There is still lack of rigorous evaluation and evidence for Low-Back Pain (LBP) apps. The objectives of this study were to develop and evaluate the feasibility of a mobile phone-based app of Mechanical Diagnosis and Therapy (MDT) extension exercise; and to examine the correlation between app rating parameters and pain characteristics of patients with non-specific LBP.
A LBP Self-care Mobile-phone App (LBP-SMA) of MDT plus back hygiene was developed following standard iteration and prototyping process. Feasibility of the LBP-SMA was tested in terms of usability, satisfaction and user's experience using the system usability scale and mobile application rating scale. Quadruple visual analogue scale was used to assess pain intensity of the participants. Data was analyzed using descriptive and inferential statistics at alpha level set at 0.05.
Participants' mean age and pain intensity was 33.8 ± 8.72 years and 45.3 ± 7.23. On a unified scale of 20, functionality (18.5 ± 1.704) and engagement (17.1 ± 2.963) had highest and least objective quality rating on the LBP-SMA. Total objective and subjective quality rating of the app was 17.9 ± 1.471 and 18.4 ± 1.173 respectively. LBP-SMA total impact and usability score was 27.2 ± 1.911 indicating high impact and 29.6 ± 1.95 indicating moderate usability. Participants reported that LBP-SMA mostly affects happiness/wellbeing (37.1%), leads to increased behavioural change (48.6%) and targets physical health (100%). There was no significant correlation between participants' pain characteristics and app rating parameters (p > 0.05).
The LBP-SMA has moderate to high usability, functionality, aesthetics and quality rating, and may serve as an effective mobile-app for self-management of long-term LBP.
Low-back pain, McKenzie extension, Mobile-app, Back hygiene, User-experience
Low-Back Pain (LBP) is a major global public health problem and it is ranked sixth in terms of overall burden of disability with a global point prevalence of 9.4% [1]. LBP results in significant socio-economic toll [2] as it is the leading cause of absenteeism in all professions [3], physician visits [4] as well as physical therapy consultations and workload [5]. Many patients with short-term (acute), intermediate (sub-acute) and long-term (chronic) LBP improve with conservative care and may not need operative interventions like surgeries [6]. However, long-term LBP is more resistant and defiant to interventions and it is one of the most common reasons for seeking physical therapy [7].
Physical therapy is a leading conservative approach for LBP management with substantial literature on its effectiveness [8,9]. Literature is replete on physical therapy armamentarium for LBP which are not limited to electrotherapy, manual therapy and therapeutic exercise [10]. Still, the most effective physical therapy intervention for LBP is still a subject of debate and front burner issue in research [11]. However, exercise is recommended in systematic reviews as the mainstay therapy for LBP [9] thus leading to a proliferation of different exercise approaches with varying results [12]. In addition, variability in exercise design and dependency on skills of the therapists for best results constitutes methodological problems that affect research results on exercise interventions in LBP [13]. The quest for most effective exercise intervention has heralded the concept of patient sub-grouping for exercise in order to achieve maximum benefit [14]. Thus, sub-grouping of patients with LBP in accordance with their signs and symptoms for treatment prescription is considered as an important advance in LBP care [14].
One of the more commonly used methods of sub-grouping amongst physical therapists is the McKenzie principle [15]. This principle is a popular classification-based treatment for LBP among physical therapists [16] with documented effectiveness in some studies [17,18]. However, there is a strong association between certification in the McKenzie Mechanical Diagnosis and Therapy (MDT) to obtain best results [19] which constitutes a potential limitation to providing access for patients who may not have certified MDT faculties and facilities for care. Use of electronically-based exercise platforms represents a superior method for management of patients [20,21]. Advancements in technology now provide new platform and paradigm to care for patients with LBP [22]. For example, smart-phone software provides a novel approach to encouraging home and on-the-go rehabilitation and health promotion [23] because the data storage and processing power of handsets enable real-time intervention [24].
Thus, advent of technology in health had brought about new concepts such as Telerehabilitation [14]. Telerehabilitation has potential to bridge service delivery gap especially in geographically remote areas with shortage of services and lack of access to physical therapy rehabilitation services [25] as well as eliminate barriers of distance, time and travel to receive care [26]. New technologies such as smart-phone application in physical therapy offer a potential means of enhancing patient engagement in usual care or traditional therapy [27]. While mobile technology will not completely replace the traditional face-to-face clinical interaction and interventions, there is modest evidence of the effectiveness and cost-effectiveness of telerehabilitation in pain management [28]. A significant shortcoming of the most of the commercial mobile applications for pain management is that they rarely adhere to estab¬lished guidelines or to scientifically proven concepts. The use of mobile applications by Health Care Professionals (HCPs) has transformed many aspects of clinical practice [29], leading to rapid growth in the development of medical and paramedical software applications [30,31]. Currently, mobile applications are being used to promote health and wellness [32]. Bacigalupo, et al. [33] submit that the use of digital mobile technologies in health care is on increase, however, there is an apparent dearth of studies on the use of MDT on telerehabilitation platforms such as a smart-phone application. Therefore, the aim of this study was to develop and assess the feasibility of a mobile phone-based application of the MDT in patients with long-term non-specific LBP.
Patients with LBP attending the physiotherapy department of a tertiary health institution in Nigeria were consecutively recruited into this study. Eligible participants were individuals with long-term (not less than 3 months) LBP with unknown aetiology (non-specific). They were users of smart/android phone with operating system of 3.5 who could respond to mobile software app instructions and commands. Excluded from this study were patients with serious spinal pathology (such as tumors) or any obvious spinal deformity or neurological disease; patients with a positive history of cardiovascular disease contra-indicated to exercise; or individuals who were with elevated blood pressure (> 140/90 mmHg); patients who were pregnant or have had a previous back surgery; patients with previous experience of the McKenzie therapy; and patients who had directional preference for flexion or no directional preference based on the McKenzie Assessment. Based on a Gang sample size formula [34], a total of 35 participants were recruitment for this study.
1. Smart phone or android phone with Operating System of 4.0 was required for the installation of the mobile apps.
2. System Usability Scale (SUS) - This was used to assess user experience in terms of usability, satisfaction, level of motivation, and complexity of the app based therapeutic tasks for LBP. (ISO 9241-210 defines user experience as "a person's perceptions and responses that result from the use or anticipated use of a product, system or service). The SUS presented 10 statements about the perceived usability of the game. Patients could indicate on a scale of 0-4 to what extent the presented statements were true for them. To obtain the final SUS score, the sum of the patients' answers was multiplied by 2.5. The SUS score ranges from 0 (low usability) to 100 (high usability) [35].
3. Mobile App Rating Scale (MARS) - This is a reliable multidimensional scale for classifying and rating the information quality of mobile app [36]. This scale was used to rate and compare the video-and-animation based mobile apps.
4. Quadruple Visual Analogue Scale (QVAS) - This scale was used to assess pain intensity experienced by the participants at the time of assessment, typical or average pain, pain at its best and pain at its worst respectively [37]. The scores of current, average and pain at its worst are averaged and then multiplied by 10 to yield a score from zero to 100. The final score is then categorized as "low-intensity" (pain < 50) or "high-intensity" (pain > 50).
Development of the Low-Back Pain Self-care Mobile-phone Application (LBP-SMA) in this study followed the iteration and prototyping process described by Naji [38]. The exercise described in the App were based on the MDT extension exercise [15,39]. The App development process followed 12 major steps including:
Step 1- Defining the goal of the app - To develop a mobile phone-based App based on the MDT extension exercise for patients with long-term non-specific LBP.
Step 2- Wire framing with experts on mobile App development and clinicians - The clinicians involved in the study provided visual description of the intended App, the technical developer in turn designed the schematic blueprint that represents the skeletal framework of the proposed App. Key functionalities of the proposed app were identified prior to actual development.
Step 3- Appraisal of strengths and flaws of the available apps from app store and Google play.
Step 4- Story-mapping and gathering requirements which involves visualization of how to achieve the goal of developing a more user-focused app.
Step 5- Define user scenarios - This stage involves ascertaining a good user scenario which includes checking if the app is working according to developer's defined goal.
Step 6- Update requirements - This stage involves testing, identifying problems and making changes to make the app more natural, individualized and instinctive.
Step 7- Prototyping the app by incorporating stakeholders' observations. In this stage, scenarios previously hypothesized were tested against existing wireframe.
Step 8- Testing of prototype on various mobile phones. The testing exposed bugs and revealed redundant design elements that were almost unnoticed. Consequently, the prototype was adopted to run on smartphones or android mobile phones with Operating System of 3.5.
Step 9- Validation requirements - At this stage of the app development, the prototype was checked with stakeholders before moving on to code.
Step 10- Laying the groundwork for the developed app. At this stage, the idea of the app was refined based on its functionality and the technical specification on what type of smart or android phone on which the app will run was determined.
Step 11- User Interface skins and cycle feedback. The user interface skin of the app was designed based on stakeholders' comments. At this stage, the prototype screen was improved to a high-fidelity skin (Figure 1 and Figure 2).
 Figure 1 and 2: User interface skins and cycle feedback of the low-back pain self-care mobile-phone application.
View Figure 1 and 2
Figure 1 and 2: User interface skins and cycle feedback of the low-back pain self-care mobile-phone application.
View Figure 1 and 2
Step 12- User testing. As the closing stage of the app development, the prototype (dummy) was transitioned to a fully functional app with customized user interface elements. Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6 and Figure 7 shows some of the images of the low-back pain self-care mobile-phone application.
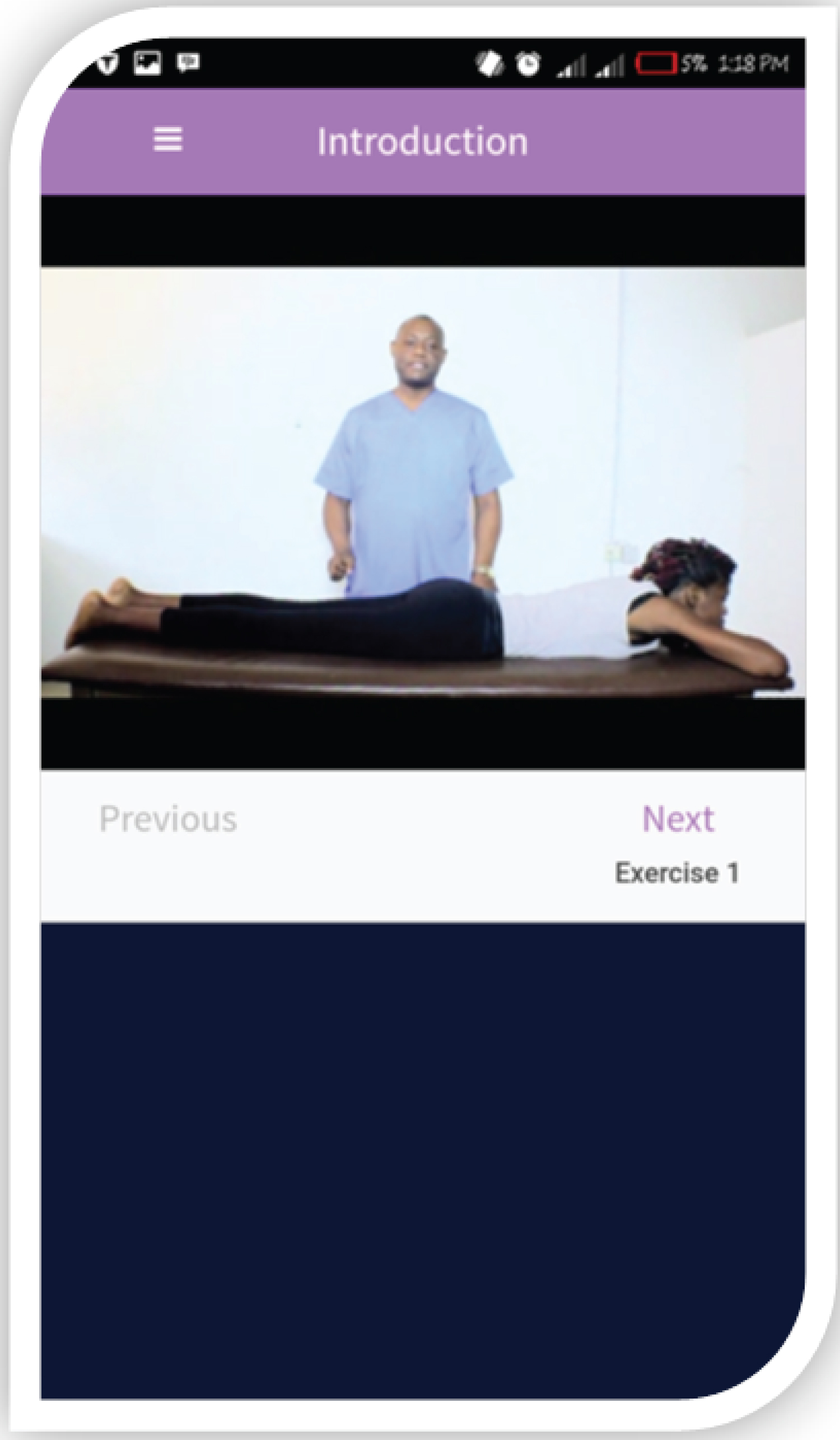 Figure 3: Introduction.
View Figure 3
Figure 3: Introduction.
View Figure 3
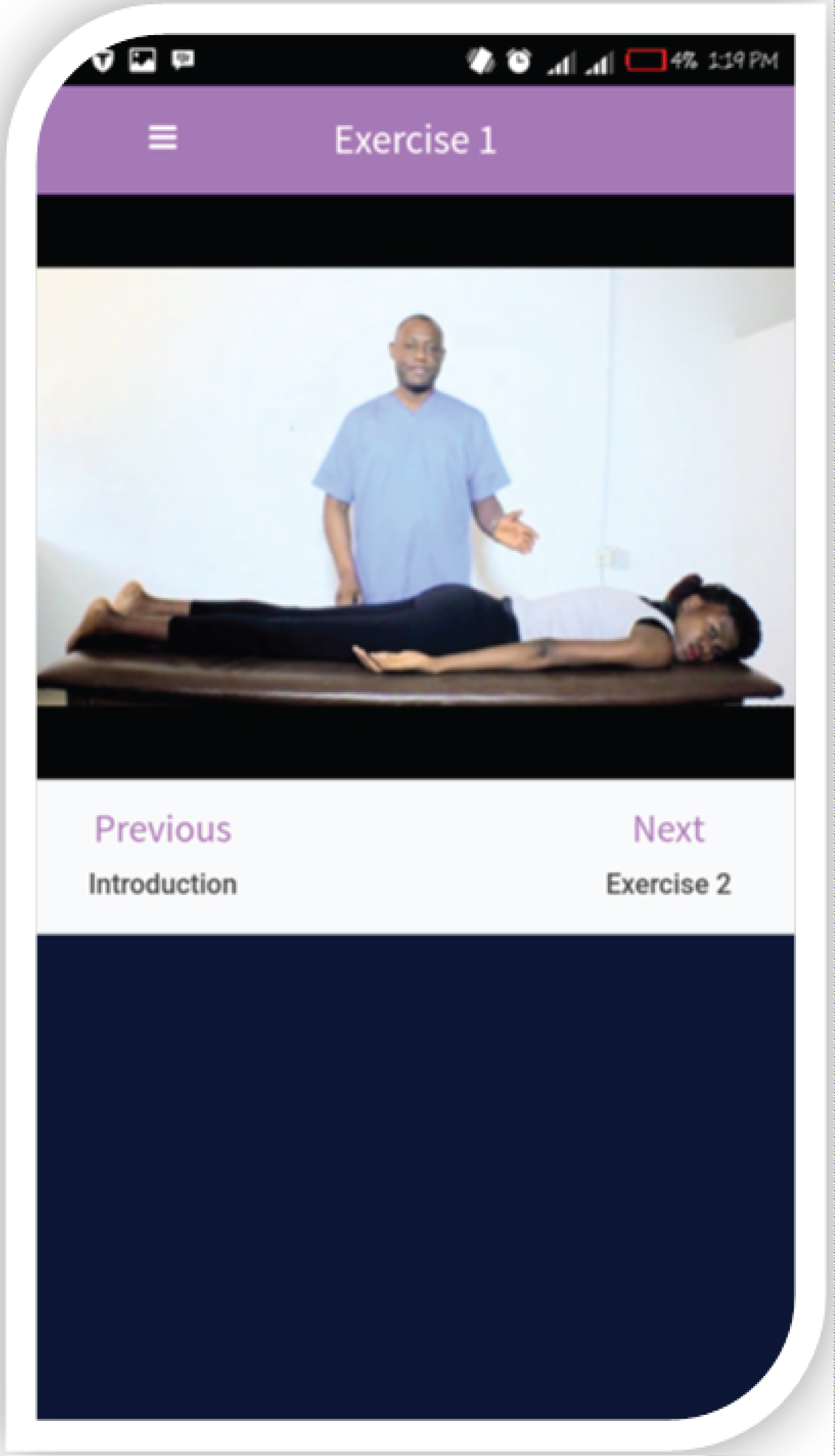 Figure 4: Exercise 1.
View Figure 4
Figure 4: Exercise 1.
View Figure 4
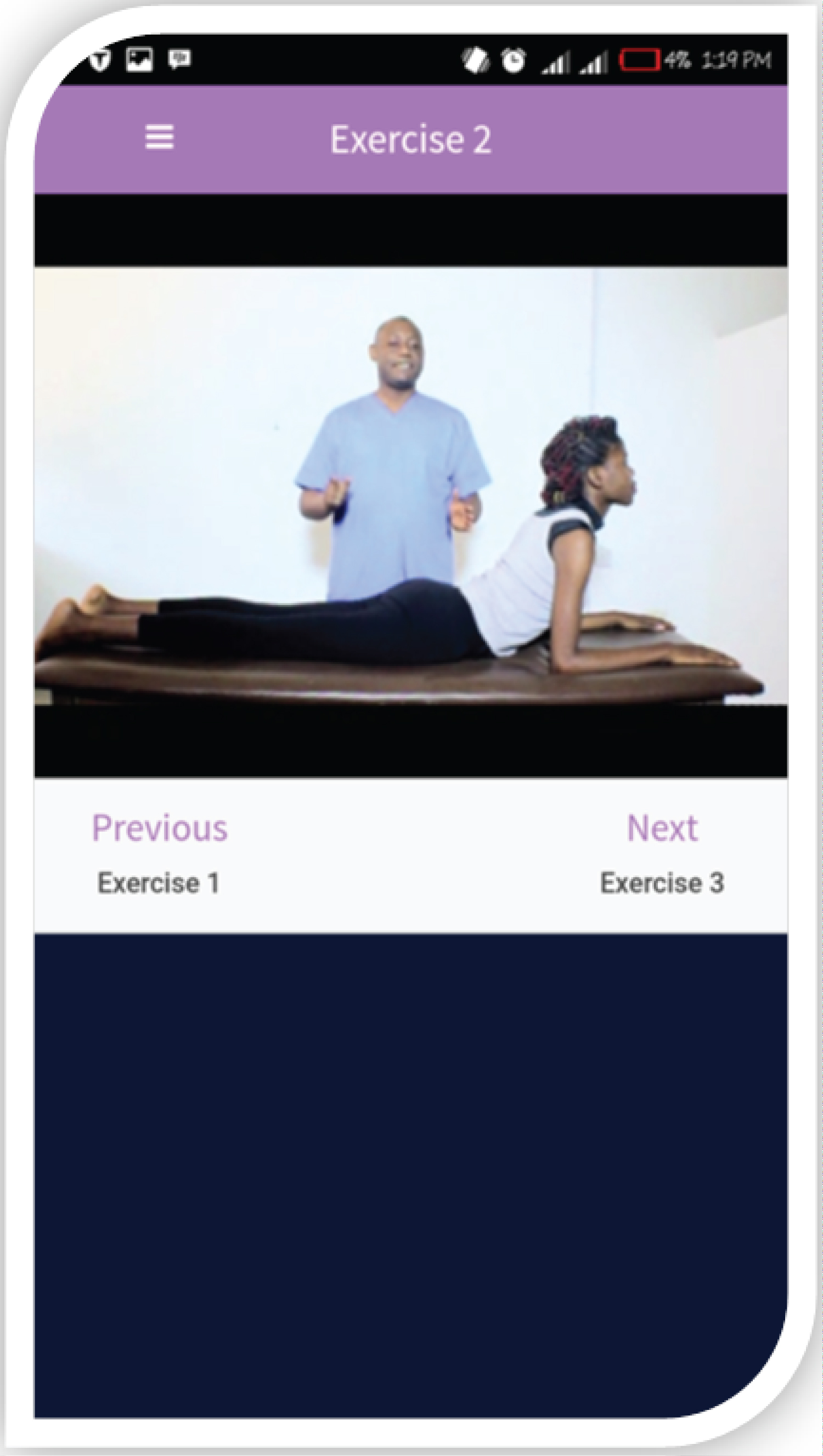 Figure 5: Exercise 2.
View Figure 5
Figure 5: Exercise 2.
View Figure 5
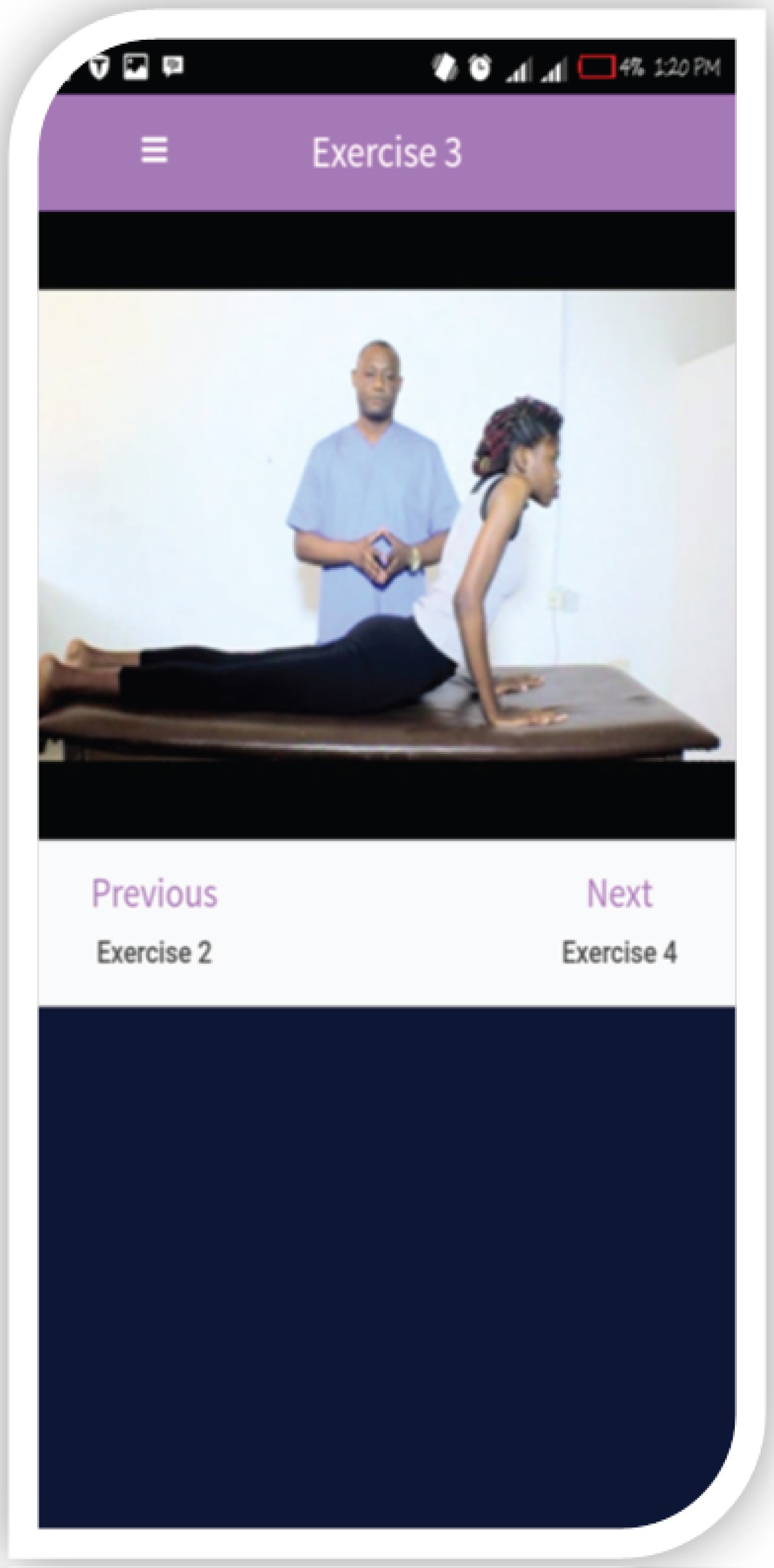 Figure 6: Exercise 3.
View Figure 6
Figure 6: Exercise 3.
View Figure 6
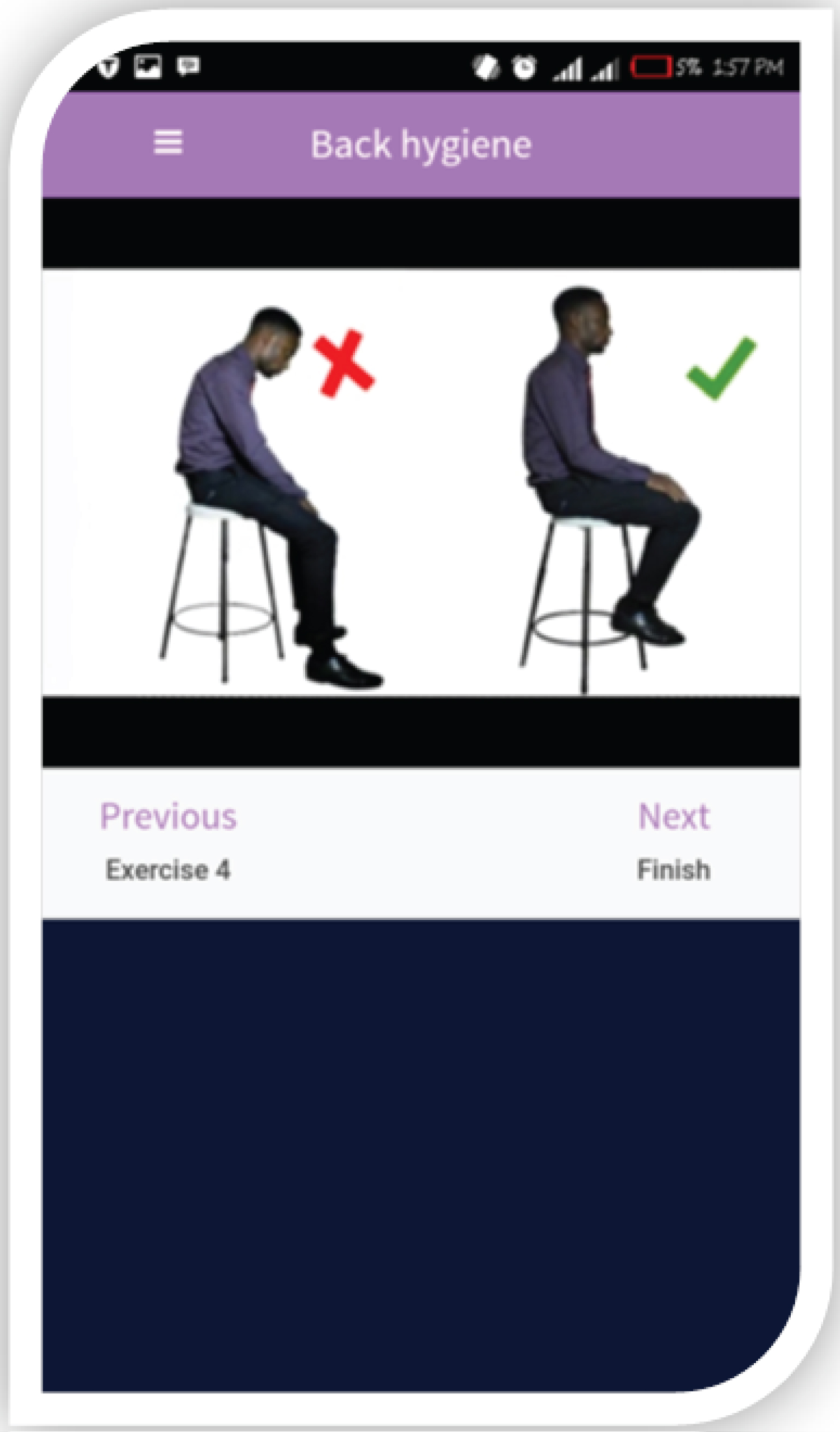 Figure 7: Back hygiene.
View Figure 7
Figure 7: Back hygiene.
View Figure 7
The development of the app involved professional video recording using HC-V770 Panasonic camera with high Lens system that gave High Dynamic Range (HRD) video capture of the various exercises. The consenting models for the development of the app include a physiotherapist who volunteered as instructor, an athlete who modeled as patient, and some undergraduate physiotherapy students who volunteered for photo shots for the mobile app podcasts. Audacity audio editing software was used in the audio recording and editing of the app. The background noise was eliminated and audio tracks were perfectly edited to give a quality output that was exported with the video. The developed App can be viewed through this link:
(https://drive.google.com/file/d/1KnfKSIsDKF_QsKjULimXzP2hPxTWAb4R/view?usp=drivesdk).
Ethical approval for the study was obtained from the Health Research Ethics Committee of the Institute of Public Health, Obafemi Awolowo University, Ile-Ife, Nigeria. Participants' weight and height were measured using standard protocols and their body mass index was calculated. Participants performed the McKenzie back extension protocol and back hygiene portrayed in the mobile app. The protocol involved a sequence of specific lumbosacral repetitive movements in extension that caused the symptoms to centralize, reduce or obliterate [39]. Specifically, the protocol includes repeated extension activities in prone lying and standing respectively [15,39]. Directional Preference (DP) guidelines, based on MDT extension protocol, were used to determine suitability of the patients to participate in the study. The details of the protocol portrayed in the app have been published in our earlier studies [40,41]. Quadruple Visual Analogue Scale (QVAS) was used to assess pain characteristics of the participants. The QVAS assessed current, average, best pain and worst pain respectively. Thereafter, the mode of use of the mobile app was introduced to the participants, and they were asked to perform the therapeutic activities portrayed in the app for a period of one week. Afterwards, the Mobile Application Rating Scale (MARS) and the System Usability Scale (SUS) were administered to the participants. MARS was used to assess the app's quality, aesthetics, engagement, functionality and users' experienced, while SUS assessed the app's usability.
Descriptive statistics of frequency, mean and standard deviation were used to summarize data. Independent t-test was used to evaluate mean differences in participants' general and pain characteristics while Pearson moment correlation were used to analyze the relationship between pain characteristics of the participants and the different rating scores of the LBP-SMA. The data analyses were carried out using SPSS 20.0 version software (SPSS Inc., Chicago, Illinois, USA). Alpha level was set at p ≤ 0.05.
The result of the general and pain characteristics of the participants is presented in Table 1. The mean age, weight, height and BMI of the participants was 33.8 ± 8.72 years, 71.0 ± 7.51 Kg, 1.66 ± 0.08 m and 25.8 ± 2.44 Kg/m2 respectively. The mean current pain of the participants was 4.0 ± 0.98 out of a total score of 10. Based on the Quadruple visual analog scale, the total pain score (derived from current pain, average pain, best pain and worst pain) was 45.3 ± 7.23. Participants' response on perception on the area of focus of the LBP-SMA is presented in Table 2. Participants reported submit that the LBP-SMA affects mindfulness/meditation/relaxation (25.7%), increases happiness/well-being (37.1%), leads to behavioural change (48.6%), and targets physical health (100%). Table 3 shows the participants' rating scores of the LBP-SMA quality. The objective quality rating scores of the LBP-SMA based on engagement, functionality, aesthetics and information was 17.1 ± 2.963, 18.5 ± 1.704, 17.6 ± 1.352 and 18.3 ± 1.804 respectively. The total App quality rating was 17.9 ± 1.471. The subjective rating score of the LBP-SMA was 18.4 ± 1.173 out of a total of 20.
Table 1: General and pain characteristics of all the participants (N = 35). View Table 1
Table 2: Participants perception of area of focus of the app using MARS. View Table 2
Table 3: Participants' app quality rating scores using MARS. View Table 3
User's knowledge, attitudes, intensions and behavioural change on the perceived impact of the LBP-SMA is presented in Table 4. From the result, LBP-SMA mostly led to increase rate of knowledge (77.0%), behavioural change (71.4%) and awareness (82.9%) on the importance of extension movement in LBP. The impact score of LBP-SMA on user's knowledge, attitudes, intensions and behavior change on importance of extension movement is presented in Table 5. The highest and the least scores were on awareness (4.8 ± 0.473) and help seeking (4.1 ± 0.845). The total impact score of the LBP-SMA was 27.2 ± 1.911 out of a total score of 30. The usability score of the LBP-SMA gave a mean score of 29.6 ± 1.95 out of a total of 50. The usability score of the LBP-SMA ranges from 24 to 33. The correlation between pain characteristics of the participants and the different rating scores of the LBP-SMA is presented in Table 6. There was no significant correlation between participants' pain characteristics and their app rating scores (r ranged from 0.000 to 0.350; p > 0.05).
Table 4: Perceived impact of the app on user's knowledge, attitudes, intensions and behavior change on importance of extension movement using MARS. View Table 4
Table 5: Impact score of app on user's knowledge, attitudes, intensions and behavior change on importance of extension movement. View Table 5
Table 6: Correlation between app rating scores and patients' pain characteristics. View Table 6
This study was aimed to develop and test the feasibility of a mobile phone-based application of the MDT and back hygiene in patients with long-term non-specific LBP. The participants in this study were patients with chronic non-specific LBP. These patients were relatively young with moderate pain intensity. After a minimum of seven days use of the LBP-SMA, the usability and rating of the app was assessed. From this study, the patients indicate that the LBP-SMA affect mindfulness/meditation/relaxation, increase happiness/well-being, leads to behavioural change as well as targets physical health. Few studies have conducted analyses of health and fitness apps [42,43] and app acceptability and utility [44-47]. The findings of this study support assertion that mobile phones may provide a unique means of administering health interventions to populations [48].
The findings of this study on the quality rating of the LBP-SMA based on engagement, functionality, aesthetics and information reveals high scores. The high quality rating of the LBP-SMA demonstrates the potential of using apps to change health behaviour and manage chronic LBP. These findings also reflect the larger societal trends wherein consumer acceptance and demand for health and fitness apps to change behavior is growing [49], which has resulted in increased profitability [50]. Most studies on health app for preventive purposes as well as management of chronic illnesses, though built on different structural platforms and functions, reported high user acceptability [51,52]. Only few studies, however, reported average and low-to-moderate acceptability [53,54]. Based on the trend observed in literature, the potential for technology-based health interventions to impact populations is possible like never before with respect to increase in mobile phone ownership and the number and complexity of health apps [48]. Thus, health apps have also become a part of global market with over 31,000 health and medical apps available for download [49].
The usability of the LBP-SMA was evaluated by considering willingness to use the app, level of complexity of app, ease of use, dependability on others to use app, integrated functionality of app, consistency of the app, time taken to use the app, cumbersomeness of the app, and confidence with the use of app. The usability score of the LBP-SMA range from moderate to high. The high usability rating observed in this study is consistent generally with users' rating of exercise and physical activity apps [55-57]. Ease of use, limited time per use, high acceptability of awareness raising, alerts to action, fastness, convenience of the app, and more automatic functions have been reported as the main acceptable features of health apps [47,58-61].
Furthermore, this study assessed the perceived impact of the LBP-SMA on user's knowledge, attitudes, intensions and behavior change on the importance of extension movement. The findings shows that the LBP-SMA led to improved knowledge, behavioural change and awareness on the importance of extension movement of the back in LBP. The total impact score of the LBP-SMA is 27.2 ± 1.911 out of a total score of 30. The finding of this study aligns with a systematic review's supposition that most health apps are efficacious at changing behavior [48]. However, Zhao, et al. [62] reported a lack of synthesized evidence regarding the effectiveness of mobile phone apps in changing people's health-related behaviors. Nonetheless, literature is increasing on studies on use of apps for exercise and physical activity. Most of the studies reported that health apps have significant health impacts [54,55].
Zhao, et al. [62] submits that globally, mobile phones have achieved wide reach at an unprecedented rate, and mobile phone apps have become increasingly prevalent among users. The number of health-related apps that were published on the two leading platforms (iOS and Android) reached more than 100,000 in 2014. Despite increasing use of health apps, generally, clinical trial evidence supporting the use of apps is generally lacking. Singh, et al. [63] explained the possible reasons in three ways. First, the health apps are fairly new as a medium for engaging patients in comparison with other digital media; therefore, research supporting their use may be ongoing but not yet published. If that is the case, evidence may be found in "gray literature" such as conference proceedings that has not yet made its way to peer-reviewed journals. Second, app developers may be participating in and using research findings to market their apps, which may favor obtaining lower-quality evidence because it is less costly and potentially biased toward a favorable result. Third, it is possible that high-quality evidence exists but that prior reviews failed to uncover it because they focused too narrowly on a small set of disease areas. However, there are limited known studies on management of chronic LBP using mobile health apps. As first step in the process of validation, this study tested the feasibility of LBP-SMA among patients with chronic LBP. Also, findings from this study show that there was no significant correlation between patients' pain characteristics and LBP-SMA rating scores. Thus, it is adducible that the findings of this study on the feasibility of the app are not influenced by pain characteristics of the patients. It is inferred that LBP-SMA will be usable by patients with LBP irrespective of their level and nature of pain.
It should be noted that the findings of this study may be limited by only recruiting existing smart-phone users, the young population cohort sampled, duration of testing only being 1 week, inclusion of only patients with a lumbar extension preference, and recruitment from only one clinical institution.
The low-back pain self-treatment app has moderate to high usability, functionality, aesthetics and quality rating, and may serve as an effective mobile app for self-management of chronic low-back pain.
The authors want to thank Mr. Babatope Oni and the team for helping develop the app. The panel of physiotherapists who advised on the app development and the patients that took part in the feasibility study are appreciated.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
This research was [partially] funded by an African Doctoral Dissertation Research Fellowship (ADDRF) re-entry grant awarded by the African Population and Health Research Center (APHRC) in partnership with the International Development Research Centre (IDRC).
CEM is the guarantor for this article.
CEM conceived this study. CEM, TMA and IPG were involved in the development of app, collection and analysis of data. All authors participated in literature review, drafting and review of the final manuscript.