment over the human spine. The node’s size and arrangement are optimized so that each node approximately tracks one individual vertebra. Each sensor node incorporates a six degrees of freedom IMU, where its embedded gyroscope and accelerometer data are periodically sampled by the main unit with a rate of 4 Hz, in succession from bottom to top. The central processing unit (CPU) then calculates the Pitch and Roll Euler angles of each sensor node, based on the acquired filtered raw IMU readings. The calculated angles are streamed in real-time through Bluetooth connection to a paired smartphone running an in-house developed dedicated Android application that manages the digital signal processing and includes algorithms for calculation of the 3D positions of each sensor node along with detection and calculation of the kyphotic, lordotic, and scoliosis angles. The Application features an interactive graphical user interface (GUI) that allows for real-time animated visualization and monitoring of the spinal cord motion in the 3D space. The spine is modeled as a flexible structure, with 26 segments, allowing dynamic three-dimensional motion.
The subject is initially, physically examined, from the physician specialist (spine surgeon), according to the following protocol. The subject is standing up, with the lower limbs in contact and the knees in full extension. The Physician is standing on the back of the subject. First, the shoulders are checked for possible shoulder imbalance and then the pelvis is checked for possible pelvic obliquity (Figure 1).
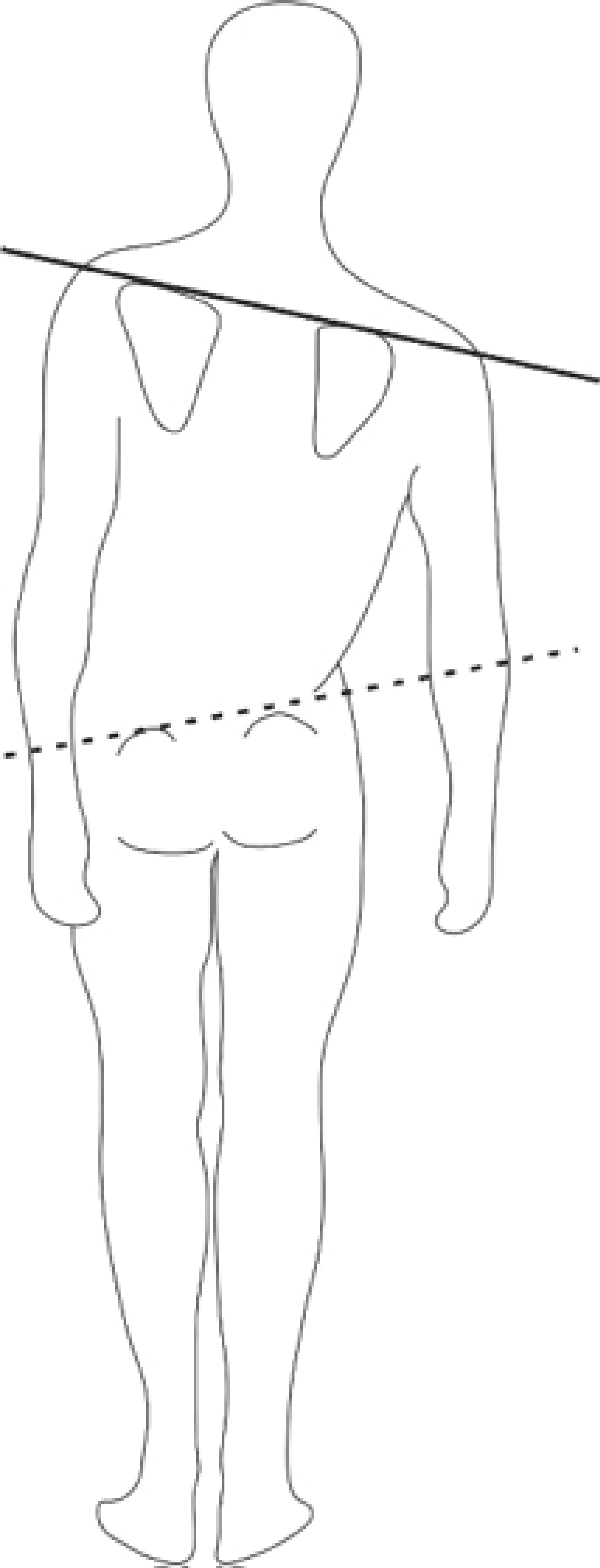 Figure 1: Inspection for shoulder imbalance and pelvic obliquity.
View Figure 1
Figure 1: Inspection for shoulder imbalance and pelvic obliquity.
View Figure 1
Then the Adam's forward bending test for scoliosis screening is used. The subject stands and bends forward at the waist. The examiner assesses for back symmetry from behind and beside the patient. Any back or rib cage abnormalities, such as a rib hump (Figure 2 arrow), may be a sign of scoliosis [9].
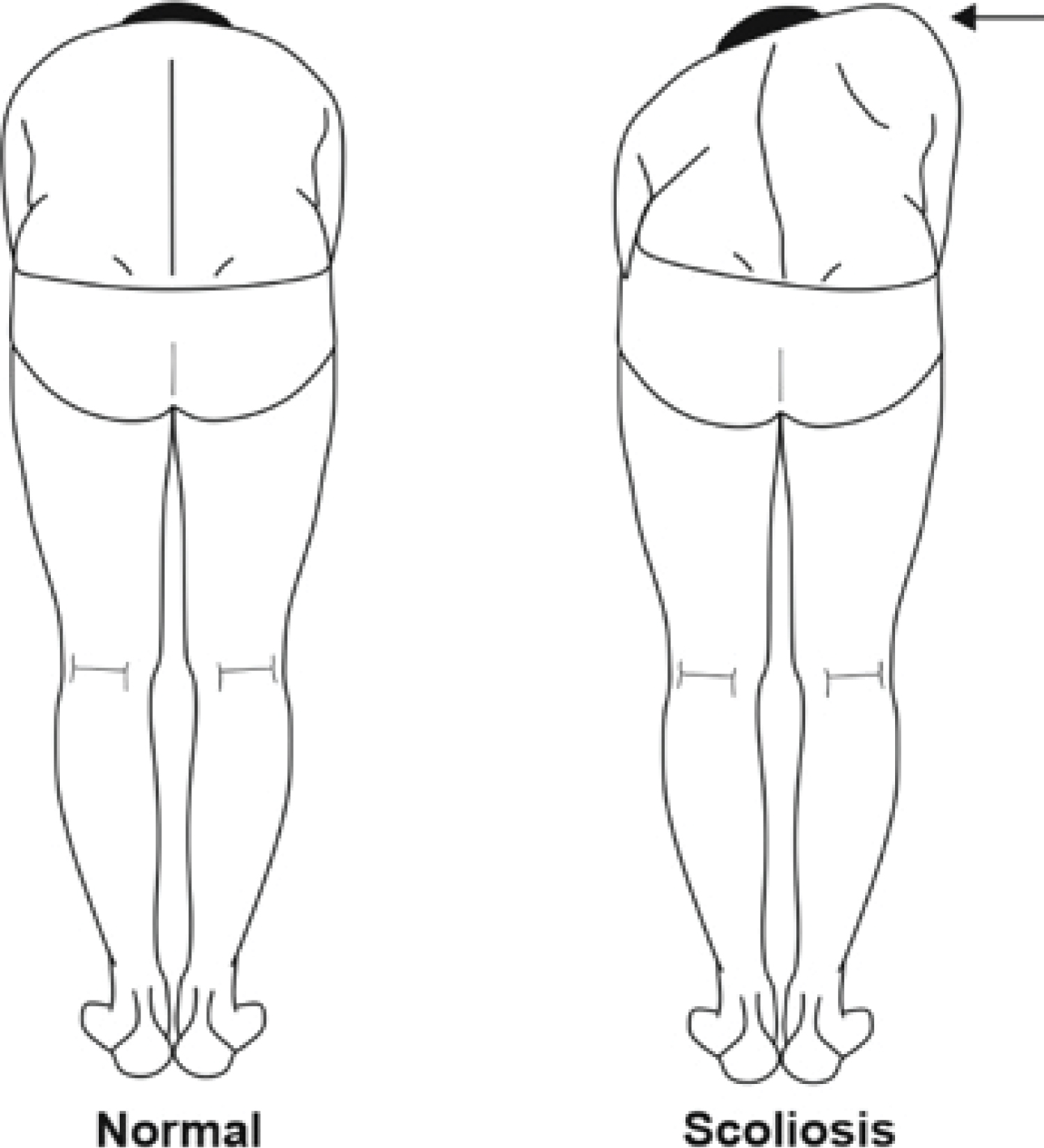 Figure 2: The Adam’s bending test.
View Figure 2
Figure 2: The Adam’s bending test.
View Figure 2
Normal Spine and Scoliosis comparisonThen the physician palpates and marks each vertebra spinal process of the subject’s spine and applies the sensor nodes upon each vertebra process as it is shown in Figure 3. The system offers real-time measurements together with 2D Views in the Coronal and Sagittal Plane, as illustrated in Figure 3.
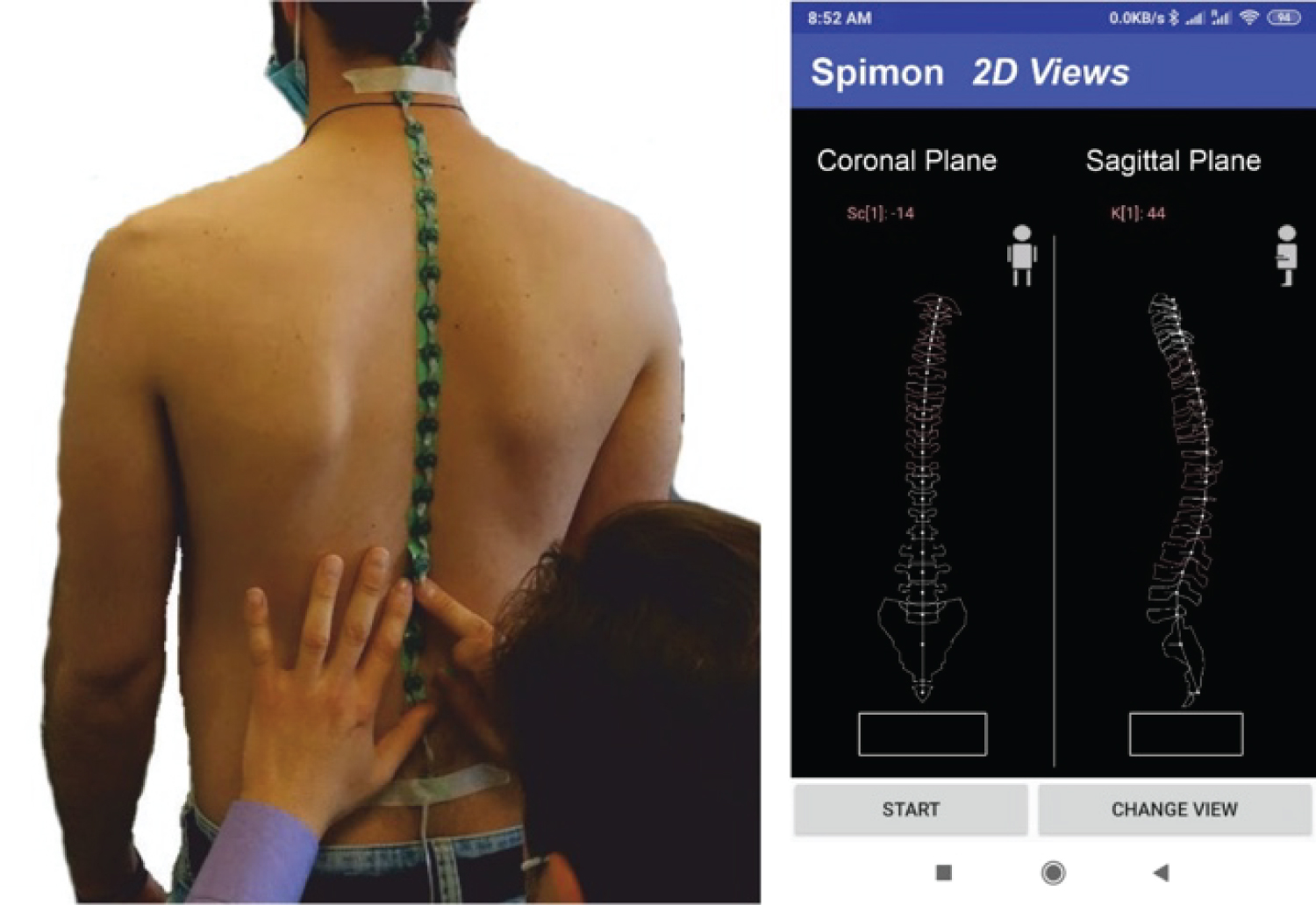 Figure 3: Application of the "SPIMON" system and real-time measurements animation in 2D Views.
View Figure 3
Figure 3: Application of the "SPIMON" system and real-time measurements animation in 2D Views.
View Figure 3
After system’s startup, the T1-T12 and L1-L5 Cobb angles are measured at 3 different positions: a) Normal Standing position, as previously described, b) Left and Right Bending, and c) Forward Flexion and Backward Flexion (Extension).
Measurements are taken in the Sagittal Plane and Cobb angles at T1-T12 and L1-L5 are calculated by the system. Figure 4 shows the Lumbar L1-L5 and Thoracic T1-T12 normal Cobb angles on Sagittal Plane.
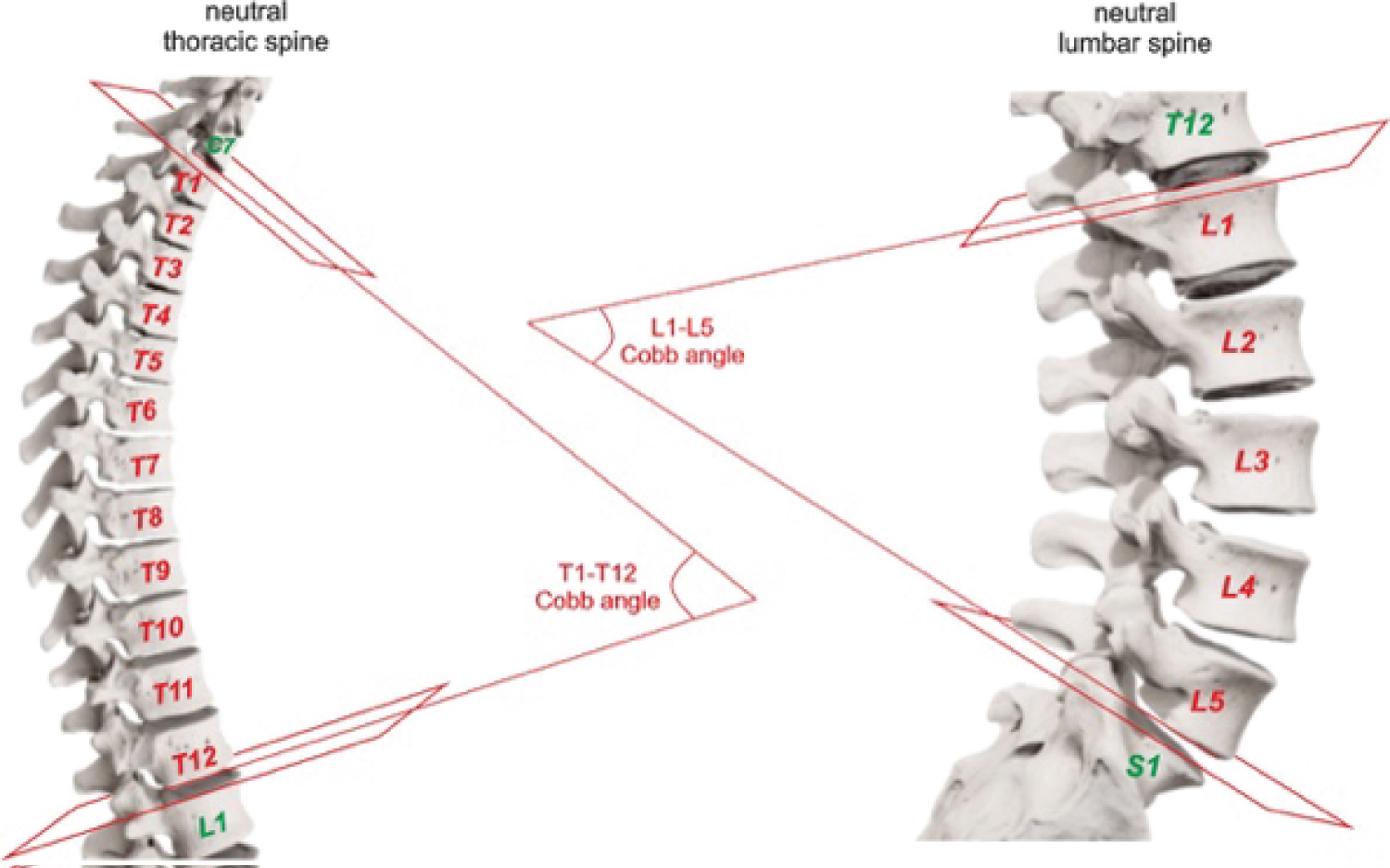 Figure 4: The lumbar L1-L5 and thoracic T1-T12 normal Cobb angles on sagittal plane.
View Figure 4
Figure 4: The lumbar L1-L5 and thoracic T1-T12 normal Cobb angles on sagittal plane.
View Figure 4
In the Coronal Plane, on a normal spine there are no angles, except for pathological cases such as scoliosis as it is shown in Figure 5.
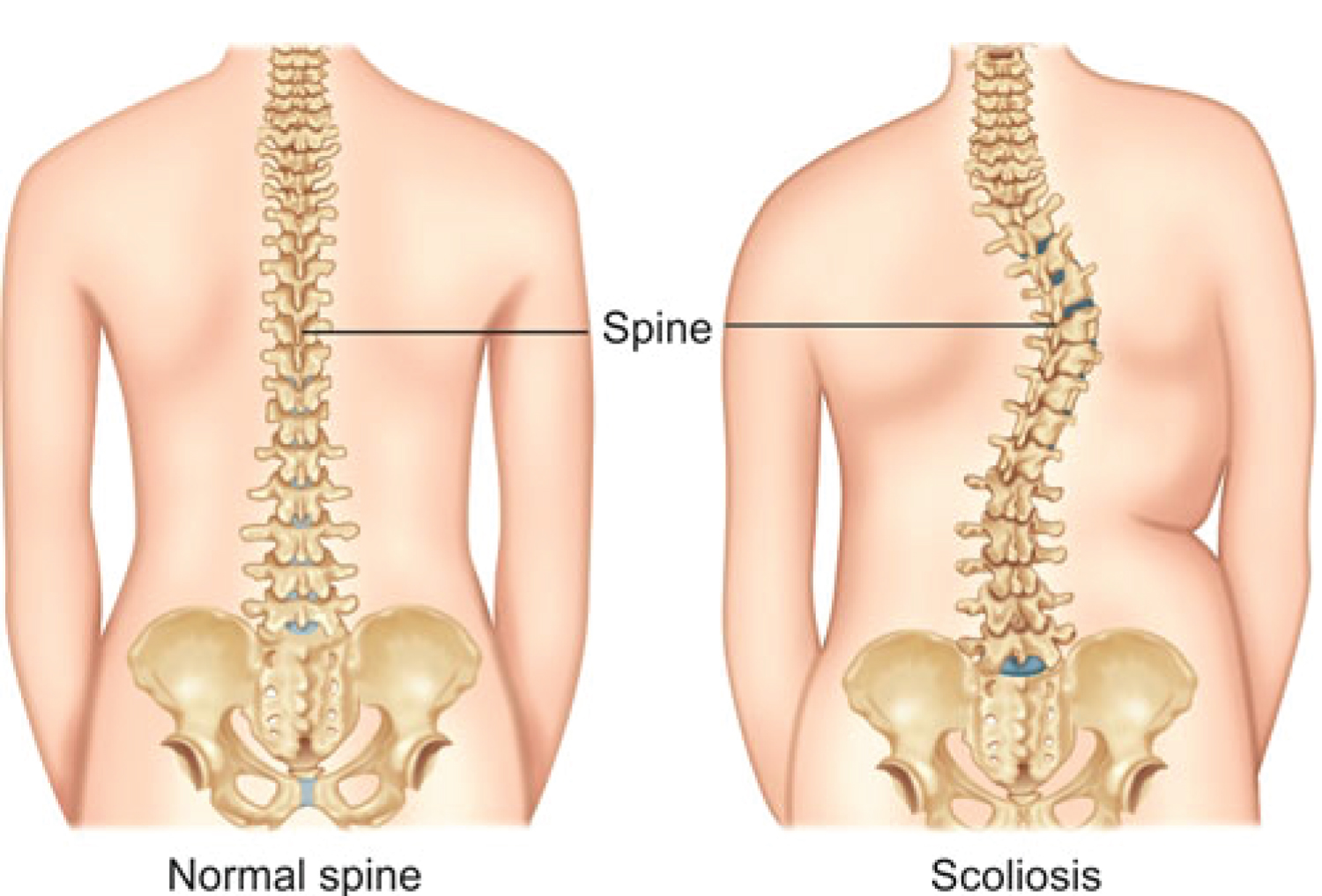 Figure 5: Ιn the Coronal Plane, on a Normal spine there are no angles. Scoliosis right curve (angle).
View Figure 5
Figure 5: Ιn the Coronal Plane, on a Normal spine there are no angles. Scoliosis right curve (angle).
View Figure 5
Right and left bending tests for measurements on the coronal plane are then performed. The subject bends on the right side aiming with the fingers of the right hand to reach the level of the right knee until the in house developed “3D motion tracking sensor” shows an angle of 30° degrees (Figure 6) [10].
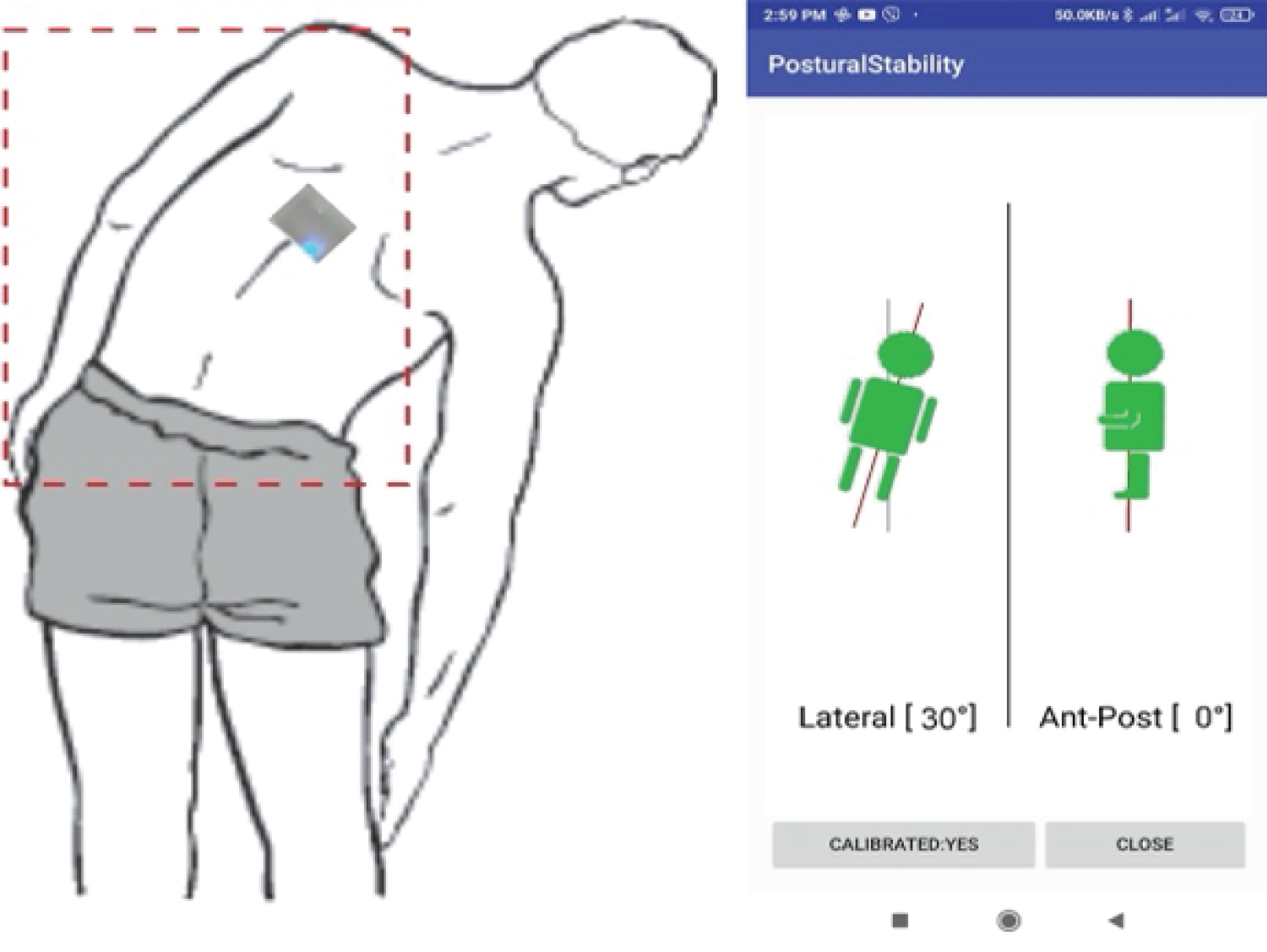 Figure 6: Right bending test with the use of the in house developed "3D motion tracking sensor".
View Figure 6
Figure 6: Right bending test with the use of the in house developed "3D motion tracking sensor".
View Figure 6
The same procedure is followed for the left side bending test.
Forward flexion and backward flexion measurements concern measurements on the sagittal plane.
The subject bends forward until the “3D motion tracking sensor” shows an angle of 65° degrees. The same procedure is followed for the backward bending test until the “3D motion tracking sensor” shows an angle of -15° degrees (Figure 7).
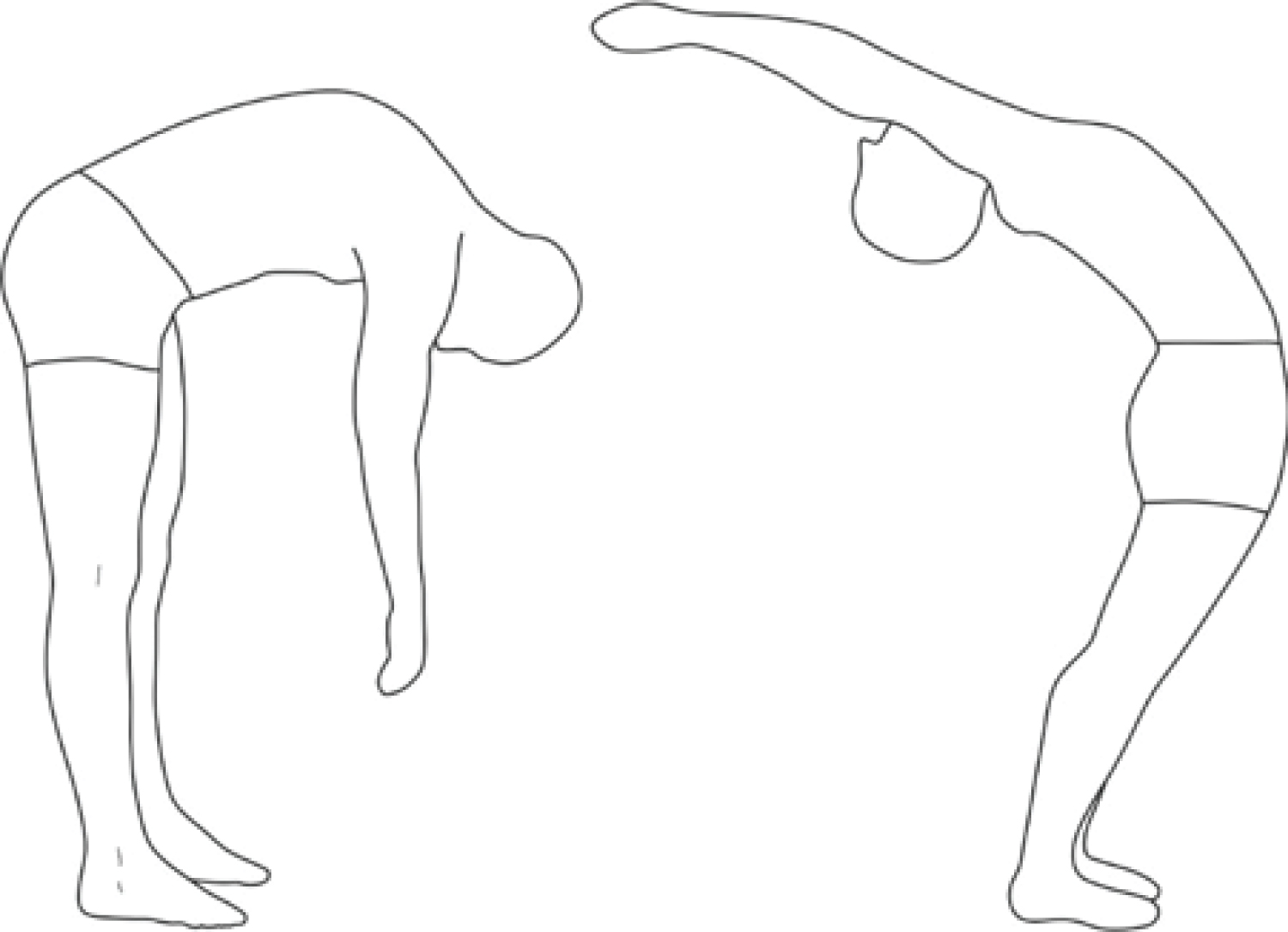 Figure 7: Forward/Backward bending test - Flexion/Extension.
View Figure 7
Figure 7: Forward/Backward bending test - Flexion/Extension.
View Figure 7
For the purpose of this study a group of 40 healthy volunteers (26 male and 14 female) with a median age of 43 years and an age range from 18 to 50, were finally selected out of 50 healthy volunteers initially examined. Ten subjects were excluded, due to shoulder imbalance, pelvic obliquity or rib hump.
Study’s results obtained after the examination of the group of 40 young, healthy volunteers, (26 men and 14 women), which were selected based on the inclusion criteria discussed before, and are presented in the following manner:
Thoracic Forward Flexion and Thoracic Backward Flexion (Extension),
Lumbar Forward Flexion and Lumbar Backward Flexion (Extension),
Thoracic Spine Bending Tests,
Lumbar Spine Bending Tests
The results of the Thoracic Spine Normal Standing T1-T12 in the sagittal plane using “SPIMON” is 46° degrees (mean value) with a range of (35° to 57°) which is a value very close to the average value of 47° degrees that reflect to the Thoracic Spine Normal Standing, see Figure 8, according to the literature [11-23], see Table 1.
Table 1: T1-T12 Sagittal plane literature average results vs. "SPIMON" measurements. View Table 1
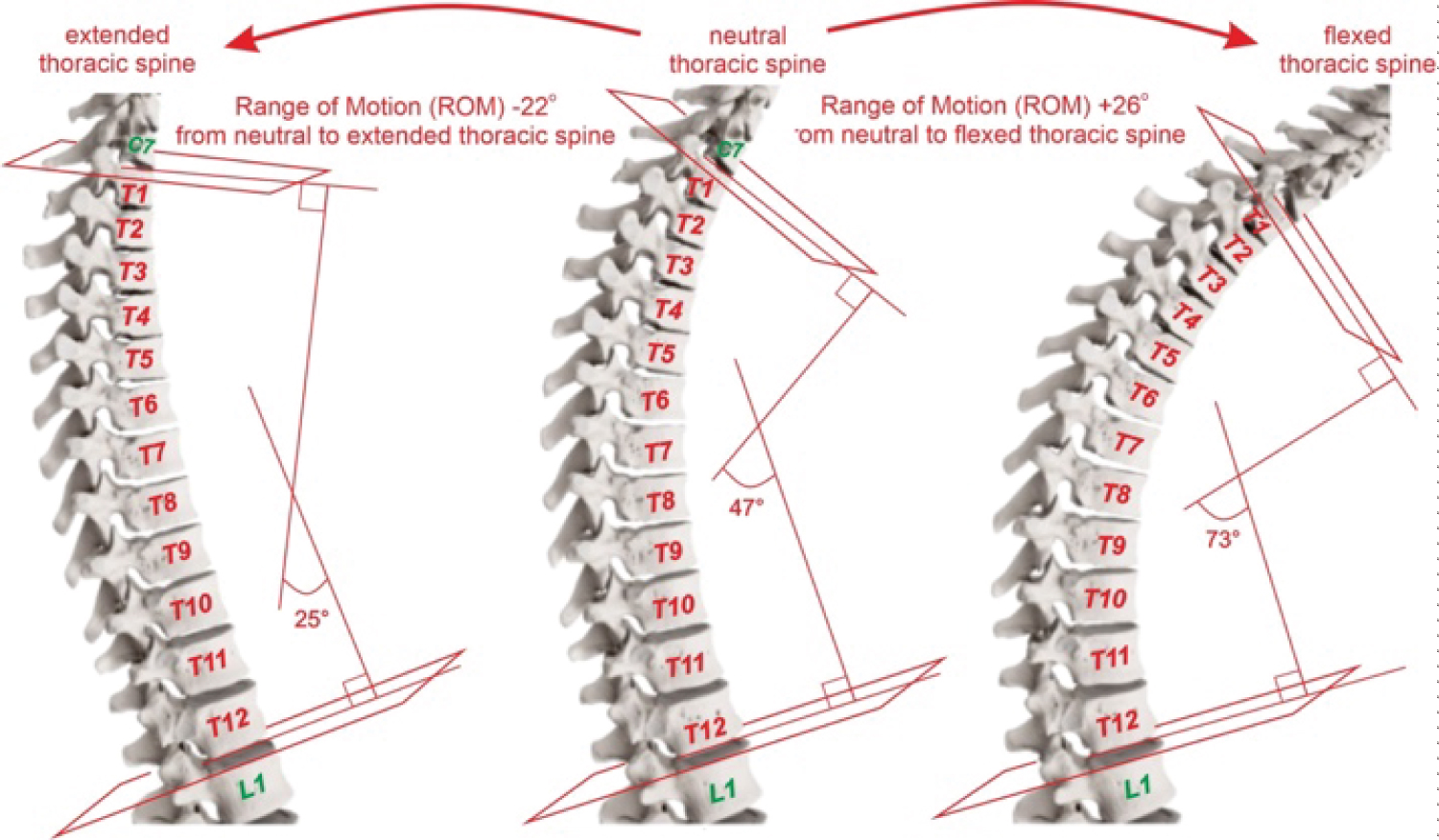 Figure 8: In the sagittal plane, the neutral normal T1-T12 angle of 47°, the maximum flexed T1-T12 ROM of 26° and the maximum extended T1-T12 ROM of -22° (normal data retrieved from the literature [11-23]).
View Figure 8
Figure 8: In the sagittal plane, the neutral normal T1-T12 angle of 47°, the maximum flexed T1-T12 ROM of 26° and the maximum extended T1-T12 ROM of -22° (normal data retrieved from the literature [11-23]).
View Figure 8
The preliminary results of the Thoracic Spine Forward Flexion in the sagittal plane reveal that the average value is 71° with a range of (61° to 85°), that is in accordance with the literature’s measurements average value 73° as they are published in [11-23], see Table 1.
The Range of Motion (ROM) computation reveals an average value of 25° with a range of (18° to 33°) that is in accordance with the literature average value of 26° also found in [11-23], see Table 1.
The results of the Thoracic Spine Backward Flexion (Extension) in the sagittal plane with “SPIMON” reveal an average value of 24° with a range of (15° to 35°), that is in accordance with the published literature’s average value of 25° [11,13-16,18, 20,22-25], see Table 1. The Range of Motion (ROM) computation reveals an average value of -21° with a range of (-16° to -32°) that is in accordance with the literature average value of -22° [11,13-16,18, 20,22-25], see Table 1.
The literature is extremely divergent regarding the range of normality in Spine normal values [11-34]. This way, the results of the Lumbar Spine Normal Standing L1-L5 in the sagittal plane using “SPIMON” is -38° degrees (mean value) with a range of (-35° to -50°) which is in accordance with the majority of literature results [20,23,28-31]. On the other hand, the average value that reflects to a “perfect” Lumbar Spine Normal Standing is -55° [11,15,20,22,23,26-31], see Figure 9 and Table 2.
Table 2: L1-L5 Sagittal plane literature results vs. "SPIMON" measurements. View Table 2
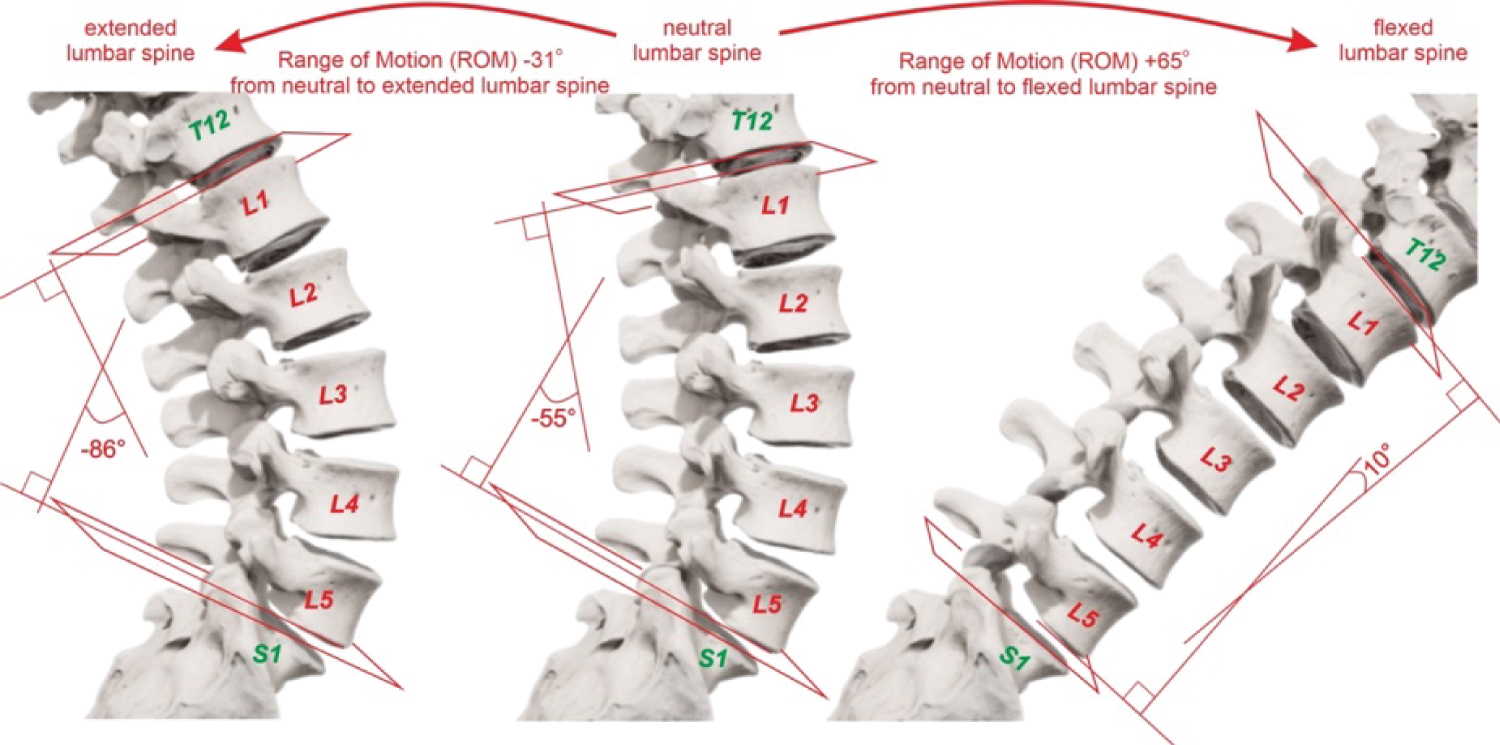 Figure 9: In the sagittal plane, the neutral normal L1-L5 angle of -55°, the maximum flexed L1-L5 ROM of 65° and the maximum extended L1-L5 ROM of -31°.
View Figure 9
Figure 9: In the sagittal plane, the neutral normal L1-L5 angle of -55°, the maximum flexed L1-L5 ROM of 65° and the maximum extended L1-L5 ROM of -31°.
View Figure 9
The results of the Lumbar Spine Forward Flexion in the sagittal plane using “SPIMON” reveal that the average value is 5° with a range of -12° to 13°, while the literature average value is 10° [11,15,20,22,23,26-31], see Table 2. The Range of Motion (ROM) computation using “SPIMON” reveals an average value of 44° with a range of (23° to 63°) that is in accordance with the majority of literature results [20,23,28-31]. On the other hand, the literature average value is 65° [11,15,20,22,23,26-31], see Table 2.
The -38° measured as the Lumbar Spine Normal Standing L1-L5 in this series versus the -55° published in [11,15,20,22,23,26-31] reveals a difference of 17°. The maximum Lumbar Forward Flexion was measured at 5° in this series while the literature average value is 10°. The different “starting point” (-38° vs. -55°) and the almost same “ending point” (5° vs. 10°) explain the difference of 21° between the ROM measured in this series and the literature, that is 44° vs. 65° respectively, see Table 2.
The preliminary results of the Lumbar Spine Backward Flexion (Extension) using “SPIMON” reveal that the average value is -68° with a range of -81° to -60° which is in accordance with the majority of literature results [20,23,28-31], while the literature average value is -86° [11,15,20,22,23,26-31], see Table 2.
The Range of Motion (ROM) computation using “SPIMON” reveals an average value of -29° with a range of (-20° to -36°) that is in accordance with the literature average value of -31° [11,15,20,22,23,26-31], see Table 2.
The results of the Thoracic Spine Normal Standing measured with “SPIMON” is -1,5° with a range of (-6° to 5°) which is in accordance with the literature 0° that reflect a “perfect” Thoracic Spine Normal Standing [11,13-15,18,20,22-24,32,33], see Table 3. The results of the Thoracic Spine bending tests (Right and Left side in the coronal level) reveal that the average value of Right side bending test is 19° with a range of (14° to 25°), while the average value of Left side bending test is -22° with a range of (-34° to -10°). There is no significant clinical difference between the measurements of the Right in comparison to the Left side, see Table 3. The Range of Motion (ROM) computation reveals an average value of 21° and -22° with a range of (14° to 28°) and (-34° to -7°) Right and Left respectively, see Table 3.
Table 3: T1-T12 Coronal plane literature results vs. "SPIMON" measurements. View Table 3
These results are significantly lower than the normal values for the Thoracic Spine bending tests which are around 30° degrees Right and -30° degrees Left, see Figure 10, [11,13-15,18,20,22-24,32,33], see Table 3.
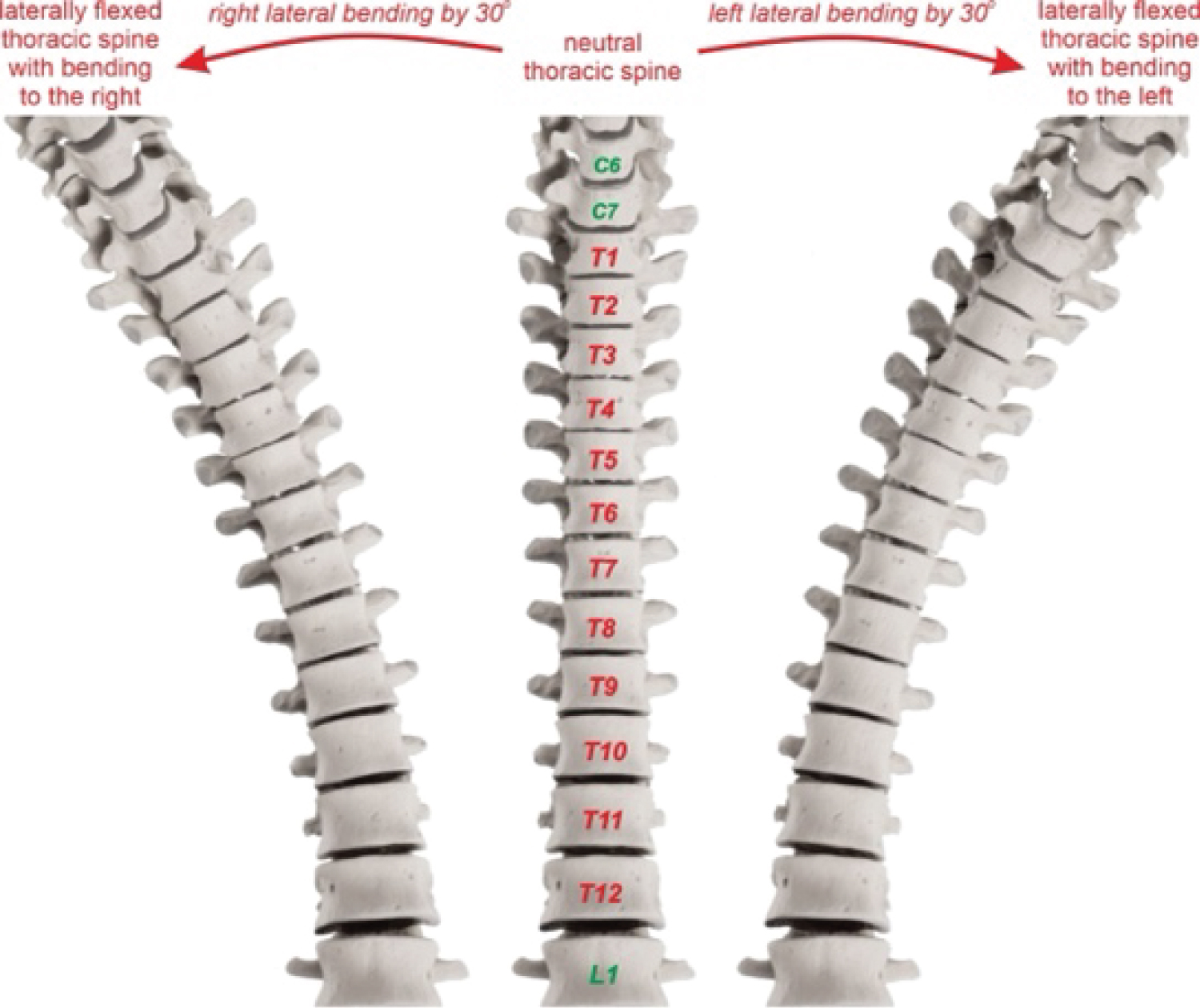 Figure 10: In the coronal plane, the neutral normal Th1-Th12 0° position and the maximum flexed Right or Left Th1-Th12 ROM of 30°.
View Figure 10
Figure 10: In the coronal plane, the neutral normal Th1-Th12 0° position and the maximum flexed Right or Left Th1-Th12 ROM of 30°.
View Figure 10
The difference between this paper’s measurements and the literature happens due to the measurement protocol used in this study. In order to standardize the measurements, the subjects were asked to bend laterally (right and left) until their fingers reach the level of their knees AND until the “3D motion tracking sensor” shows an index of 30° degrees. Most of the subjects were capable of bending further laterally but they were instructed to return to the less extreme position that was previously described resulting this way to an average value of 21° and -22° right and left respectively, instead of the 30° degrees normal value.
The results of the Lumbar Spine Normal Standing with “SPIMON” are 0 degrees with a range of (-5° to 5°) which is in full accordance to 0° degrees that reflect a “perfect” Lumbar Spine Normal Standing [11,15,20,22,23,26-29,31,33], see Table 4. The results of the Lumbar Spine bending tests (Right and Left side in the coronal level) reveal that the average value of Right side bending test is 17° with a range of (10° to 29°), while the average value of Left side bending test is -18° with a range of (-27° to -9°). There is no significant difference between the measurements of the Right in comparison to the Left side, see Table 4. The Range of Motion (ROM) computationwith “SPIMON” reveals an average value of 17° and -18° with a range of (12° to 26°) and (13° to 24°) Right and Left respectively, see Table 4.
Table 4: L1-L5 Coronal plane literature results vs. "SPIMON" measurements. View Table 4
These results are significantly lower than the normal values for the Lumbar Spine bending tests which are around 25° degrees Right and -25° degrees Left, see Figure 11, [11,15,20,22,23,26-29,31,33], see Table 4.
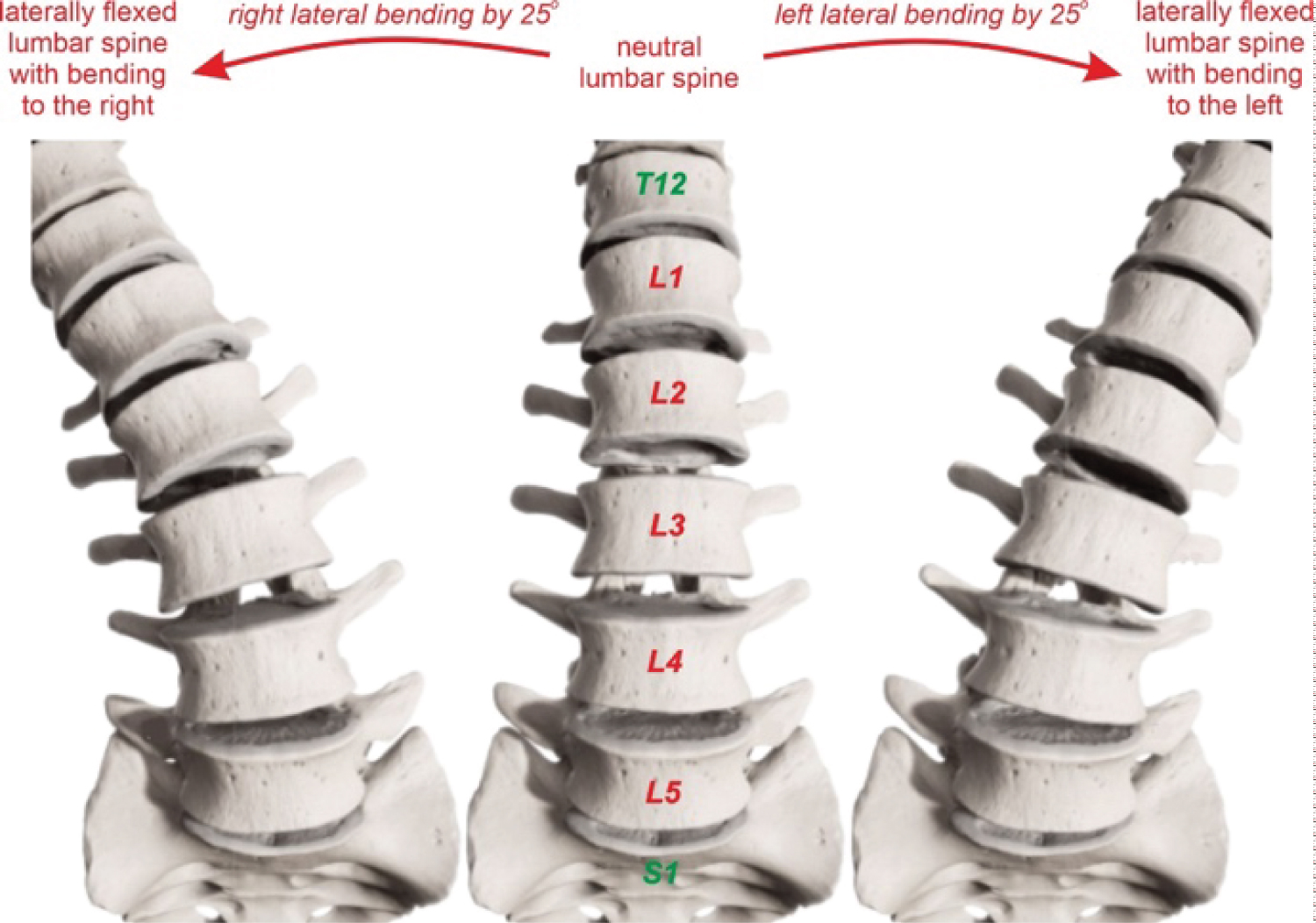 Figure 11: In the coronal plane, the neutral normal L1-L5 0° position and the maximum flexed right or left L1-L5 ROM of 25°.
View Figure 11
Figure 11: In the coronal plane, the neutral normal L1-L5 0° position and the maximum flexed right or left L1-L5 ROM of 25°.
View Figure 11
The difference between the obtained results and the literature is due to the measurement protocol used in this study in order to standardize the measurements of the different subjects, as is already explained in the section of Thoracic Spine Bending Tests.
The literature is extremely divergent regarding the range of normalityin Spine normal values in the traditional anatomical planes [11-34]. “SPIMON” results were within normal limits regarding Thoracic and Lumbar Flexion and Extension previously published data. On the other hand, “SPIMON” results were significantly lower compared to those previously published, regarding the Thoracic and Lumbar Bending Tests . This is associated to the measurement protocol used in this study in order to standardize the way measurements are taken on different subjects. In the case of the Thoracic and Lumbar Flexion and Extension the subjects were able to move till their maximum range of motion, therefore the “SPIMON” results turned out to be in accordance with the literature results. In the case of the Thoracic and Lumbar Bending Tests the subjects were able to bend further but they were instructed to stop at the 30° bending, therefore resulting this way to lower measured values from “SPIMON”.
Further general remarks are highlighted showing a greater lateral bending of the Thoracic Spine in comparison to the Lumbar Spine. The difference between Thoracic and Lumbar Spine Left bending is 4° (-22° vs. -18°) while the difference between Thoracic and Lumbar Spine Right bending is 2° (19° vs. 17°). These results are clinically insignificant between Right and Left and are compatible with the majority of literature data which refer to an around 5° degrees greater flexibility of the Thoracic Spine in comparison to the Lumbar Spine, in lateral bending [12-33].
As presented, the proposed “SPIMON” system comes in accordance with the known literature results and measurements, while at the same time introduces a series of advantages including: Real-time monitoring and observing of the Spine, Relatively simple and easy donning on and off and a non-radiation and non-invasive system .
So far, the “Golden Standard” for diagnosing and evaluating the progress of a Spinal Deformity is the X-rays. X-rays of the whole Spine Face and Profile, as well as “bending tests” on the maximum bending right and on the left side are used in order to evaluate the rigidity or not of a Spinal Deformity. This procedure is a static procedure that gives information regarding the position of the Spine in the final posture.
A main advantage of the proposed system is the ability to observe the movement of the Spine in real-time. In this case, a Spinal Expert can watch in real-time the whole movement of the Spine from a neutral position till the final posture and then back to the neutral position till the other side final posture and back to the neutral position. This dynamic view of the Spine and not static as used so far offers new capabilities to Spine Experts towards further understanding the functionality of the Spine.
Stability or fusion issues between one, two, or more Spinal levels are common areas of clinical and research interest in cases of rigid deformities, surgical stabilization with instrumentation, or degenerative pathologies. These cases can be further studied regarding their diagnosis and monitoring in a much more detailed way since the movement of the Spine and the levels of interest can be observed dynamically in real-time and in the whole range of motion.
Instability issues, such as Spondylolisthesis or Spondylolysis, can be further studied since the real-time observation of the Spinal movement can reveal the exact Spinal levels, in the whole range of motion, where the removal between two vertebrae happens and/or where and when the greater amount of removal takes place. Placing of the system sensors requires the palpation of the spinous processes of the lumbar and thoracic Spine and the stabilization of the sensors using an adhesive. The taking out of the system requires simple traction that easily detaches the sensors from the spinous processes.
The proposed system does not use any kind of radiation as it is used in the X-rays, protecting this way the developing body of children and adults from necessary exposure to radiation. The amount of radiation becomes significant, especially in young children that are treated with Braces, where the compliance of the patient and the efficacy of the customized Brace, require regular whole Spine X-rays. Finally, placing of the sensors does not require any invasive method apart from a simple sticky material stabilized on the skin of the patient.
Disadvantages of the proposed system may be a Low accuracy in obese patients and User dependent results . Placing of the system is in general based upon the medical expert. Although the palpation of the spinous processes does not require special expertise, the experience and the patience required is dependent on each user depended. As placing of the system requires the palpation of the spinous processes, in cases of obese patients where there is plenty of fat tissue placing of the sensors may not be as accurate. In addition, the main advantage of the system that is the real-time, in motion observing of the Spine, could be seriously affected since the fat tissue and the skin are much more moveable in obese patients and therefore may not reflect the real movement of the spinous processes.
Nevertheless, a deformity of the Spine is not an issue that requires exact placement and accurate, detailed measurements. A Spinal deformity is firstly diagnosed by a simple physical examination of a Pediatrician or an Orthopedic, without any use of equipment. Therefore, even in the case of obese patients, the proposed system can detect Spinal deformities and furthermore can monitor and estimate the deformity progress much better than the simple physical examination.
Future work should address some additional issues, such as: to obtain measurements from abnormal Spines and to prove the efficacy of the system comparing them with measurements that come out from the “Golden Standard” that is the X-Rays. Additionally, an updated version of the proposed system, designed for easier placement not requiring palpation of the spinous processes, it will not be necessary to put every IMU sensor upon every spinous process as well as better visualization in terms of more detailed 3D graphics could resolve medical expert dependability.
“SPIMON” results were within normal limits regarding Thoracic and Lumbar Flexion and Extension previously published data. On the other hand, “SPIMON” results were significantly lower compared to those previously published, only regarding the Thoracic and Lumbar Bending Tests but this was due to the measurement protocol used in this study.“SPIMON” presented significant advantages such as: real-time monitoring and observing of the Spine, relatively simple and easy donning on and off and a non-radiating, non-invasive procedure. On the other hand, “SPIMON” disadvantage is the user dependent reliability based on the experience and patience of the user. Finally, measurements from abnormal Spines X-Rays must be compared to “SPIMON” measurements in order to further prove the reliability of the system.