Background: The practice of classical ballet requires constant, prolonged physical training periods, and the repetition of aesthetic movements that exceed anatomical limits. Joint misalignment during sustained posture or movement execution is one of the principal risk factors for injury in the dance world. Injury prevention strategies based on correcting altered movement patterns need to be targeted by health professionals during the teaching-learning-training process. The aim of this study was to determine the effects of an intervention program based on Piret and Beziers' Motor Coordination principles on knee alignment, foot arch stability and pelvic position in pre-professional ballet dancers.
Methods: Twenty dancers from 7th year of the Bolshoi Theatre School in Brazil underwent an intervention program based on Motor Coordination principles. The intervention program was composed of three different types of sessions (individual home-based sessions, supervised group sessions and "life lessons") focusing on exercises that organize the lower limb torsion, torso stabilization and proprioception. The outcomes included knee center alignment (patella related to 2nd toe), pelvic position (tilt) and foot arch stability (stable/unstable). They were assessed using the Dynamic Evaluation Method of Lower Limb Joint Alignment (MADAAMI) during one sequential execution of classical ballet steps (demi-plié, grand plié, and fondu), in three feet positions: Parallel, 180° En dehor, and self-select En dehor. The Friedman test was used to determine the time-effects on dependent variables and the Wilcoxon test was used to identify differences between two consecutive periods (pre- and post-control, pre- and post-intervention, pre- and post-follow-up). The effect size was calculated to examine the practical significance of the results.
Results: Small and medium effects were identified in knee center alignment during several sequential execution phases of the feet in self-selected and 180° turnout positions. Regarding knee center alignment, during the feet in parallel position, changes in the number of occurrences from lowest to highest scores following the intervention period were only identified during the fondu step with medium effect size. No differences were observed between post-intervention and follow-up period for any of the variables.
Conclusions: The intervention promoted knee center alignment, which persisted after 24 weeks, beyond supervised sessions. No effects in the pelvic position or in the foot arch were observed.
Dancing, Clinical trial, Exercise therapy
MADAAMI: Dynamic Evaluation Method of Lower Limb Joint Alignment in Portuguese Método de Avaliação Dinâmica do Alinhamento Articular dos Membros Inferiores; PSIS: Posterior Superior Iliac Spine; ASIS: Anterior Superior Iliac Spine; SK1: Extended Knees before Demi-Plié; DPD: Demi-Plié Descent; DP: Demi-Plié; DPA: Demi-Plié Ascent; SK2: Extended Knees before Grand Plié; GPD: Grand Plié Descent; GP: Grand Plié; GPA: Grand Plié ascent; SK3: Extended Knees before Fondu; FOD: Fondu Descent; FO: Fondu; FOA: Fondu Ascent; ES: Effect Size
The practice of classical ballet requires constant, prolonged physical training periods, choreographic technical complexity and the repetition of aesthetic movements with a wide range of motion that exceed the anatomical limits [1,2]. Thus, unsurprisingly there is a high prevalence of lower-limb injuries among classical ballet dancers due to overuse [3-6] and multifactorial causes, such as muscle fatigue, inadequate flooring or insufficient rest time [4,7].
Furthermore, there seems to be a consensus that joint misalignment during sustained posture or movement execution is one of the principal risk factors for injury in the dance world [3,4,8,9]. This approach is based on the premise that these joint misalignments generate compensatory movements, reduce the body's capacity to absorb forces and exceed the mechanical threshold of musculoskeletal tissues [3,10-12]. It is believed injury prevention strategies based on correcting altered movement patterns need to be targeted by health professionals during the teaching-learning-training process [13-15]. The Motor Coordination principles, as described by Piret and Béziers [16], represent an alternative physiotherapeutic approach which envisages posture and movement re-education [16-18].
We believe that the alignment of the joint structures dictates how forces are absorbed and transferred throughout the body. Based on this, it is hypothesized that an intervention program with therapeutic exercises that emphasize a physiological joint alignment during technical ballet steps could be an effective strategy for decreasing injury risk factors [17]. Thus, the aim of this study was to determine the effects of an intervention program based on Piret and Beziers' Motor Coordination principles on the knee alignments, foot arch stability and pelvic position in pre-professional ballet dancers.
This experimental study was approved by the Research Ethics Committee of the university. All participants were recruited from the Bolshoi Theatre School in Brazil and provided written consent before data collection. Thirty hours per week is the average training time at this school, and this training lasts 8 years. This study was conducted between 2014 and 2016. During this period, 39 participants were recruited, evaluated and submitted to a 4-week intervention program. The intervention was conducted when the participants were in the 7th grade level of the ballet school. Twenty participants were submitted to a control period during 2014 when no intervention was conducted, and they were oriented to maintain their normal routine of ballet classes. These participants were evaluated at four different time points: pre-control, pre-intervention, post-intervention and post-follow-up. For these participants, the intervention occurred during the year 2015 (Figure 1). Another 19 participants were recruited in 2016, which are not submitted to a control period, and they were evaluated at only three different time points (pre-intervention, post-intervention and post-follow-up) during the 2016 year (Figure 1).
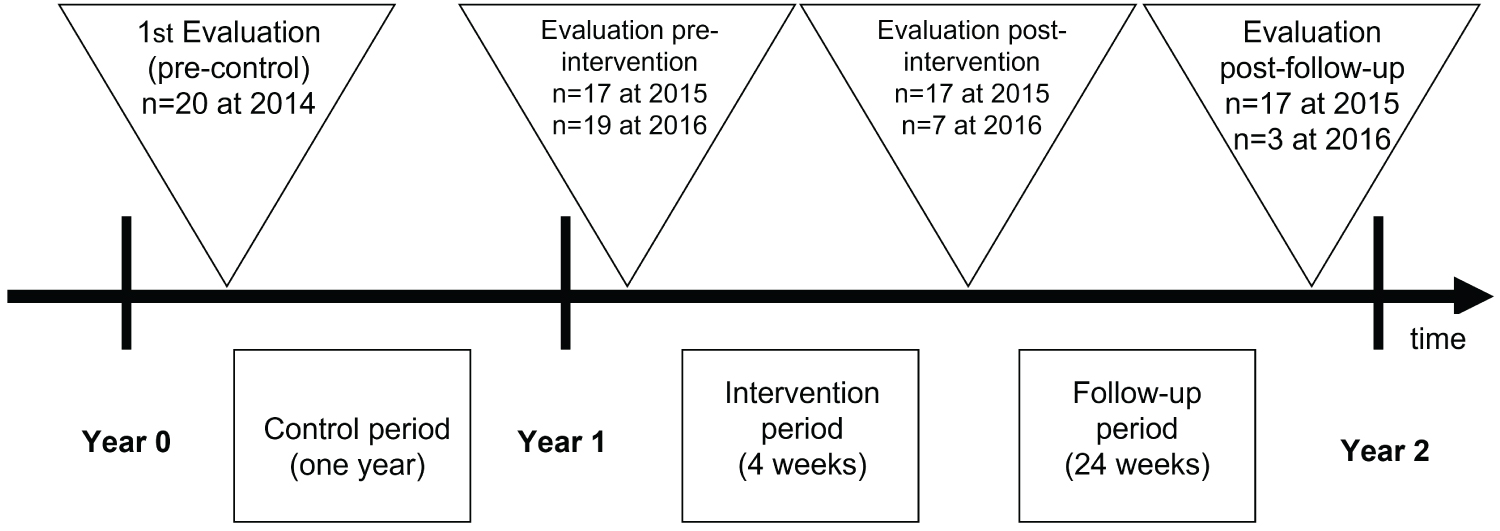 Figure 1: Study design for evaluations and intervention.
View Figure 1
Figure 1: Study design for evaluations and intervention.
View Figure 1
Thirty-nine dancers were initially recruited to participate in the present study, 20 in 2014 and 19 in 2016. The sample was intentional, and the participants were recruited via advertisements published on murals in the ballet school. The inclusion criteria required candidates to be regularly matriculated in the 7th-grade level of Bolshoi Theatre School during the intervention period and aged between 15 and 21 years. The following exclusion criteria were observed: musculoskeletal injury during the study period and surgery performed in the previous six months.
Participants were excluded from the data analysis in the case of absence during the evaluation protocol, less than 100% adherence to the supervised sessions or less than 75% adherence to the home-based exercises. The researchers responsible for data collection and data analysis, with 3 years of experience in postural evaluation, were blinded in relation to the program intervention.
Knee center alignment, pelvic position and foot arch stability were assessed using the Dynamic Evaluation Method of Lower Limb Joint Alignment (MADAAMI) by one researcher with experience in the use of this method, who was blinded to the data analysis and to intervention. Details of the MADAAMI protocol were reported in previous studies that confirmed the validity and reliability of this method [19-21]. MADAAMI consist of: (i) Digital video recording of the lower limbs during sequential execution of classical ballet steps; and (ii) Checklist which helps the professional to measure change in knee alignment, foot arch stability and pelvic position based on pre-determined criteria and scores [20].
During the evaluation protocol, participants were required to be barefoot and wearing clothes that allowed the hips, knees, ankles, and feet to be clearly viewed [21]. Before the test, reflective markers were attached to the following anatomical points: the right posterior superior iliac spine (PSIS) and right anterior superior iliac spine (ASIS), the right foot second toe, the right navicular bone, the first metatarsophalangeal joint medial region, the fifth metatarsophalangeal joint lateral region and the anterior tibial tuberosity [21]. First, each participant was positioned at a previously prepared location based on the protocol proposed by MADAAMI [21]. They then performed the step sequence proposed [21] (a demi-plié, a grand plié, and a fondu) (Figure 2) three times, twice for familiarization and once for the digital video recording. The foot position order was randomly defined: (1) Feet in parallel position, (2) Feet in the 180-degree En dehorposition and (3) Feet in self-selected En dehor position. When in the parallel position, the feet were hip width apart. A one-minute interval was used between the tested positions. During the control period, only the feet in self-selected En dehor position were evaluated.
 Figure 2: Ballet movements analyzed demi-plié, grand plié, and fondu, respectively.
View Figure 2
Figure 2: Ballet movements analyzed demi-plié, grand plié, and fondu, respectively.
View Figure 2
The resulting data were analyzed by one researcher, blinded to data acquisition and the intervention, who was asked to rate the score sheet based on observation of the video recordings. The content of MADAAMI score sheet was also previously validated [21]. Briefly, the MADAAMI score sheet is divided into three criteria that are used to analyze each one of the executed steps (demi-plié, grand-plié, and fondu): 1) Foot arch stability, 2) Pelvic position and 3) Knee center alignment. Each criterion was evaluated in the following step phases: Extended knees before Demi-plié (SK1), Demi-plié descent (DPD), Demi-plié (DP), Demi-plié ascent (DPA), Extended Knees before Grand plié (SK2), Grand plié descent (GPD), Grand plié (GP), Grand plié ascent (GPA), Extended Knees before Fondu (SK3), Fondu Descent (FOD), Fondu (FO), Fondu Ascent (FOA) [21]. Thus, the foot arch stability was assessed as "Unstable toward the fifth toe", "Stable", or "Unstable toward the first toe"; the knee center alignment was assessed with the ipsilateral foot in static phase as "Above the fourth and fifth toe or beyond the fifth toe", "Above the second and third toes", or "Above or beyond out the first toe (femur internal rotation)", and dynamic phases as "Stable (starts and ends in the same position)", "Unstable (starts with internal rotation and ends above the second and third toes)", or "Unstable (starts with internal rotation and ends above or beyond the first toe)"; and the pelvic position (i.e., anterior and posterior pelvic tilt) was assessed in both the static and dynamic phases. The pelvic position was only assessed in the 180° and self-selected turnout foot positions.
In short, each of these criteria includes descriptive categories that are scored from 1 to 4 for the knee alignment, where the scores 1 and 2 indicate a performance that deviates from the theoretical norm, while scores 3 and 4 indicate a performance that conforms to the theoretical norm. For foot arch stability and pelvic position, the scores are from 1 to 3, where the scores 1 and 2 indicate a performance that deviates from the theoretical norm, while scores 3 indicate a performance that conforms to the theoretical norm. Therefore, the higher the MADAAMI score, the better the alignment [21].
A physiotherapist with 5 years of experience and blinded to the data acquisition and data analysis conducted the intervention protocol. The intervention program was based on the Motor Coordination principles (i.e. adequate proprioceptivity, motor control and balance between the tension produced by antagonist muscles) [16-18].
For the creators of the Motor Coordination principles, the knee joint is the central point between the external femoral rotation and the internal tibial rotation produced by the iliopsoas, the sartorius and the tibialis anterior muscles. In other words, this antagonistic opposition between rotations is brought about by "organizational tension" that keeps the tibia rotating internally, as opposed to the tension for external rotation exerted on the femur. This condition ensures alignment of the bone segments and knee stabilization, which is essential for dancers since the injuries can be caused by the loss of tibial internal rotation when performing the maximal turnout position [11-13] (Figure 3 and Figure 4).
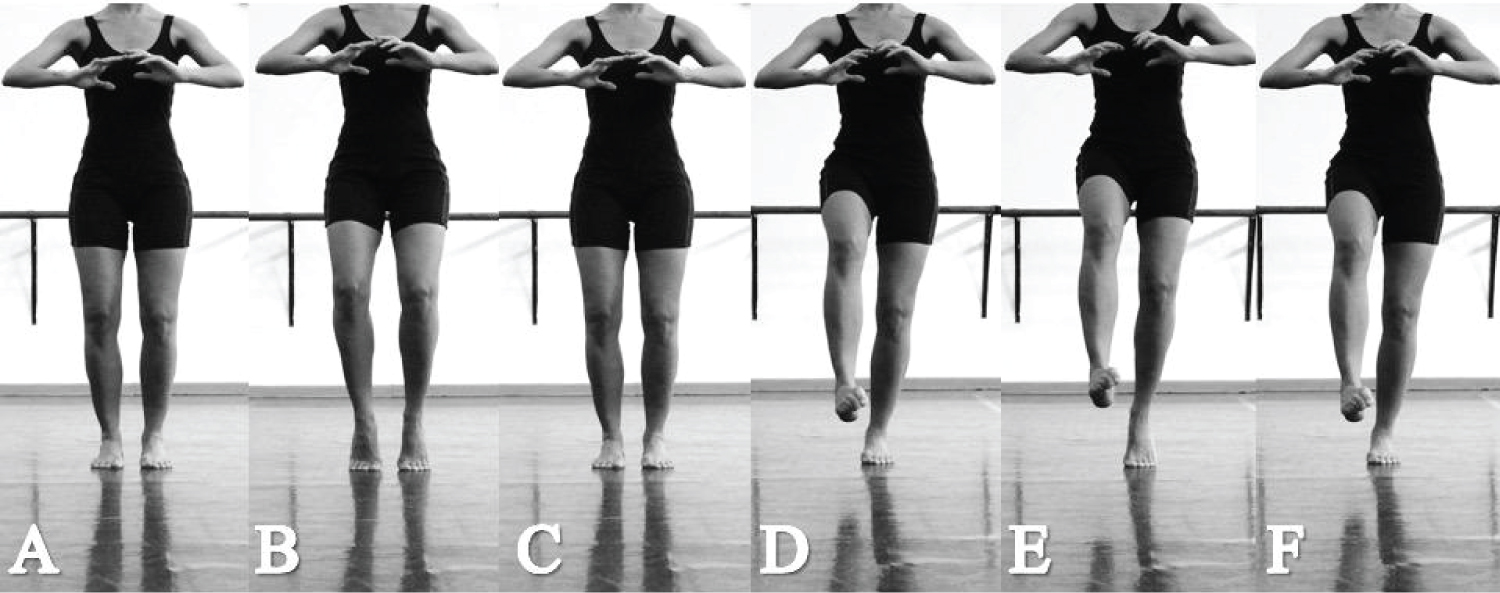 Figure 3: Sequence of Alavanca exercise with torsions of the motor coordination of Piret and Béziers. (A, B and C) Bilateral task and; (D, E, and F) Unipodal task.
View Figure 3
Figure 3: Sequence of Alavanca exercise with torsions of the motor coordination of Piret and Béziers. (A, B and C) Bilateral task and; (D, E, and F) Unipodal task.
View Figure 3
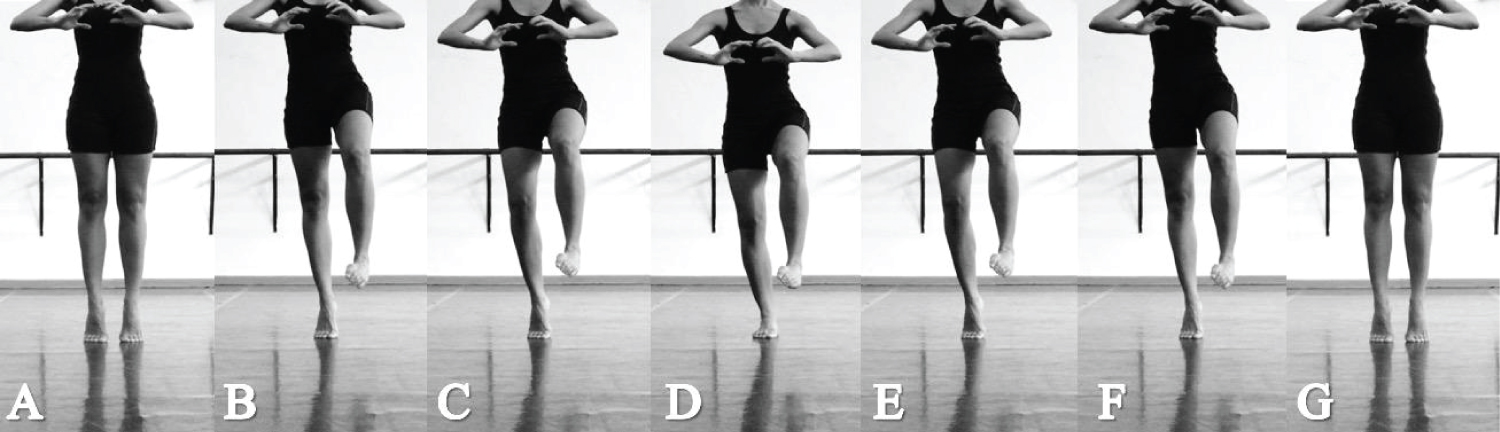 Figure 4: Sequence of Reggae exercises with torsions of the motor coordination of Piret and Béziers: (a) Initial position; (b) Weight transference and maintenance of demi-pointe in the supporting leg; (c) Flexion of the knee of the supporting limb lower; (d) Decent phase of the foot arch without noise and with maintenance of flexed knee and demi-pointe in the supporting limb; (e) Ascent phase of the foot arch without noise and with maintenance of flexed knee and demi-pointe in the supporting limb; (f) Extension of the knee of the supporting limb lower with maintenance of demi-pointe; (g) Weight transference for both limbs with maintenance of demi-pointe.
View Figure 4
Figure 4: Sequence of Reggae exercises with torsions of the motor coordination of Piret and Béziers: (a) Initial position; (b) Weight transference and maintenance of demi-pointe in the supporting leg; (c) Flexion of the knee of the supporting limb lower; (d) Decent phase of the foot arch without noise and with maintenance of flexed knee and demi-pointe in the supporting limb; (e) Ascent phase of the foot arch without noise and with maintenance of flexed knee and demi-pointe in the supporting limb; (f) Extension of the knee of the supporting limb lower with maintenance of demi-pointe; (g) Weight transference for both limbs with maintenance of demi-pointe.
View Figure 4
The intervention program focused on exercises that organize the lower limb torsions, torso stabilization and proprioception, involving the use of planks in different positions and on different support surfaces (Figure 5 and Figure 6). In practice, the program consisted of three different types of session: individual home-based sessions, supervised group sessions and sessions called by "life lessons", in which the participants were instructed regarding specific self-care tips and exercises they could do at home at any time during the intervention period (Table 1).
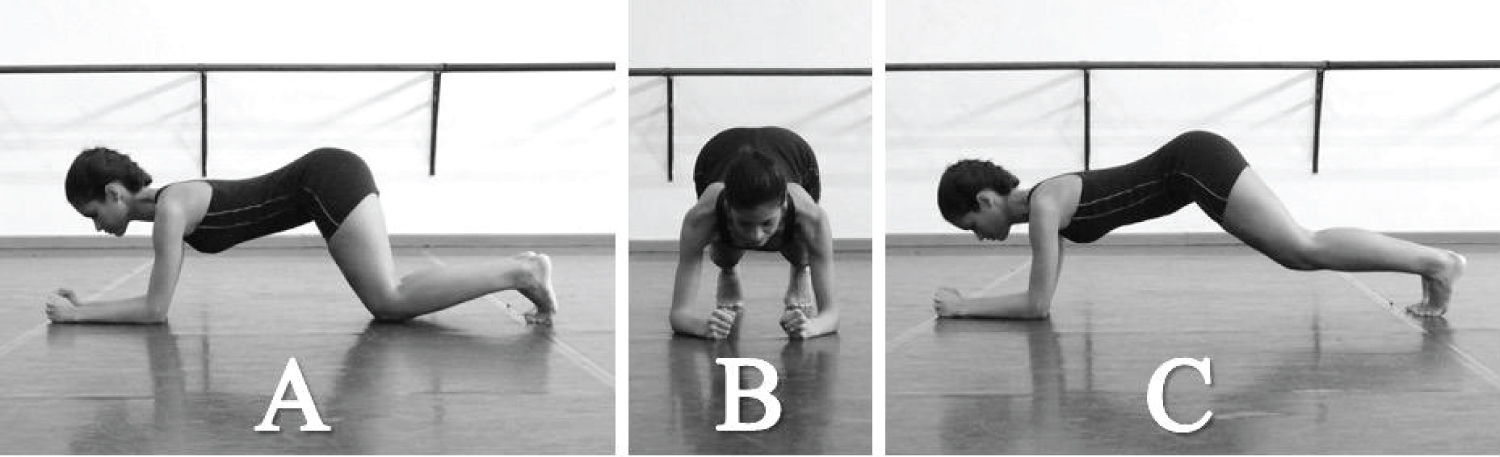 Figure 5: Frontal plank exercise: (a) Initial position, maintaining the lumbar region neutral while simultaneously activating the abdominal and pelvic floor muscles; (b) Note the knee and foot alignment while maintaining Piret and Béziers' Motor Coordination torsions; (c) Final position.
View Figure 5
Figure 5: Frontal plank exercise: (a) Initial position, maintaining the lumbar region neutral while simultaneously activating the abdominal and pelvic floor muscles; (b) Note the knee and foot alignment while maintaining Piret and Béziers' Motor Coordination torsions; (c) Final position.
View Figure 5
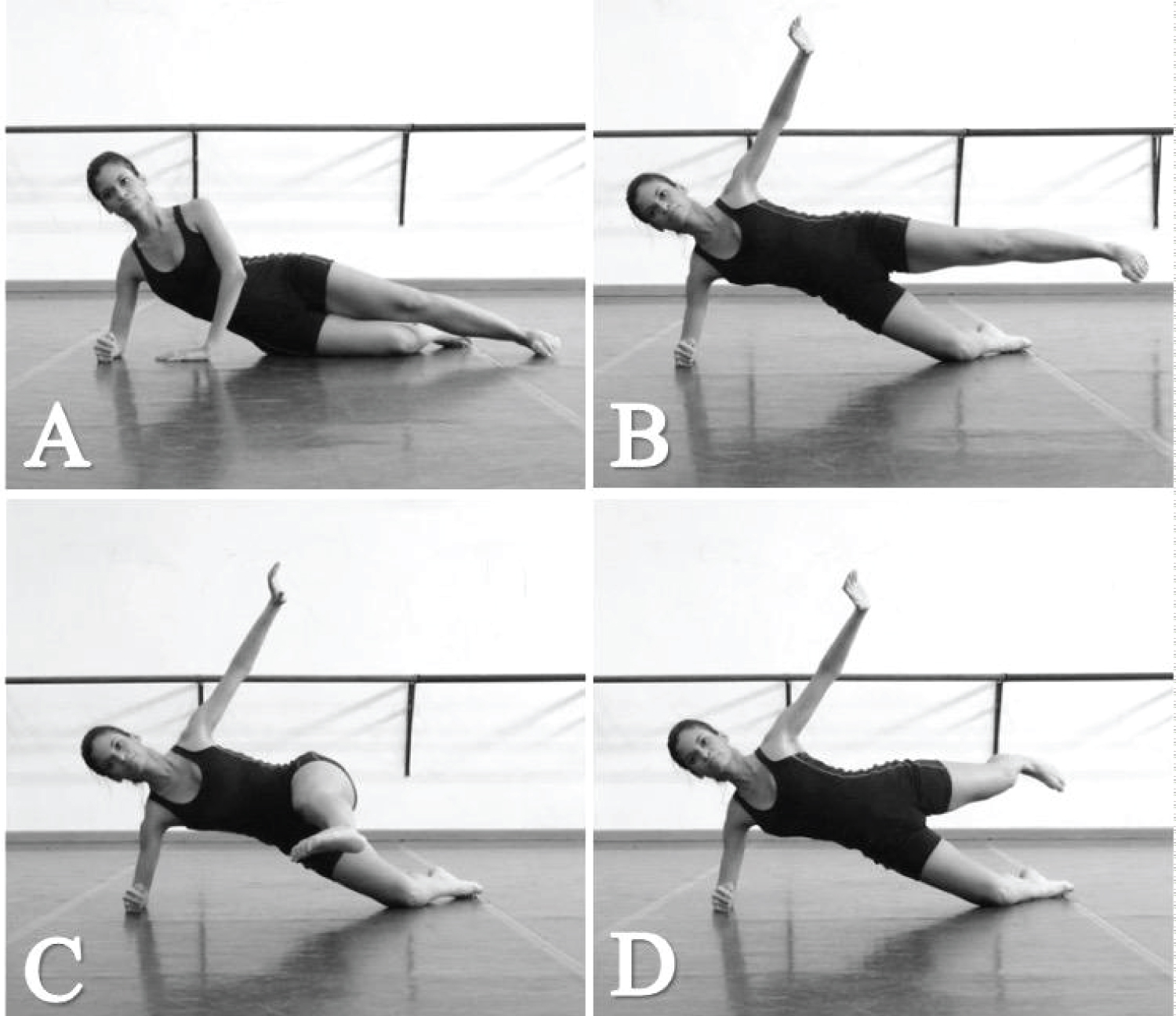 Figure 6: Lateral plank exercise with pendulum: (a) Initial position for organizing the neutral lumbar region and maintaining Piret and Béziers' Motor Coordination torsions (coordination position) during simultaneous activation of the abdominal and pelvic floor muscles; (b) Intermediate pendulum position where inhalation should be performed; (c) Anterior pendulum balance phase; (d) Posterior pendulum balance phase.
View Figure 6
Figure 6: Lateral plank exercise with pendulum: (a) Initial position for organizing the neutral lumbar region and maintaining Piret and Béziers' Motor Coordination torsions (coordination position) during simultaneous activation of the abdominal and pelvic floor muscles; (b) Intermediate pendulum position where inhalation should be performed; (c) Anterior pendulum balance phase; (d) Posterior pendulum balance phase.
View Figure 6
Thus, the participants attended 4 supervised group sessions, once a week, over a one-month period. Between sessions, the participants were expected to perform the home-based exercises twice a week and the life lessons as often as possible. In addition, in each session the participants were inquired about the frequency of home-bases and life lessons exercises.
At the end of intervention period, the participants were oriented to maintain the home-based exercises and the life lessons as part of their life and ballet classes. Table 1 summarises the content and main exercises developed during the intervention period. Figure 2, Figure 3, Figure 4 and Figure 5 show the typical exercises used in the intervention protocol.
Table 1: Summary of the main contents and exercises used in the intervention protocol. View Table 1
Using the knee center alignment as the main variable, the G*Power v.3.1.7 was used to estimate the sample size. Based on the Wilcoxon test (matched pairs), two tails, estimating the effect size in 0.5, α = 0.05 and power of 80%, a sample size of 35 subjects was obtained.
The Friedman test was used to determine the time-effects on the dependent variables. The Wilcoxon test, with the Bonferroni correction, was used to identify differences between two consecutive periods (pre- and post-control, pre- and post-intervention, pre- and post-follow-up). Magnitude-based inference analyses were also used to examine the results practical application. The magnitude of differences between pre- and post-intervention was calculated [22] and was interpreted using the following scale, which was proposed by Cohen [23]: Trivial effect (< 0.10), small effect (0.10-0.30), medium effect (0.30-0.50), and large effect (above 0.50). The significance level was α < 0.05 for all statistical analyses. The results are expressed as absolute and relative frequencies in tables when significant differences were detected.
Twenty participants (female = 8 and male = 12) completed the full protocol, (age = 18.5 ± 0.9 years, height = 1.7 ± 0.1 m and total body mass = 56.1 ± 8.5 kg). Six dropped out due to personal reasons or injury, one participant was dismissed from the School, and 12 participants failed to reach the required percentage of adherence to the intervention program sessions during the study (Figure 1). All the participants had more than 9 years of experience in classical ballet and more than 5 years dancing in the School of Bolshoi Theatre, in Brazil.
There were no significant differences between the pre-control and pre-intervention tests for the knee center alignment, foot arch stability or pelvic position in any of the assessed phases during each step (demi-plié, grand plié and fondu) performed with feet in the En dehor self-selected position (p > 0.05 for all).
Knee center alignment: Regarding the knee center alignment during the feet in the self-selected En dehorposition, a treatment effect was observed for the SK1 [X2(2) = 6.400, p = 0.041], DPD [X2(2) = 9.250, p = 0.010], DPA [X2(2) = 13.188, p = 0.001], SK2 [X2(2) = 6.400, p = 0.041], GPA [X2(2) = 11.000, p = 0.004], SK3 [X2(2) = 6.400, p = 0.041] and FO [X2(2) = 6.333, p = 0.042]. In addition, the adjusted Bonferroni test identified improvement in knee center scores following the intervention period for DPD (p = 0.014), DPA (p = 0,006), GPA (p = 0.016), a FOD (p = 0.017) and FO (p = 0.025). No differences were observed between post- intervention and follow-up (p > 0.05 for all, Table 2). The effect size between the pre-intervention and post-intervention tests were small for DP (ES = 0.22), GPD (ES = 0.27) and FOA (ES = 0.29) and medium for SK1 (ES = 0.31), DPD (ES = 0.38), DPA (ES = 0.43), SK2 (ES = 0.31), GP (ES = 0.33), GPA (ES = 0.37), SK3 (ES = 0.31), FOD (ES = 0.37) and FO (ES = 0.35).
Table 2: Number of occurrences absolute (and relative) for the knee center alignment scores in each phase of the feet in En dehors self-selected position during the study evaluation times. View Table 2
When the knee center alignment was investigated during the feet in the 180° En dehor position, a treatment effect was observed on the knee center for the SK1 [X2(2) = 1.333, p = 0.006], DPA [X2(2) = 14.000, p = 0.00]), SK2 [X2(2) = 10.333, p = 0.006], GPA [X2(2) = 6.059, p = 0.048], SK3 [X2(2) = 10.333, p = 0.006], FOD [X2(2) = 9.000, p = 0.011] and FOA (X2(2) = 17,077, p < 0.001]. The Bonferroni test showed an increased number of occurrences in the highest knee center scores following the intervention period for SK1 (p = 0.025), DPA (p = 0.006), SSK2 (p = 0.025), GPA (p = 0.009), SK3 (p = 0.025) and FOA (p = 0.003) (Table 3). No differences were found between post intervention and follow-up (p > 0.05, for all, Table 3). Trivial (DP, ES = 0.10), small (GDP, ES = 0.17; GP, ES = 0.12 and FO, ES = 0.15) and medium effect size (SK1, ES = 0.35; DPA, ES = 0.43; SK2, ES = 0.35; GPA, ES = 0.41; SK3, ES = 0.35; FOD, ES = 0.38 and FO, ES = 0.47) were found between the pre-intervention and post-intervention tests.
Table 3: Number of occurrences (absolute and relative) for knee center alignment in each phase of the feet in En dehors 180° position during the study evaluation times. View Table 3
Regarding the knee center alignment during feet in the parallel position, a treatment effect was observed for FOD [X2(3) = 12.019, p = 0.007] and FO [X2(3) D = 14.455, p = 0.002]. The Bonferroni test identified changes in the number of occurrences from lowest to highest knee center scores following the intervention period for FO (p = 0.015) (Table 4). No differences were observed between post-intervention and follow-up period (p > 0.05 for all, Table 4). The effect size was trivial (SK1, ES = 0.05; DDP, ES = 0.08; DPA, ES = 0.05; GPD and ES = 0.09), small (DP, ES = 0.17; SK2, ES = 0.15; GP, ES = 0.13; SK3, ES = 0.15 and FOA, ES = 0.17) and medium (GPA, ES = 0.31; FOD, ES = 0.31; FO, ES = 0.38) between the pre-intervention and post-intervention tests.
Table 4: Number of occurrences (absolute and relative) for knee center alignment in each phase of the feet in parallel position during the study evaluation times. View Table 4
Foot arch stability: With respect to arch foot stability during the feet in self-selected En dehor position, a treatment effect for FO was observed [X2(2) = 8.000, p = 0.018]. However, no difference between pre- and post-intervention (p > 0.05 for all) or between post-intervention and follow-up periods (p > 0.05 for all) was found using the adjusted Bonferroni test.
For arch foot stability during the feet in the 180° En dehor position, a treatment effect was observed for GPD [X2(2) = 7.538, p = 0.023]. The adjusted Bonferroni test did not identify differences between the pre- and post-intervention periods (p > 0.05 for all).
Regarding arch foot stability during feet in parallel position, a treatment effect was observed for GPD [X2(3) = 9.923, p = 0.019]. However, the adjusted Bonferroni test did not identify difference between pre-intervention and post-intervention (p > 0.05 for all) or between post-intervention and follow-up periods (p > 0.05 for all).
Pelvic position: Regarding the pelvic position during the feet in self-selected En dehor position, a treatment effect was observed for the SK3 [X2(2) = 8.000, p = 0.018]. The Bonferroni test showed fewer occurrences in the highest pelvic scores following the intervention period (p = 0.021) between pre- and post-intervention (p > 0.05 for all). No difference was found between the post-intervention and follow-up periods (p > 0.05 for all).
In the analysis of the feet in 180° En dehor position, no treatment effect was observed and the effect size between the pre- and post-intervention periods was trivial for all the analyzed phases.
This study aimed to determine the effects of an intervention program based on Piret and Beziers' Motor Coordination principles on the knee alignments, foot arch stability and pelvic position in pre-professional ballet dancers. Based on this aim the main findings were the following: (1) An intervention program based on Piret and Beziers Motor Coordination principles results in improved knee center alignment, but has no effect on the foot arch stability or pelvic position; (2) The improved knee alignment was maintained for 24 weeks after the conclusion of the supervised sessions.
Our results support the hypothesis that an intervention program with exercises that emphasize the balance between muscles that perform antagonistic twist actions and the alignment of the lower limbs can be an effective strategy to achieve knee alignment in pre-professional dancers. Some studies suggest that improving knee alignment decreases the risk factors for lower extremity injury in dancers [4-6].
The major novelty of the present study resides in testing the application of an intervention program based on exercises designed to reduce misalignment in the lower limbs though "knee torsional stabilization" [17]. Considering that classical ballet requires dancers to repeatedly adopt the turnout position, which involves extreme lower-limb external rotation, and that to achieve this position, dancers frequently turn the tibia out externally beyond the physiological internal rotation, the exercises selected in this study were focused on achieving knee stabilization and alignment through the application of the Motor Coordination principles (Chart 1). In practical terms, it is believed that the exercises applied in this study, such as Alavanca and Reggae, executed on different surfaces and at different execution speeds, which focused on the dancers' lower-limb torsional organization and on proprioceptive gains, helped the dancers transfer these Motor Coordination principles into the execution of basic ballet movements such as the plié, grand-plié and fondu.
Our results showed that during the control period, when no intervention was performed, no differences in knee alignment were found, but during the intervention period, differences were detected for this criterion in several phases of the plié, demi-plié and grand plié steps. Thus, post-intervention improvements seem to be related to the real effects caused by the tested intervention. The most meaningful result of our study for knee alignment was observed during the feet in the 180° En dehor position, which is considered the most fundamental position in classical ballet. For this position, we found consistent improvements with a medium effect magnitude at two static extended knee phases, where, generally, the participants had increased scores from above or beyond the 1st toe (femur internal rotation) to above the 2nd/3rd toes (knee aligned). In addition, a significant effect with a medium magnitude was also found for the ascent phase of the demi plié and grand plié, where a larger percent change from unstable knee center (starts with internal rotation and ends above or beyond the 1st toe) to stable (starts and ends in the same position) was noted. When the findings of the feet in self-selected position were explored, a larger percentage increase in the highest scores of the knee center in the ascent phase of demi-plié and grand-plié and the descent phase of the demi-plié and fondu was observed after the intervention period. Thus, the fact that the participants presented increased MADAAMI' scores in several phases during the evaluated steps after the intervention period suggests the tested intervention is effective in minimizing the effects of the misalignments resulting from altered movements and can help reduce this important risk factor of lower-limb injury in dancers.
Our results can be attributed to the fact the three types of sessions (supervised, home-based and life sessions) involved the participants actively learning how the nervous system automatically executes aligned body movements to avoid the internal rotation of the femur associated with the exaggerated external rotation of the tibia and the eversion of the subtalar joint during basic ballet steps. In theory, a better afferent somatosensory input coupled with adequate efferent muscle force generation could influence neuromuscular control of the synergist muscles, ultimately improving their function in dancers [24-26]. The central argument given by Piret and Beziers [16] is that the re-education of the antagonism between muscles with opposite actions through exercises could optimize neuromuscular control and proprioceptive function. Future interventional studies and clinical trials are needed to test these hypotheses.
Unfortunately, the evidence for the effectiveness of applying the Motor Coordination principles in the prevention or treatment of lower-limb injury is current circumstancial [16,17]. Previous studies involving areas other than dance provide evidence to show improvement in patients with, for example, patellofemoral syndrome subjected to treatment methods that incorporate physical exercises to correct the biomechanical misalignment, such as dynamic valgus [27,28]. In general, the intervention programs were comprised of exercises that emphasized hip and lumbopelvic stabilization, correction of hip muscle imbalance, biomechanical control and sensory motor training. The results from these studies showed improved joint alignments, pain relief, increased range of motion, strength and motor control gains, in patients with knee injuries. There is an unjustified lack of scientific evidence on the effects of preventive programs that focus on correcting altered movement patterns in ballet dancers. The authors of the present study believe that if the altered movement is repeated, the sequence of compensations leading to microtrauma and macrotrauma progress, producing pain and, eventually, tissue abnormalities [29]. Thus, investigations into the effects of preventive programs on parameters related to movement competency are considered of great value for clinical practice in the dance world.
The fact that no differences in terms of foot arch stabilization were observed was expected because most of the participants had presented the highest scores (stable foot arch) during the phases in the MADAAMI assessment prior to the intervention program. However, we expected our intervention to ameliorate the pelvic stabilization capacity due to the inclusion of exercises focused on trunk stabilization, such as the Frontal and Lateral Plank (Table 1). The objective of these exercises was to challenge the body to activate what Piret and Beziers [16] refer to as the "rectus muscle system" to stabilize the trunk based on the antagonism between the spine flexor (rectus abdominis) and extensor (erectors spinae) muscles. For Piret and Beziers, this stabilizing tension can support any movement demanded of it, such as the torsions performed in the "cross-system dynamic" opposition action, especially by the abdominal oblique muscles [17]. This concept is very important for classical ballet because before spinning around themselves, using their lower limbs as a base, dancers need to stabilize their own trunk in static postures during the teaching-learning-training process [17].
One possible explanation for the lack of changes in the pelvic position is that the effect generated by the intervention was a false negative (Type II error) given that the final sample size was very small (n = 20). Aiming to maintain high levels of quality regarding the execution of the intervention protocol, we decided to exclude all participants that presented poor adherence to intervention sessions from the study. The small sample size is considered a potential limitation of this study, as it reduces the power of our statistical test in determining real differences, given that our sample size calculation determined that 35 subjects achieved a calculated power of 0.80.
It is important to note that the participants could have obtained additional clinical benefits unevaluated in the assessment protocol, such as improvements to the proprioception system. Future studies could use an isokinetic dynamometer to assess the effect of a Motor Coordination principles-based intervention program on proprioception measurements, such as joint position sense [26] and assess the correlation of these effects with the improved alignments. Furthermore, it may be that the proposed MADAAMI protocol classification lacked sufficient sensitivity to detect very small differences in the pelvic position between pre- and post-intervention since the pertinent scoring system has only three differentiated scores, two of which are associated with, hypothetically, more stable positions. However, this hypothesis also requires further study.
Moreover, the absence of a control or sham group might also be considered a study limitation. To minimise this limitation, we used a control period, at least in part of the sample, during which no intervention was used to evaluate the natural variance expected without intervention. Considering that during the control period the participants engaged in a systematic routine of ballet classes according the Bolshoi Theatre School, we decided to assume the observed effect on knee alignment was produced by the intervention protocol, rather than being due to mere coincidence.
As a practical application, the results of the present study demonstrate that when the main goal of the treatment is to promote knee alignment, a preventive intervention based on Motor Coordination principles seems to be effective. It is important to note that moderate knee alignment improvement was found during several phases of the En dehors (feet in self-selected and 180-degree position). Finally, our findings point to an improved knee alignment who does persist beyond supervised sessions, what can be considered an advantage of this approach because dancers can incorporate without difficulties the "life lessons" and the home-based exercises into their ballet classes routine [30].
The intervention was effective to promote knee center alignment, which persisted after 24 weeks, beyond supervised sessions. No effects in the pelvic position or in the foot arch were observed.
Not applicable.
This manuscript was written with equal authors' contributions.