Idiopathic Inflammatory Myopathies (IIM) are considered to be multisystemic diseases that commonly present as muscle weakness and myalgia [1]. Currently, there are no reports of hip or sacral fractures that result as a complication of IIM, despite evidence of increased falls risk in these cases due to commonly reported lower extremity proximal muscle weakness and myalgias [1]. There is limited data on ethnic variability as it relates to IIM and its sequelae.
The incidence of fracture has not been reported commonly in the literature, however de Andrade, et al., suggest increased fracture risk amongst middle aged-women who suffer from inflammatory myopathies such as Polymyositis and Dermatomyositis [2]. This finding is further supported by Gupta, et al., who found asymptomatic vertebral fractures were much more common in patients with inflammatory myopathy versus healthy controls, even in individuals who were not on long-term glucocorticoid therapy [3]. To date, there is a lack of literature that reflects the occurrence of fractures and associated complications amongst diverse populations with IIM.
This case highlights a middle-aged black woman, who upon initial presentation to the emergency department reported low back pain with an inability to ambulate after a mechanical fall and was found to have a sacral fracture.
Fracture, Myositis, Inflammatory myopathy, Sacral fracture, Case report
A 54-year-old African American Female presented to the ED reporting a fall after slipping on water with initial CT images of her pelvis showing a minimally displaced right sacral fracture (Figure 1 and Figure 2). The right anterior superior iliac spine changes seen on CT were previously noted on imaging from a different hospitalization. She had both an elevated Creatine Kinase (CK) (2758 U/L) and AST (411 IU/L) level. The patient was admitted for observation for 24 hours to have Orthopedic Surgery further evaluate the imaging and quality of the fracture. On further questioning of the patient, she mentioned multiple falls over the past 1-2 years requiring ED visits for fractures of various regions of her body including: right radius, left ankle, and multiple left ribs (sixth-ninth and eleventh). She reported an associated generalized weakness throughout her body, especially of her lower extremities which would lead to the falls. She reports these episodes of weakness are accompanied by pain, last for 1-2 weeks, and then self-resolve. She has noticed these episodes with stress and most recently, after a heated disagreement with a family member. On initial examination of the patient, in addition to sacral pain, she had a slightly erythematous rash around her eyes (images not available), hypopigmentation of her digits and toes, with reddish-violet colored patches over her knees (images not available), as well as macules over her metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints (Figure 3a, Figure 3b, Figure 3c and Figure 3d).
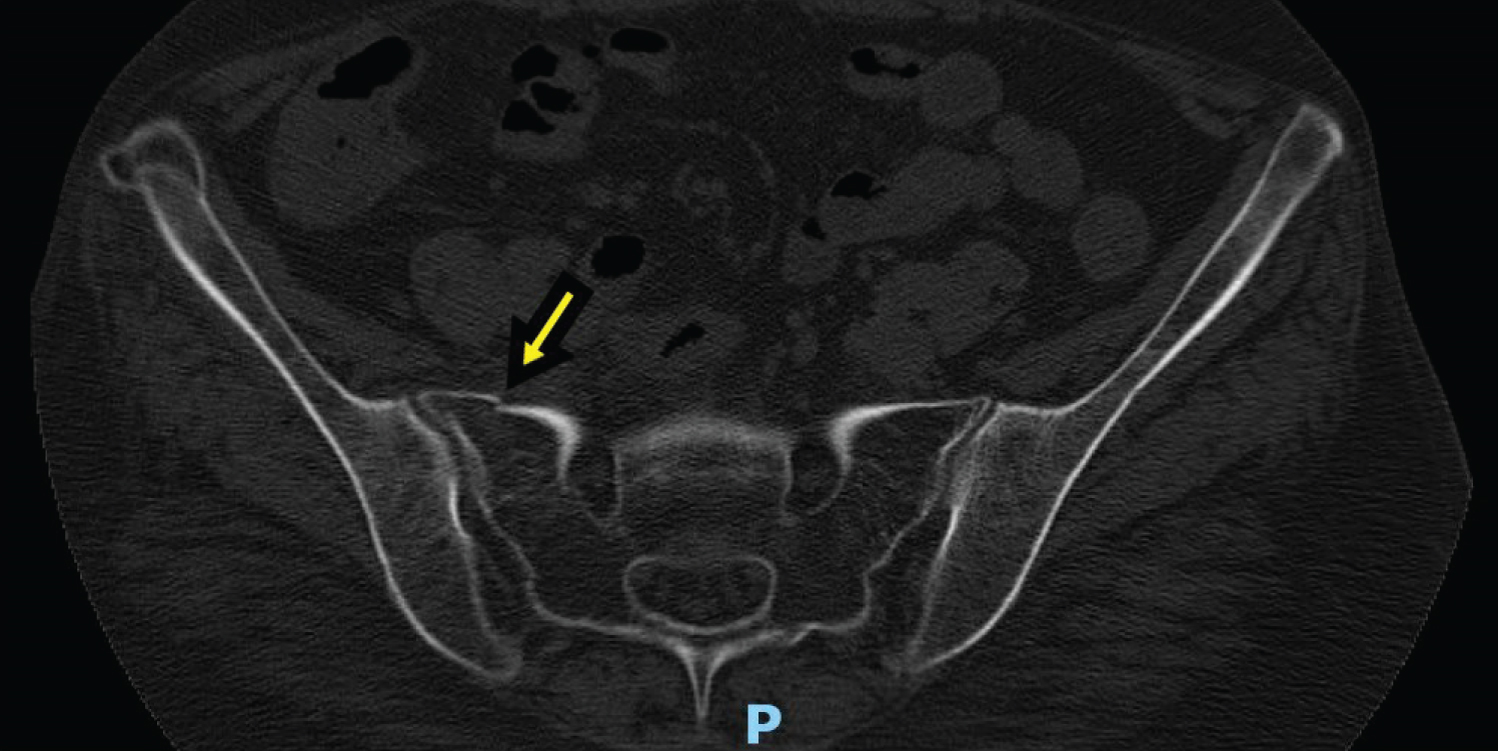 Figure 1: CT pelvis w/o contrast [Transverse View] - Inferior right pelvis partially displaced fracture 1 of 2.
View Figure 1
Figure 1: CT pelvis w/o contrast [Transverse View] - Inferior right pelvis partially displaced fracture 1 of 2.
View Figure 1
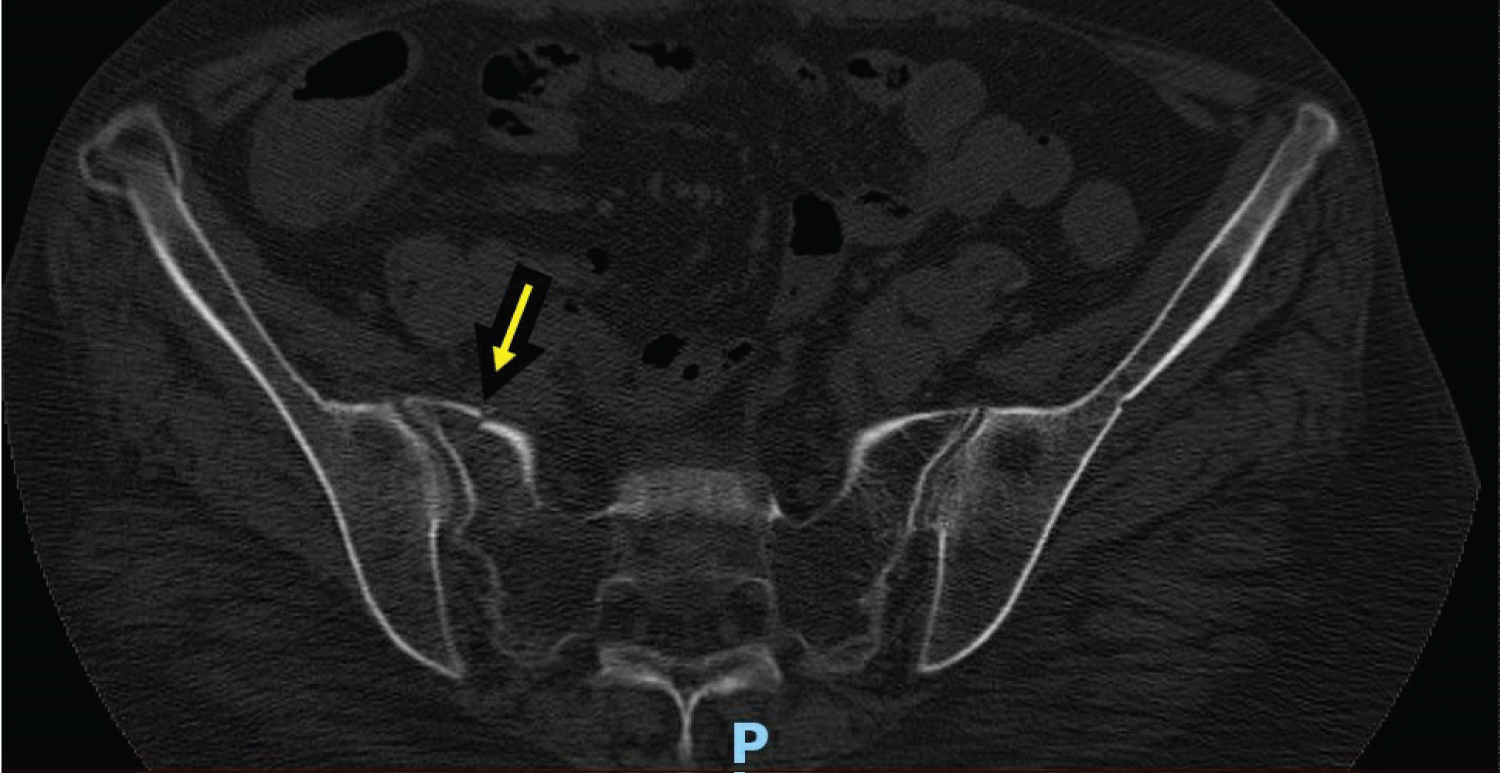 Figure 2: CT pelvis w/o contrast [Transverse View] - Inferior right pelvis partially displaced fracture 2 of 2.
View Figure 2
Figure 2: CT pelvis w/o contrast [Transverse View] - Inferior right pelvis partially displaced fracture 2 of 2.
View Figure 2
 Figure 3: Photo images of patient's upper and lower extremities showing non-specific hypo- and hyper- pigmentation with nodular appearing changes around MCP/PIP joints in (a) and (b). Hypo/hyper pigmentation of feet bilaterally (c) and (d).
View Figure 3
Figure 3: Photo images of patient's upper and lower extremities showing non-specific hypo- and hyper- pigmentation with nodular appearing changes around MCP/PIP joints in (a) and (b). Hypo/hyper pigmentation of feet bilaterally (c) and (d).
View Figure 3
Based on the physical exam findings and history by the primary family medicine team, the patient was admitted to the floor for further work-up. Her pain was managed with the following pain regimen: IV Morphine as needed which was de-escalated after five days to PO Tramadol 25 mg q4 hrs as needed with Tizanidine 2 mg q6 hrs as needed for muscle spasms. Upon review of the patient's records from prior hospitalization, it was discovered that she had undergone a muscle biopsy within the past two months.
The biopsy findings from the outside hospital showed necrotizing inflammatory infiltration of T-cells into her myocytes. The records further confirmed a history of skin changes along the bony prominences, marked elevations of her CK with recurrent episodes of weakness and falls, and a prior ANA + test (1:160 titer). In light of her clinical course, combined with this new information, there was concern for Dermatomyositis and Dermatomyositis-related diagnoses.
A few days into her admission, she began to have diarrhea along with increased myalgia and myopathy of bilateral upper and lower extremities. Repeat CK levels at that time were > 100,000 U/L, despite continuous intravenous (IV) fluids. At this point, the patient was started on Prednisone 60 mg daily. This led to a significant decrease in her myopathy with improved ambulation and decreased weakness. Her clinical picture improved, and the patient was discharged with an appointment for Rheumatology follow-up to further evaluate her suspected Dermatomyositis and manage the condition moving forward (Table 1).
Table 1: Creatine Kinase (CK) daily trend over 12-day hospital course. View Table 1
Our patient was appropriately treated with pain control, physical therapy and standard high-dose glucocorticoid therapy and was discharged to a skilled nursing facility to help with rehabilitation. It is important to mention that there is evidence showing an independent risk between inflammatory myopathy and bone fracture, and this information was shared with the patient [2,3]. In patients with Polymyositis/Dermatomyositis (PM/DM), 17.5% reported fractures of the distal forearm, humerus, femoral neck and ribs, compared to 3.85% in the control group [4]. The cause for this mechanism is not well understood but thought to be associated with the inflammatory process that makes individuals more susceptible to osteoporosis and insufficiency fractures [5,6].
Stress fractures (including insufficiency type) occur in 1% of the general population and most commonly affects lower extremity structures, such as the pelvis [7]. Cuadros, et al., suggests that insufficiency fractures are related to immunologic disease processes, post-menopausal changes, and other risk factors [6]. We suggest that post-menopausal patients with idiopathic inflammatory myopathy and a concerning history, should be counseled about these potential risks as in our case.
Of note, since our patient's discharge from the hospital, she has had further evaluation and assessment by Rheumatology and Neurology who recently completed EMG study confirming myopathic disease.
There are no competing interests for any of the involved authors or faculty members in production of this case report. All authors listed above contributed equally in production of this manuscript.
Munish Bakshi, MD (Faculty Advisor)
Kaitlin O'Malley, MD PGY-2
Samar Haroun, MD PGY-1