Objective: Open reduction and internal fixation (ORIF) for proximal humeral fractures is said to increase the incidence of osteonecrosis of humeral head. Fact or fiction? Therefore a systematic review was performed, searching multiple databases, online registers of randomized controlled trials (RCTs), and the proceedings of major meetings.
Methods: All RCTs comparing the incidence of osteonecrosis of humeral head between ORIF and conservative treatment were identified. Two authors independently assessed methodological quality and extracted data. Three articles with 149 patients were identified. The odds ratio and 95% confidence intervals were calculated for each study.
Results: Pooled analysis showed that there is no significant increase of the osteonecrosis rate of the humeral head after ORIF compared with that of conservative treatment.
Conclusion: Based on the best available studies, there is no sufficient evidence to support the belief that ORIF can significantly increase the incidence of osteonecrosis of the humeral head.
Level of evidence: Level I.
Proximal humeral fractures, Internal fixation, Osteonecrosis, Meta-analysis
Proximal humeral fractures are account for approximately 4% to 5% of all fractures [1]. They are the third most common fractures after hip and distal radius fractures [2,3]. The incidence of these fractures increases as the population ages, particularly in women [3,4]. These fractures are mostly stable and minimally or nondisplaced osteoporotic fractures. Many patients can regain shoulder function with conservative treatment, and proximately 20% of patients are treated surgically [5].
Open reduction and internal fixation (ORIF), an effective surgery proven by multiple studies, has become increasingly popular for proximal humeral fractures [6-8]. It is partly the result of the advancement in surgical technique, especially locking plate technology for the treatment of fractures in osteoporotic bone, and the fact of the suboptimal functional results of humeral head replacement. However, several complications have been reported, such as infection, nonunion, hardware failure and osteonecrosis [6]. The humeral head is the second most common site of osteonecrosis following the femoral head [9]. Among complications, osteonecrosis considered as a major complication after fractures of the proximal humerus remains a significant source of patient morbidity, often resulting in pain and shoulder dysfunction [10]. Perfusion of the humeral head is, though not the only, an essential consideration when deciding on the treatment of proximal humeral fractures. Therefore, current fracture classification systems of the proximal humeral fractures are mainly based on the probability of development of osteonecrosis [11,12].
As a head-conserving reconstruction of humeral head, ORIF may restore the anatomy of the proximal humerus but may further compromise the vascularity of the head, leading to osteonecrosis and poor outcome. Whether this technique would increase the osteonecrosis rate of humeral head is uncertain [5,6]. However, this information would be helpful for a rational selection of prosthetic replacement, if ORIF was associated with a high risk of osteonecrosis. It could avoid the requirement for prosthetic replacement which might occur following unsuccessful ORIF, complicated osteonecrosis. Therefore, this study performed a meta-analysis of randomized controlled trials (RCTs) concerning whether ORIF would increase osteonecrosis rate of the humeral head.
We searched for all publications (from January 1980 to January 2015), using electronic databases, including Pubmed, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), China National Knowledge Infrastructure (CNKI), Chinese BioMedical Literature Database (CBM), Chinese Medical Current Content (CMCC), Cochrane Central Register of Controlled Trials (CENTRAL), the Cochrane Database of Systematic Reviews, and Cochrane Bone, Joint and Muscle Trauma Group Specialized Register. We also searched for unpublished trials and those in progress using clinical trials repositories, including that of the National Institute of Health, the National Research Register, Current Controlled Trials, Trials Central and archives of abstracts of the annual meetings of the Orthopaedic Trauma Association, the American Academy of Orthopaedic Surgeons, and the Canadian Orthopaedic Association.
The search strategy first used Mesh terms ("Humerus" (Mesh) OR "Humeral Fractures" (Mesh)) AND type of clinical trial (Randomized controlled trial and Clinical trial) and then a secondary free search was performed using multiple key words (humer* and fractur* and random*) to ensure inclusion all possible studies. We conducted the search in duplicate (WL, ZJ) and independently, with no restriction on language or publication status. The abstract of any study that was potentially relevant to the topic was reviewed. The full text was obtained if inadequate information was acquired from the abstract. Disagreements were resolved by discussion, and a third reviewer (DR) was consulted for the final decision when necessary. Relevant reviews regarding proximal humeral fractures were examined for potential trials.
We conducted and reported this meta-analysis according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) Statement [13].
The eligible articles should meet the following inclusion criteria: (1) Patients aged 18 years or over with proximal humeral fractures; (2) ORIF versus conservative treatment; (3) Outcome measure was osteonecrosis of the humeral head; (4) Published or unpublished, prospective and RCTs. This review excluded studies focused on the treatment of skeletally immature individuals, delayed union, nonunion or pathological fractures.
For each eligible study, two reviewers (WL, ZJ) independently extracted data with the use of a standardized data recording form, and disagreements were resolved by discussion and, if necessary, by means of scrutiny by a third reviewer (DR). Information extracted included population demographics, year of publication, fracture type, number of patient, trial duration, treatment method and number of osteonecrosis. Authors were contacted if information could not be obtained from the original literature.
Two reviewers (WL, ZJ) independently assessed the methodological quality of each included study with use of the modified Jadad score [14]. This is an eight-item score designed to assess randomization, blinding, withdrawals and dropouts, inclusion and exclusion criteria, adverse effects and statistical analysis (Table 1). The score for each article could range from 0 (lowest quality) to 8 (highest quality). Scores of 4-8 denote good to excellent quality and 0-3 poor to low quality. Disagreement was resolved by means of discussion, with arbitration by a third reviewer (DR).
Table 1: Eight-item modified Jadad score. View Table 1
The statistical analysis was conducted using Review Manager 5.0 software (The Nordic Cochrane Centre, the Cochrane Collaboration, 2008, Copenhagen, Denmark). Heterogeneity between studies was tested with use of both the chi-square (χ2) test and the I-squared (I2) test [15]. Statistical heterogeneity was considered significant when p < 0.10 for the χ2 test or I2 > 50%. A fixed effects model was used if there was no evidence of heterogeneity between studies; if there was evidence of heterogeneity, a random effects model was used for the meta-analysis. The odds ratio (OR) and 95% confidence intervals (CI) were calculated for each trial and presented in a forest plot. Sensitivity analysis was performed by excluding low modified Jadad score studies (< 4 points), if necessary. All reported P values were two-sided and P < 0.05 were regarded as statistically significant.
Figure 1 illustrates the study flow. A total of 3 studies [16-18] included 149 patients met our inclusion criteria, and one study [19] were excluded for no relevant outcome reported. A total of 75 patients were treated by ORIF, and 74 patients were treated conservatively.
 Figure 1: The flowchart.
View Figure 1
Figure 1: The flowchart.
View Figure 1
All included studies were RCTs that enrolled patients with complex displaced proximal humeral fractures, including three- and four-part fractures. All ORIF was performed using a delto-pectoral approach. Internal fixation was accomplished with plate as the operative technique in 2 studies [16,17], and with tension-band surgery in 1 study [18]. The patients in the included studies were predominately old (mean age range from 72.2 to 75 years) and female (85.2%) patients. Other detailed information from each study was list in Table 2.
Table 2: General information of included studies. View Table 2
All included studies reported osteonecrosis of the humeral head as one of the outcomes. The overall osteonecrosis ratio was 16% for the ORIF group (12/75) compared to 20.3% in the conservative group (15/74). The test for heterogeneity was not statistically significant (χ2 = 2.13, I2 = 6% and p = 0.35), which indicates that the pooling of the data was valid. Analysis showed that there was no significant difference between ORIF and conservative treatment (OR = 0.72, 95% CI = 0.29 to 1.77, p = 0.48) (Figure 2).
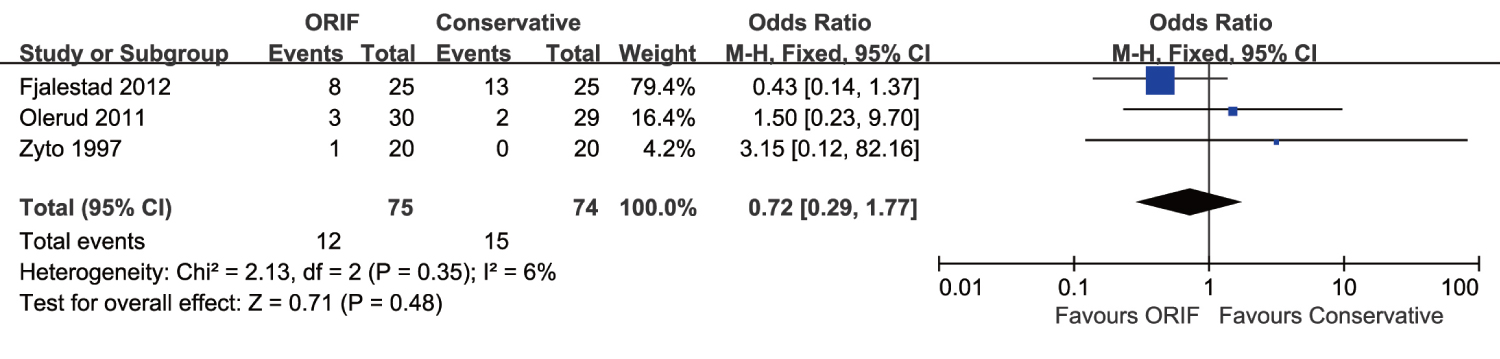 Figure 2: Incidence of osteonecrosis of the humeral head.
View Figure 2
Figure 2: Incidence of osteonecrosis of the humeral head.
View Figure 2
According to the best available evidence, this meta-analysis suggests that there is no significant difference in the osteonecrosis rate of the humeral head after ORIF for proximal humeral fractures compared with conservative treatment.
Osteonecrosis rate varied greatly has been reported from 0% to 37% of patients after ORIF with proximal humeral fractures [20,21]. In this study, osteonecrosis rate in ORIF group is 16%, which is similar to previous articles [7,8]. ORIF is associated with a lower incidence of osteonecrosis compared with conservative treatment, but there was no significant difference.
There are several reasons for the osteonecrosis of humeral head. First, the severe injury resulted in the disruption of the arteries is related to the risk of osteonecrosis. Four-part fractures usually have higher rates of osteonecrosis than three-part fractures, varying from 15%-30% [9,22]. It may be an inevitable complication of an injury because of disruption of the blood supply of the humeral head [9,16]. The arterial supply of the proximal humerus is derived from the anterior circumflex humeral artery and posterior circumflex humeral artery. The anterior circumflex artery, arising from the axillary artery, courses laterally under the tendon of the long head of the biceps and terminates with smaller branches in the greater tuberosity. The arcuate artery arises from the anterolateral branch of the anterior circumflex and ascends proximally into the humeral head, acting as its major intraosseous supply. The lesser tuberosity also receives blood from the anterolateral branch. The posterior circumflex humeral artery travels posteriorly along the medial aspect of the surgical neck, sending branches to supply the posterior portion of the greater tuberosity and a small posteroinferior part of the head [23]. Most of proximal humeral fractures can disrupt the anterior humeral circumflex artery. After injury to this main blood supply, the posterior circumflex artery is believed to provide additional blood flow to the humeral head [24]. Second, the time of surgery is one of the important factors. Earlier surgery may help to the earlier reduction the fractures, which is beneficial for the bone healing [9,17]. Third, corticosteroid therapy is the most commonly reported cause of nontraumatic osteonecrosis [9,16,17]. The underlying disease for which the corticosteroid is administrated may be involved in the pathogenesis of osteonecrosis. In addition, several hemogloblinopathies are common causes of osteonecrosis, especially sickle-cell disease [9]. Therefore, patient with some comorbidities should be further assessed for the humeral head.
Osteonecrosis may also be the result of treatment, which may be to the result of either procedure selection or in the surgery provided. Use of a minimally invasive approach likely reduces the risk of osteonecrosis, so limited exposure or percutaneous technique is performed in the included studies to reduce blood supply disruption of the humeral head. Moreover, the delto-pectoral approach reported in the included studies is generally used to treatment proximal fractures. Base on the meta-analysis, there is no evidence to support ORIF in this approach can influence the outcome of humeral head. This traditional approach may require more dissection and retraction to access the lateral humerus increasing the potential for vascular insult. The anterolateral approach provides direct access to the lateral humeral bald spot obviating the need for circumferential dissection and potential vascular disruption either anteriorly or posteriorly [25]. Fracture manipulation and implant insertion can be performed directly through the lateral fracture lines. Additionally, it is demonstrated that there is a trend toward increased osteonecrosis in the delto-pectoral approach compared with the anterolateral deltoid split [26]. So ORIF in anterlateral approach is a possible option which may further reduce the incidence of osteonecrosis.
The quality of fixation may contribute to reduce the occurrence of osteonecrosis. In cases where the blood supply is compromised, ORIF may restore the anatomy of the proximal humerus and keep the reduction, reducing additional disruption of the blood supply and making revascularization possible. For traditional plating has been associated with a high rate of complications, the site-specific locking plate technology has been used to the proximal humerus. This new plate technology provides more secure fixation in osteoporotic bone, reducing the risk of fixation failure and show benefit over conventional plate fixation [6]. Additionally, Initial ischemia of humeral head after proximal humeral fracture does not necessarily lead to the osteonecrosis, indicating that revascularization may indeed occur [27]. ORIF can provide adequate reduction and stable conditions for revascularization and make the preservation of the humeral head viable. Therefore, ORIF with minimal soft tissue disruption while establishing rigid fixation of the fracture may provide a predictable method to reduce the long-term incidence of osteonecrosis even when treating at risk fracture types.
Although many surgeons believe that ORIF might increase the incidence of osteonecrosis of humeral head, little clinical information is currently available on this topic. In this meta-analysis, we conduct a comprehensive literature search to include all available evidence, and do data extraction and methodological assessments in duplicate, and make conclusions based only on high-quality RCTs. However, our study has several potential limitations. Our best efforts in using multiple search strategy and available database, but publication bias may be unavoidable in this meta-analysis. The included studies have some limitations, including small sample sizes, incomplete reporting of treatment allocation concealment and no possibility of blinding patients and physicians. Additionally, the low number of included studies limits our ability to make more definitive conclusion.
In conclusion, this meta-analysis of randomized controlled trials suggests that ORIF for proximal humeral fractures could not significantly increase the incidence of osteonecrosis of humeral head. Accurate decision-making and improved surgical technique would help to optimize the outcome and reliably avoid this complication even in fractures traditionally considered at high risk for osteonecrosis obviating the need for joint replacement. However, the limitations of the available studies indicate the planning and performance of sufficiently sized, methodologically sound studies. The result should be interpreted with caution and comprehensive until confirmed by large, definitive randomized controlled trials.
We declare that we have no conflicts of interest.
WL and SZ: Design issue; WL and LC: Wrote the paper draft; WL, LC, DG and SZ: Collect, analyze the data and revised the paper.