Abstract
Several options are available to manage osteoarthritis of the knee including arthroscopic joint debridement, high tibial osteotomy, proximal fibula osteotomy, Maquet osteotomy, joint distraction procedure, sub-chondroplasty, injection of platelet rich plasma, injection of stem cell, patellofemoral arthroplasty, unicompartment knee arthroplasty, and total knee replacement. The choice of surgery will depend on location and severity of the osteoarthritis, age, comorbidities, and body mass index of the patient. The aim of this review is to provide an overview of the available surgical treatments for knee osteoarthritis.
Keywords
Knee, Arthroplasty, Osteotomy, Osteoarthritis
List of Abbreviations
BMI: Body Mass Index; OA: Osteoarthritis; OARSI: Osteoarthritis Research Society International; HTO: High Tibial Osteotomy; PRP: Platelet Rich Plasma; PFA: Patellofemoral Arthroplasty; UKA: Unicompartment Knee Replacement; ACL: Anterior Cruciate Ligament
Background
Osteoarthritis (OA) of the knee joint is an extremely common condition seen in our daily practice with reported prevalence of 30% in people over 60 years of age [1]. It is the fourth leading cause of disability the world-over [2,3].
The guideline for non-surgical management of OA was published in 2007 by OARSI (Osteoarthritis research society international), which have been refined based on systematic reviews [4]. There have been published pathways, evidence based guidelines and appropriate use criteria for surgical management of this condition [5-7].
But there are several surgical options not mentioned in these studies. The purpose of this article is to provide a comprehensive review of various surgical options available for management of knee OA.
The available options are broadly classified into four categories as mentioned in Table 1.
Table 1: Classification of surgical options for management of knee osteoarthritis. View Table 1
Arthroscopic Knee Surgery
It is one of the most controversial procedures performed for knee OA. It was thought to benefit patients by removing debris and cytokines along with wash [7]. However, randomized control trials did not show any benefit compared to placebo. The relief of symptoms may have been due to the natural course of the disease, effect of the co-interventions or a placebo effect [8-10].
Arthroscopic meniscectomy was found to be no better than sham surgery for degenerative meniscal tear [11]. British Medical Journal (BMJ) published clinical practice guidelines based on randomized controlled trials (RCT). They reported that there was only short term benefit in pain and function, and on the contrary it was possible for patients to develop thromboembolism (0.5%) and infection (0.2%). They strongly recommended against arthroscopic knee surgery in patients with degenerative knee disease [12].
Recommendation at present
There is no role for routine lavage or debridement for patients with radiographic OA. However, patients with clicking or locking may be offered this procedure for improvement in mechanical symptoms only along with possible associated risks.
High Tibial Osteotomy (HTO)
This procedure was described by Jackson in 1958 and popularized by Coventry [13,14]. There was loss of interest in the procedure subsequently, but with improved surgical techniques, better implants, and fixation techniques, a renewed interest has been found in this procedure [15-17]. It is recommended for physiologically young and active patients meeting the criteria mentioned in Table 2. Presence of advanced degenerative changes, inflammatory arthritis, and large areas of exposed bone are contraindications to the procedure [18]. The aim of this osteotomy is to over correct the mechanical alignment to 3-5 deg of valgus [14,19,20]. The correction can be achieved by either a lateral closing, medial opening or dome shaped osteotomy [21,22]. The required amount of wedge to be removed is determined pre-operatively using a technique described by Fujisawa [23]. The osteotomy can be fixed using a spacer plate (Puddu), Locked plate (Tomofix) or a dual sliding compression plate (Figure 1) [22,24]. Good or excellent results have been reported in 68% to 77% with a survival of 90% at 15 years [25]. It is recommended to start with arthroscopy and address the lateral compartment pathology.
 Figure 1: Medial opening osteotomy fixed by Tomofix plate.
View Figure 1
Figure 1: Medial opening osteotomy fixed by Tomofix plate.
View Figure 1
Table 2: Indications for high tibial osteotomy. View Table 2
Recommendation at present
There is limited available evidence to recommend HTO for treating pain from knee medial compartment OA.
Proximal Fibular Osteotomy
Fibula acts as a strut to load 1/6 body weight and prevents uniform settling of osteoporotic proximal tibia [26]. This contributes to increased stress on medial tibial plateau and development of varus osteotomy. Proximal fibular osteotomy redistributes the loading of tibial plateau and relieves pain (Figure 2) [26-28]. Only few short term studies are available [26,28,29]. The improvement in post-operative score depends upon inclination and OA of proximal tibiofibular joint, BMI and pre-operative knee function [28].
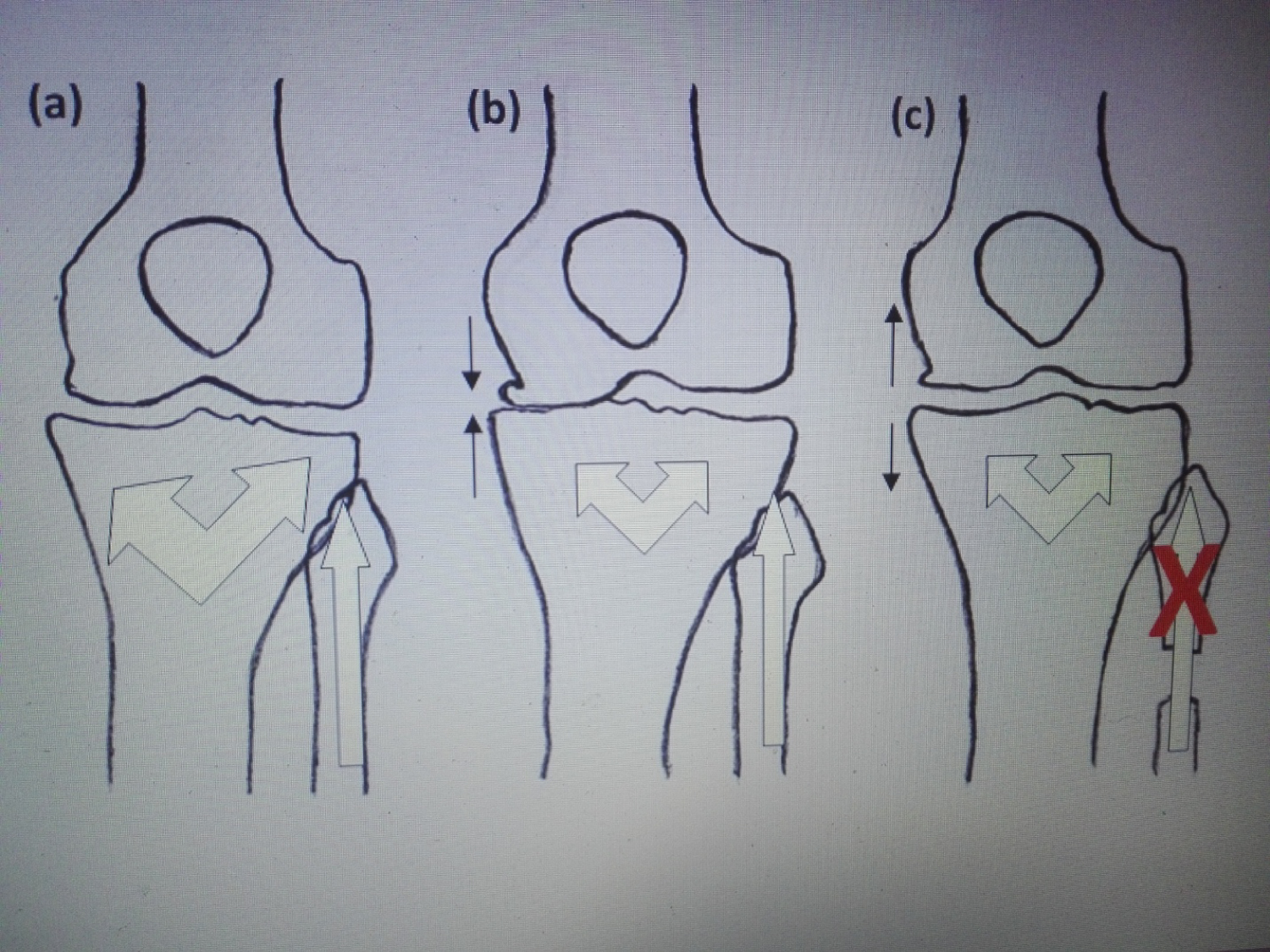 Figure 2: Schematic figure illustrating mechanism of PFO. (a) The proximal tibia and fibula structures resulted in equal load bearing capacity in medial and lateral sides of proximal tibia; (b) Varus deformity resulted from a decrease in proximal tibia trabecular bone mass. The proximal fibular load bearing capability is not affected; (c) PFO resulted in redistribution of the load bearing capacity of the proximal tibia, leading to correction of the alignment.
View Figure 2
Figure 2: Schematic figure illustrating mechanism of PFO. (a) The proximal tibia and fibula structures resulted in equal load bearing capacity in medial and lateral sides of proximal tibia; (b) Varus deformity resulted from a decrease in proximal tibia trabecular bone mass. The proximal fibular load bearing capability is not affected; (c) PFO resulted in redistribution of the load bearing capacity of the proximal tibia, leading to correction of the alignment.
View Figure 2
Maquet Osteotomy
First proposed by Maquet in 1963 and aimed to unload painful patellofemoral (PF) joint by tibial tubercle anteriorization [30,31]. Generally, patellofemoral pain from severe PF osteoarthritis not responding to non-operative treatment is the primary indication for this procedure.
The Maquet technique relieves anterior knee pain by decreasing contact load on the PF joint by elevating tibial tubercle [30-32]. A bone block, either autograft or allograft, inserted beneath the tibial tubercle to maintain crest elevation (Figure 3). It provides a good short and long term results in 80% of the cases [33,34]. Progressive anteriorization of the tibial crest is associated with progressive decrease in the PF compressive force [32]. However, only 1.5 to 2 cm of elevation is recommended as further elevation result in minimal compressive relief [35]. Reports of this procedure had good result; however, skin necrosis and graft nonunion are the main local complications seen with this technique [34].
 Figure 3: Maquet osteotomy performed for young patient with isolated patellofemoral osteoarthritis.
View Figure 3
Figure 3: Maquet osteotomy performed for young patient with isolated patellofemoral osteoarthritis.
View Figure 3
Knee Joint Distraction - Arthrodiastasis
It works on the principle of unloading of the medial tibial compartment. It was first described in 2010 as a case report and subsequently used for management of knee OA [36,37]. There was a study mentioning that the thickness of cartilage formed after this procedure was better than HTO [38]. A randomized control trial comparing knee joint distraction with HTO found no difference between the two techniques in regards to joint space widening and clinical outcome [39]. It may be considered as an alternate option for medial compartment OA in patients with minimal leg malalignment.
Recommendation at present
There is a lack of strong evidence on the efficacy of this procedure in treatment of knee OA. Well designed comparative trials in this subject are needed for evaluation of its benefit.
Sub-Chondroplasty
It is minimally invasive procedure described for knee OA patients with bone marrow edema (Figure 4). These patients have been shown to have accelerated progression to painful OA [40,41]. This technique involves fluoroscopic control and application of calcium sulphate based bone substitute. Early results (2-4 years) have shown relief in pain with improved structural quality and remodeling of bone [42-44]. Longer term studies and controlled trial are required before it can be included in the guidelines.
 Figure 4: Coronal T-2 MRI shows medial tibial subchondral oedema.
View Figure 4
Figure 4: Coronal T-2 MRI shows medial tibial subchondral oedema.
View Figure 4
Platelet Rich Plasma (PRP)
Concentrates obtained from blood releases various cytokines which help in cartilage regeneration and reducing synovial inflammation [45]. Early results (1 year) of PRP injection are better than Hyaluronic acid/placebo without any additional risks [46,47]. It is recommended to make shared decision with the patient [48].
Recommendation at present
There is inadequate evidence on the efficacy of this procedure in relieving OA knee pain. However, there is no known major harm of using PRP.
Stem Cell
Pleuripotent mesenchymal stem cells help in replacing lost cells. They release trophic factors which help to reduce inflammation and stabilize matrix [49]. Randomized control trials comparing stem cells injection with conservative treatment have shown improved function at 12 months and a lot of future studies are anticipated in this modality of treatment [50-53].
Patellofemoral Arthroplasty
Patellofemoral arthroplasty (PFA) introduced by Mackveer in 1955, but initial design was associated with poor functional results [54]. However the current modern design has produced good results and outcomes with ten years survivorship of more than 80% [55]. Patient selection, implant designs, and surgical technique are the main factors for achieving better outcome. The main indication for PFA is advanced isolated OA of knee joint in patient older than 40 who exhausted conservative managements [56,57].
The indications and contraindications for PFA are summarized in Table 3. Total knee replacement (TKR) with patellar replacement is the gold standard for treating advanced PFOA due to long term good result [58]. However, meta-analysis of 28 studies revealed comparable results in function and complications rate between TKR and modern generation PFA in short and mid-term results [59].
Table 3: Indications and contraindications for patellofemoral arthroplasty. View Table 3
Unicompartment Knee Arthroplasty
There has been more interest in this technique recently, although it was described initially in 1970 [60]. Medial compartment is more commonly involved and unicompartment knee arthroplasty (UKA) comprises 11% of total arthroplasty cases of knee joint (UK joint registry). It was classically indicated for elderly > 60 years low demand and thin patients (weight < 82 kg) [61]. The indications have been extended to younger patients by oxford group (Cite - oxford knee) as a result of better surgical technique, better prosthesis design and improved polywear [60-62]. Historically ACL deficient knees have shown early failure after UKA due to eccentric loading and polywear. Recent studies have divided ACL deficient knees into two subgroups; traumatic and degenerative. UKA should not be done in patients with traumatic, symptomatic ACL rupture. Although satisfactory results have been reported in these by combining ACL reconstruction with UKA [63,64]. The other group of patients with degenerative tear of ACL should have a posterior slope < 7 degrees [65].
UKA has been successful in middle aged patients with > 90% survival at 10 years, with excellent function (Figure 5) [66,67]. In comparison to total TKR, UKA provides faster rehabilitation and quick recovery, less morbidity, and less blood loss. It also preserves normal kinematics of the joint. This procedure should be avoided in conditions shown in Table 4.
 Figure 5: Unicompartment knee replacement- AP and lateral radiographs.
View Figure 5
Figure 5: Unicompartment knee replacement- AP and lateral radiographs.
View Figure 5
Table 4: Contraindications for unicompartment knee replacement. View Table 4
Total Knee Replacement
TKR is indicated for end stage OA (Figure 6). A 25 year survival rate of 82% has been reported (95% CT - 83-83.2) [68]. But despite this, one out of five patients are still not satisfied after surgery [69]. The aim of the procedure is to restore mechanical alignment, joint line, and achieve normal balanced ligaments with restored angle. The joint can be approached using either a medial parapatellar, mid vastus or subvastus approach. Better early outcomes were reported subvastus and midvastus approach but in long term there was no difference between two groups [70-72]. Coronal plane alignment is achieved by precise bone cuts, releasing of tight medial ligaments and tightening of lax lateral side. The saggital plane alignment is achieved by tackling tibia in symmetric gap mismatch and femur in asymmetric gap mismatch. There is no difference in clinical results between posterior cruciate retaining and stabilized implants [73,74]. The implant fixation (cemented/uncemented) bearing surface (mobile/fixed) and alignment has shown no difference in RCT [68]. It can be safely said that a conventional knee can be performed by an approach familiar to surgeon, using standard well established components, with or without tourniquet and without drains to achieve good long term results [68].
Conclusion
Surgical option should be considered to manage OA knees only after exhausting conservative options. The treatment offered should be modified based on patient age, demands and symptoms. HTO and UKA are considered in single compartment disease and total knee should be reserved for end stage disease. A realistic expectation should be offered to the patient based on available evidence to have a satisfied patient.
Declarations
Ethical consideration
This is a review article that does not involve patients or patient's information.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Authors' contributions
JSL conceived and designed the article's outlines and wrote the initial and final draft. SAH contributed with draft writing, organized and prepared the figures, and was the corresponding author. SUG: Reviewed the final manuscript.
All authors read and approved the final manuscript. All authors have critically reviewed and approved the final draft and are responsible for the manuscript's content and similarity index.
Statement of equal authors' contribution
All authors have contributed equally.
References
-
Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, et al. (1987) The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum 30: 914-918.
-
Mahir L, Belhaj K, Zahi S, Azanmasso H, Lmidmani F, et al. (2016) Impact of knee osteoarthritis on the quality of life. Ann Phys Rehabil Med 59: e159.
-
Nguyen U-SDT, Zhang Y, Zhu Y, Niu J, Zhang B, et al. (2011) Increasing prevalence of knee pain and symptomatic knee osteoarthritis: Survey and cohort data. Ann Intern Med 155: 725-732.
-
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, et al. (2019) OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage 27: 1578-1589.
-
Manner PA, Tubb CC, Levine BR (2018) AAOS appropriate use criteria: Surgical management of osteoarthritis of the knee. J Am Acad Orthop Surg 26: e194-e197.
-
(2014) Osteoarthritis: Care and management. NICE.
-
Aaron RK, Skolnick AH, Reinert SE, Ciombor DM (2006) Arthroscopic débridement for osteoarthritis of the knee. J Bone Joint Surg Am 88: 936-943.
-
Chang RW, Falconer J, Stulberg SD, Arnold WJ, Manheim LM, et al. (1993) A randomized, controlled trial of arthroscopic surgery versus closed-needle joint lavage for patients with osteoarthritis of the knee. Arthritis Rheum 36: 289-296.
-
Hubbard MJ (1996) Articular debridement versus washout for degeneration of the medial femoral condyle. A five-year study. J Bone Joint Surg Br 78: 217-219.
-
Dervin GF, Stiell IG, Rody K, Grabowski J (2003) Effect of arthroscopic débridement for osteoarthritis of the knee on health-related quality of life. J Bone Joint Surg Am 85: 10-19.
-
Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, et al. (2013) Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 369: 2515-2524.
-
Siemieniuk RAC, Harris IA, Agoritsas T, Poolman RW, Brignardello-Petersen R, et al. (2017) Arthroscopic surgery for degenerative knee arthritis and meniscal tears: A clinical practice guideline. BMJ 357: 1982.
-
Jackson JP, Waugh W (1961) Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br 43: 746-751.
-
Coventry MB (1973) Osteotomy about the knee for degenerative and rheumatoid arthritis. J Bone Joint Surg Am 55: 23-48.
-
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: A new LCP-concept for open wedge osteotomy of the medial proximal tibia--early results in 92 cases. Injury 34: 55-62.
-
Sommer C, Gautier E, Müller M, Helfet DL, Wagner M (2003) First clinical results of the Locking Compression Plate (LCP). Injury 34: 43-54.
-
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11: 132-138.
-
Brinkman JM, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, et al. (2008) Osteotomies around the knee: Patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 90: 1548-1557.
-
Hernigou P, Medevielle D, Debeyre J, Goutallier D (1987) Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am 69: 332-354.
-
Myrnerts R (1980) Optimal correction in high tibial osteotomy for varus deformity. Acta Orthop Scand 51: 689-694.
-
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10: 585-608.
-
Liu X, Chen Z, Gao Y, Zhang J, Jin Z (2019) High tibial osteotomy: Review of techniques and biomechanics. J Healthc Eng 2019: 8363128.
-
Polat G, Balcı Hİ, Çakmak MF, Demirel M, Şen C, et al. (2017) Long-term results and comparison of the three different high tibial osteotomy and fixation techniques in medial compartment arthrosis. J Orthop Surg 12: 44.
-
hrefLobenhoffer P, Agneskirchner JD (2012) Technique of open wedge HTO. In: The Knee Joint. Springer, Paris.
-
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy: A ten- to 20-year follow-up. J Bone Joint Surg Br 90: 592-596.
-
Baldini T, Roberts J, Hao J, Hunt K, Dayton M, et al. (2018) Medial compartment decompression by proximal fibular osteotomy: A biomechanical cadaver study. Orthopedics 41: e496-e501.
-
Wang X, Wei L, Lv Z, Zhao B, Duan Z, et al. (2017) Proximal fibular osteotomy: A new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res 45: 282-289.
-
Qin D, Chen W, Wang J, Lv H, Ma W, Dong T, et al. (2018) Mechanism and influencing factors of proximal fibular osteotomy for treatment of medial compartment knee osteoarthritis: A prospective study. J Int Med Res 46: 3114-3123.
-
Liu B, Chen W, Zhang Q, Yan X, Zhang F, et al. (2018) Proximal fibular osteotomy to treat medial compartment knee osteoarthritis: Preoperational factors for short-term prognosis. PLoS One 13: e0197980.
-
Maquet P (1979) Mechanics and osteoarthritis of the patellofemoral joint. Clin Orthop Relat Res 70-73.
-
Maquet P (1976) Advancement of the tibial tuberosity. Clin Orthop Relat Res 225-230.
-
Ferguson AB, Brown TD, Fu FH, Rutkowski R (1979) Relief of patellofemoral contact stress by anterior displacement of the tibial tubercle. J Bone Joint Surg Am 61: 159-166.
-
Schmid F (1993) The Maquet procedure in the treatment of patellofemoral osteoarthrosis. Long-term results. Clin Orthop 294: 254-258.
-
Mendes DG, Soudry M, Iusim M (1987) Clinical assessment of Maquet tibial tuberosity advancement. Clin Orthop Relat Res 228-238.
-
Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J, et al. (2014) Tibial tuberosity osteotomy: Indications, techniques, and outcomes. Am J Sports Med 42: 2006-2017.
-
Abouheif MM, Nakamura M, Deie M, Adachi N, Nishimori M, et al. (2010) Repair of a large osteochondral defect in the knee joint using autologous and artificial bone graft combined with motion preserving distraction arthroplasty: A case report. Arch Orthop Trauma Surg 130: 231-236.
-
Aly TA, Hafez K, Amin O (2011) Arthrodiatasis for management of knee osteoarthritis. Orthopedics 34: e338-e343.
-
hrefJansen M, Maschek S, Heerwaarden R, Mastbergen S, Wirth W, et al. (2019) Knee joint distraction is more efficient in rebuilding cartilage thickness in the more affected compartment than high tibial osteotomy in patients with knee osteoarthritis.
-
van der Woude JD, Wiegant K, van Heerwaarden RJ, Spruijt S, van Roermund PM, et al. (2017) Knee joint distraction compared with high tibial osteotomy: A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 25: 876-886.
-
Agten CA, Kaplan DJ, Jazrawi LM, Burke CJ (2016) Subchondroplasty: What the radiologist needs to know. AJR Am J Roentgenol 207: 1257-1262.
-
Cohen S, Sharkey P (2012) Surgical treatment of osteoarthritis pain related to subchondral bone defects or bone marrow lesions: Subchondroplasty. Tech Knee Surg 11: 170-175.
-
hrefChua K, Kang JYB, Ng FDJ, Pang HN, Lie DTT, et al. (2019) Subchondroplasty for bone marrow lesions in the arthritic knee results in pain relief and improvement in function. J Knee Surg.
-
Davis AT, Byrd JM, Zenner JA, Frank DA, DeMeo PJ, et al. (2015) Short-term outcomes of the subchondroplasty procedure for the treatment of bone marrow edema lesions in patients with knee osteoarthritis. Orthop J Sports Med 3: 2325967115S00125.
-
hrefCohen SB, Sharkey PF (2016) Subchondroplasty for treating bone marrow lesions. J Knee Surg 29: 555-563.
-
Milano G, Deriu L, Sanna Passino E, Masala G, Manunta A, et al. (2012) Repeated platelet concentrate injections enhance reparative response of microfractures in the treatment of chondral defects of the knee: An experimental study in an animal model. Arthroscopy 28: 688-701.
-
Chen P, Huang L, Ma Y, Zhang D, Zhang X, et al. (2019) Intra-articular platelet-rich plasma injection for knee osteoarthritis: A summary of meta-analyses. J Orthop Surg Res 14: 385.
-
Gato-Calvo L, Magalhaes J, Ruiz-Romero C, Blanco FJ, Burguera EF (2019) Platelet-rich plasma in osteoarthritis treatment: review of current evidence. Ther Adv Chronic Dis 10: 2040622319825567.
-
(2019) Platelet-rich plasma injections for knee osteoarthritis. NICE.
-
Shariatzadeh M, Song J, Wilson SL (2019) The efficacy of different sources of mesenchymal stem cells for the treatment of knee osteoarthritis. Cell Tissue Res 378: 399-410.
-
Lu L, Dai C, Zhang Z, Du H, Li S, et al. (2019) Treatment of knee osteoarthritis with intra-articular injection of autologous adipose-derived mesenchymal progenitor cells: A prospective, randomized, double-blind, active-controlled, phase IIb clinical trial. Stem Cell Res Ther 10: 143.
-
Freitag J, Bates D, Wickham J, Shah K, Huguenin L, et al. (2019) Evaulation of intra-articular adipose derived mesenchymal stem cell therapy in the treatment of symptomatic knee osteoarthritis - a randomised controlled trial. Cytotherapy 21: S69.
-
Doyle EC, Wragg NM, Wilson SL (2020) Intraarticular injection of bone marrow-derived mesenchymal stem cells enhances regeneration in knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc.
-
Freitag J, Bates D, Wickham J, Shah K, Huguenin L, et al. (2019) Adipose-derived mesenchymal stem cell therapy in the treatment of knee osteoarthritis: A randomized controlled trial. Regen Med 14: 213-230.
-
Levitt RL (1973) A long-term evaluation of patellar prostheses. Clin Orthop 153-157.
-
van der List JP, Chawla H, Villa JC, Pearle AD (2017) Why do patellofemoral arthroplasties fail today? A systematic review. The Knee 24: 2-8.
-
Delanois RE, McGrath MS, Ulrich SD, Marker DR, Seyler TM, et al. (2008) Results of total knee replacement for isolated patellofemoral arthritis: when not to perform a patellofemoral arthroplasty. Orthop Clin North Am 39: 381-388.
-
Leadbetter WB, Ragland PS, Mont MA (2005) The appropriate use of patellofemoral arthroplasty: An analysis of reported indications, contraindications, and failures. Clin Orthop Relat Res 91-99.
-
Clement ND, Howard TA, Immelman RJ, MacDonald D, Patton JT, et al. (2019) Patellofemoral arthroplasty versus total knee arthroplasty for patients with patellofemoral osteoarthritis. Bone Jt J 101: 41-46.
-
Dy CJ, Franco N, Ma Y, Mazumdar M, McCarthy MM, et al. (2012) Complications after patello-femoral versus total knee replacement in the treatment of isolated patello-femoral osteoarthritis. A meta-analysis. Knee Surg Sports Traumatol Arthrosc 20: 2174-2190.
-
hrefBorus T, Thornhill T (2008) Unicompartmental knee arthroplasty. J Am Acad Orthop Surg 16: 9-18.
-
hrefKozinn SC, Scott R (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71: 145-150.
-
Pandit H, Jenkins C, Barker K, Dodd C, Murray DW (2006) The Oxford medial unicompartmental knee replacement using a minimally-invasive approach. J Bone Joint Surg Br 88: 54-60.
-
Tian S, Wang B, Wang Y, Ha C, Liu L, et al. (2016) Combined unicompartmental knee arthroplasty and anterior cruciate ligament reconstruction in knees with osteoarthritis and deficient anterior cruciate ligament. BMC Musculoskelet Disord 17: 327.
-
hrefVolpin A, Kini SG, Meuffels DE (2018) Satisfactory outcomes following combined unicompartmental knee replacement and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 26: 2594-2601.
-
Hernigou P, Deschamps G (2004) Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty. J Bone Joint Surg Am 86: 506-511.
-
Kim KT, Lee S, Lee JS, Kang MS, Koo KH (2018) Long-term clinical results of unicompartmental knee arthroplasty in patients younger than 60 years of age: Minimum 10-year follow-up. Knee Surg Relat Res 30: 28-33.
-
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2003) Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am 85: 1968-1973.
-
Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, et al. (2019) How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet Lond Engl 393: 655-663.
-
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop 468: 57-63.
-
hrefDutton AQ, Yeo S-J, Yang K-Y, Lo N-N, Chia K-U, et al. (2008) Computer-assisted minimally invasive total knee arthroplasty compared with standard total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am 90: 2-9.
-
Roysam GS, Oakley MJ (2001) Subvastus approach for total knee arthroplasty: A prospective, randomized, and observer-blinded trial. J Arthroplasty 16: 454-457.
-
Bäthis H, Perlick L, Blum C, Lüring C, Perlick C, et al. (2005) Midvastus approach in total knee arthroplasty: A randomized, double-blinded study on early rehabilitation. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 13: 545-550.
-
Baumgarten KM, Chang PS, Looby PA, McKenzie MJ, Rothrock CP (2019) Do more expensive total knee arthroplasty prostheses provide greater improvements in outcomes over less expensive prostheses sold by a physician-owned distributorship? J Am Acad Orthop Surg 27: e1059-e1067.
-
Meijerink HJ, Verdonschot N, van Loon CJ, Hannink G, de WaalMalefijt MC (2011) Similar TKA designs with differences in clinical outcome. Acta Orthop 82: 685-691.
Citation
Luthra JS, AL Habsi S, AL Ghannami S (2020) Surgical Options for Treating Knee Osteoarthritis - A Concise Review. J Musculoskelet Disord Treat 6:084. doi.org/10.23937/2572-3243.1510084
 Figure 1: Medial opening osteotomy fixed by Tomofix plate.
View Figure 1
Figure 1: Medial opening osteotomy fixed by Tomofix plate.
View Figure 1
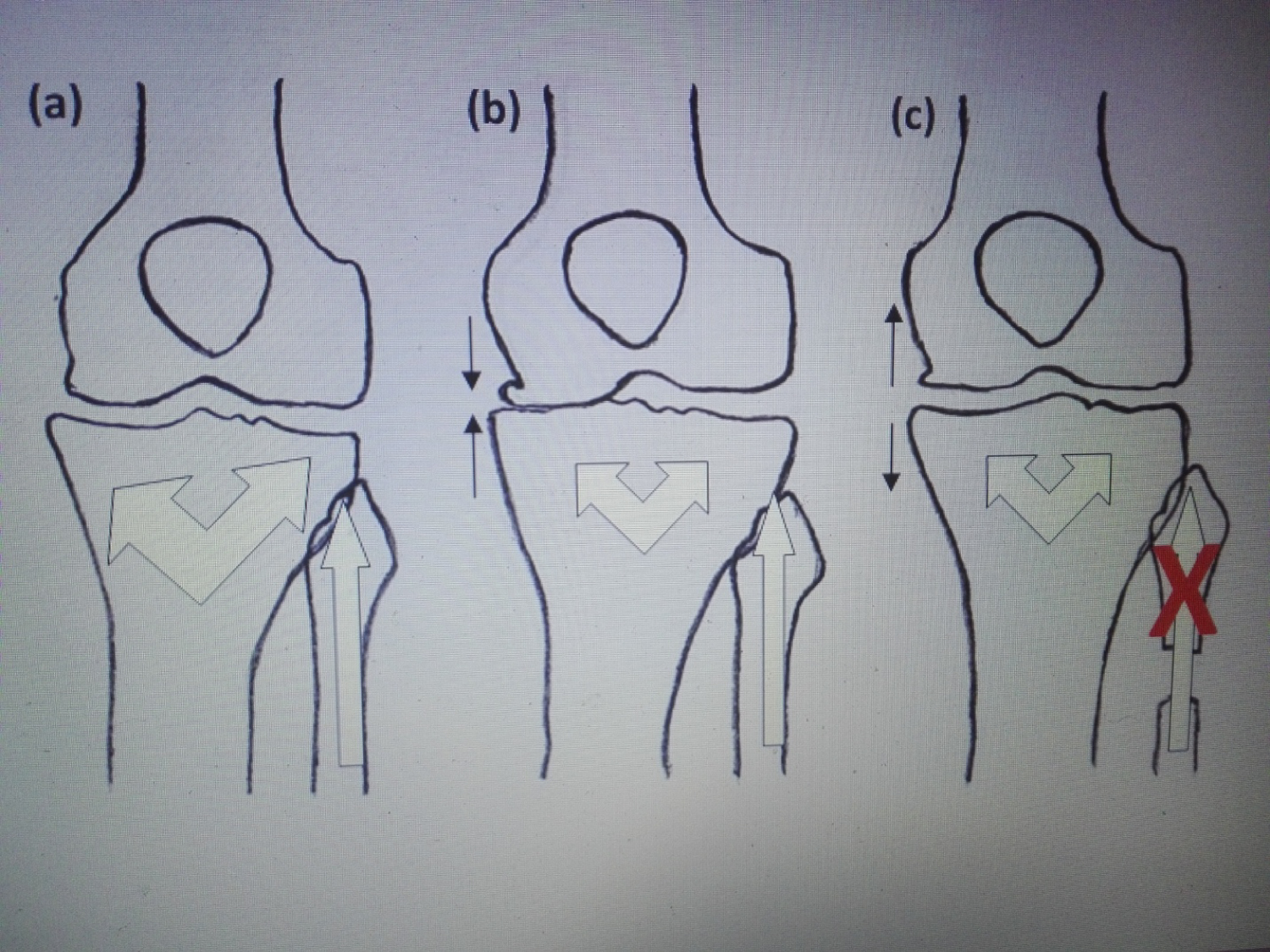 Figure 2: Schematic figure illustrating mechanism of PFO. (a) The proximal tibia and fibula structures resulted in equal load bearing capacity in medial and lateral sides of proximal tibia; (b) Varus deformity resulted from a decrease in proximal tibia trabecular bone mass. The proximal fibular load bearing capability is not affected; (c) PFO resulted in redistribution of the load bearing capacity of the proximal tibia, leading to correction of the alignment.
View Figure 2
Figure 2: Schematic figure illustrating mechanism of PFO. (a) The proximal tibia and fibula structures resulted in equal load bearing capacity in medial and lateral sides of proximal tibia; (b) Varus deformity resulted from a decrease in proximal tibia trabecular bone mass. The proximal fibular load bearing capability is not affected; (c) PFO resulted in redistribution of the load bearing capacity of the proximal tibia, leading to correction of the alignment.
View Figure 2
 Figure 3: Maquet osteotomy performed for young patient with isolated patellofemoral osteoarthritis.
View Figure 3
Figure 3: Maquet osteotomy performed for young patient with isolated patellofemoral osteoarthritis.
View Figure 3
 Figure 4: Coronal T-2 MRI shows medial tibial subchondral oedema.
View Figure 4
Figure 4: Coronal T-2 MRI shows medial tibial subchondral oedema.
View Figure 4
 Figure 5: Unicompartment knee replacement- AP and lateral radiographs.
View Figure 5
Figure 5: Unicompartment knee replacement- AP and lateral radiographs.
View Figure 5
 Figure 6: Total knee replacement- AP radiograph.
View Figure 6
Figure 6: Total knee replacement- AP radiograph.
View Figure 6